Spinal shock is an acute physiological loss or depression of spinal cord function following a spinal cord injury.
When the spinal cord is suddenly severed, all the fundamental functions of the cord below the level of injury including the spinal cord reflexes are immediately depressed, which is referred to as spinal shock. It can start from 30 minutes post-injury. Spinal shock does not resolve abruptly but rather in a series of phases extending over days to weeks to months, and spinal shock slowly transitions to spasticity. Neurological deficit cannot be evaluated until spinal shock has been resolved.
There continues to be a lack of consensus on the clinical symptomatology that defines the duration of spinal shock. Some clinicians interpret spinal shock as ending with the appearance of the bulbocavernosus reflex within the first few days of injury. Others state that it ends with the recovery of deep tendon reflexes (DTRs) which may not reappear for several weeks, and other clinicians define the resolution of spinal shock as the return of reflexive detrusor function which can happen months following injury.
Flaccid motor paralysis, a loss of all sensorimotor functions below the level of injury, areflexia/hyporeflexia and autonomic dysfunction are signs of spinal shock.
Stages of spinal shock: Spinal shock follows a predictable, stereotypical patterns.
This progression includes the following 4 phases:
1. Initial hyporeflexia (0 to 1 days)
2. Initial return of some reflexes (1 to 3 days)
Polysynaptic reflexes (those that require a signal to travel from a sensory neuron to a motor neuron) tend to return first. The delayed plantar reflex, a variation of the normal plantar reflex common among SCI survivors, typically returns first. Next is the bulbocavernosus reflex, which causes the anal sphincter to tighten in response to squeezing the clitoris or head of the penis.
3. Early hyperreflexia (4 days to 4 weeks) Hyperreflexia, a pattern of unusually strong reflexes. This is the result of new nerve synapse growth, and is normally temporary
4. Late hyperreflexia (1 to 12 months) Hyperreflexia continues, and spasticity may develop. This process is due to changes in the neuronal cell bodies.
Typical recovery:
• Vasovagal hypotension and bradycardia generally improve within 3 to 6 weeks
• Orthostatic hypotension may take 10 to 12 weeks to disappear.
• Bladder recovery may take from 4–6 weeks.
Autonomic dysreflexia is permanent and occurs from Phase 4 onwards.
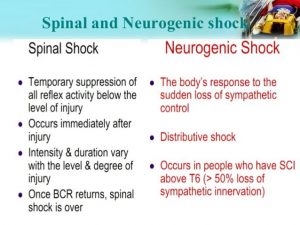
Spinal shock is often confused with neurogenic shock.
Spinal shock refers to loss of all sensation below the level of injury and is not circulatory in nature.
Neurogenic shock describes the hemodynamic changes resulting from a sudden loss of autonomic tone due to spinal cord injury. It is commonly seen when the level of the injury is above T6. Neurogenic shock is a type of distributive shock, consisting of the hemodynamic triad of hypotension, bradycardia, and peripheral vasodilatation (hypothermia), attributed to severe central nervous system damage (head trauma, cervical cord trauma, or high thoracic cord injuries), resulting in loss of sympathetic stimulation to the blood vessels and unopposed vagal activity. Neurogenic shock can persist for 1–6 weeks after the injury.
Both spinal and neurogenic shock can coexist in a patient.
The bulbocavernosus reflex (BCR) is spinal mediated and involves S2-S4.
It is a somatic reflex, mediated through the pudendal nerve, which elicits the contraction of the bulbocavernosus muscle in response to squeezing the glans penis/tugging on the indwelling Foley catheter or clitoris. Contractions of bulbocavernosus muscles and/or external anal sphincter are monitored in response to this squeezing of the glans penis or clitoris.
The BR is one of the few ways to test the conus medullaris (distal end of the spinal cord) and the S2 to S4 pelvic nerves. In the clinical evaluation of the spinal cord injury, the BR is fundamentally important because it signifies the end of spinal shock, as well as allows the classification of the spinal cord injury (complete and incomplete).
If the BR is present 48 hours following injury, it can be assumed that the patient is out of spinal cord shock. Patients must therefore have recovered from spinal shock (bulbocavernosus reflex is intact) before an injury can be determined as complete. Lack of motor and sensory function after the reflex has returned indicates complete SCI.
Interpretation of BR test:
• Bulbocavernosus Reflex absent- Spinal Shock
• Bulbocavernosus Reflex present- Severed spinal cord (lesion or injury of the conus medullaris or sacral nerve roots).
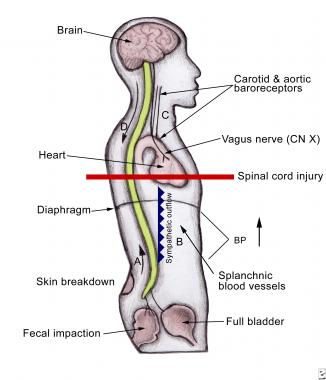 Autonomic dysreflexia (AD) develops in individuals with a spinal cord injury at or above the sixth thoracic vertebral level (T6).
Autonomic dysreflexia (AD) develops in individuals with a spinal cord injury at or above the sixth thoracic vertebral level (T6).
It is considered a medical emergency and must be recognized immediately.
What happens during an episode of AD
Autonomic dysreflexia indicates over-activity of the autonomic nervous system.
A noxious stimulus (would be painful if one could sense it) below the injury level sends nerve impulses to the spinal cord; they travel upward until blocked at the level of injury. Since these impulses cannot reach the brain, the body doesn’t respond as it would normally. A reflex is activated that increases activity of the sympathetic portion of the autonomic nervous system. This results in a narrowing of the blood vessels, which causes a rise in blood pressure.
Nerve receptors in the heart and blood vessels detect this rise in blood pressure and send a message to the brain. The brain then sends a message to the heart, causing the heartbeat to slow down and the blood vessels above the level of injury to dilate. However, since the brain is not able to send messages below the level of injury, blood pressure cannot be regulated. The body is confused and can’t sort out the situation.
For most people, AD can be easily treated as well as prevented. The key is for the patient to know and to inform their caregivers about their baseline blood pressure, triggers, and symptoms. It is therefore important for at-risk individuals to know their baseline blood pressure values.
Causes
Essentially, any painful, irritating, or even strong stimulus below the level of the injury can cause an episode of autonomic dysreflexia including:
1. Bladder: irritation of the bladder wall, urinary tract infection, blocked catheter or overfilled collection bag.
2. Bowel: distended or irritated bowel, constipation or impaction, hemorrhoids or anal infections.
3. Other causes: tight or restrictive clothing, skin infection or irritation, cuts, bruises, abrasions or pressure sores (decubitus ulcers), ingrown toenails, burns (including sunburn and burns from hot water), sexual activity, menstrual cramps, labor and delivery, ovarian cysts, abdominal conditions (gastric ulcer, colitis, peritonitis) or bone fractures.
When triggered, AD requires quick and correct action or there may be serious consequences such as a stroke.
Signs
• High blood pressure
• Pounding headache
• Flushed face
• Sweating above the level of injury
• Goose bumps below the level of injury
• Nasal stuffiness
• Nausea
• Slow pulse (slower than 60 beats per minute).
What to do when AD is triggered
1. The first step of treatment, regardless of the cause, is to sit the patient upright, thus producing an orthostatic decrease in blood pressure.
• Sit the patient up or raise their head to 90 degrees.
• Lower their legs if possible.
This will help lower BP while cause is identified.
2. The next step in managing acute AD must be to loosen any tight clothing and/or constrictive devices / splints / braces-especially around torso and quickly check catheter for blockages.
3. Closely monitor BP. Attach intermittent BP device and check BP every 5 minutes or more if needed. This will allow you to identify whether or not you have identified the problem. It is critical that blood pressure is checked at least every 5 minutes throughout the episode of AD, until the individual is stable.
An individual with SCI above T6 often has a normal systolic blood pressure in the 90-110 mm Hg range. A blood pressure reading of 20mm to 40mm Hg above their baseline may be a sign of autonomic dysreflexia.
4. Search for and eliminate the precipitating stimulus. This involves careful inspection to identify the source of painful stimuli.
Begin by looking for the most common causes: bladder distention or bowel impaction are the most common.
• Bladder. Check bladder drainage equipment for kinks or other causes of obstruction to flow
• Bowel
• Skin issues
A less common cause of AD during therapy sessions may originate with muscle stretching, either from range-of-motion or passive stretching.
Remember: “The Five B’s”
Bed Up
BP
Bladder
Bowels
Body
Role of the OT – prevention and management
The OT has an important role to educate the patient and family members about autonomic dysreflexia and ensure that they are familiar with prevention strategies, signs and symptoms, and proper management of the condition.
OT Intervention – principles of management
Throughout the therapy sessions, the therapist needs to monitor the urinary catheter for any blockage or twisting. If the patient develops autonomic dysreflexia, the therapist needs to treat it as a medical emergency and be familiar with established protocols for medical management within his or her particular setting. The individual therapy session must be immediately discontinued to allow the patient to stabilize and recover.
References:
https://pmj.bmj.com/content/81/954/232/
https://www.christopherreeve.org/living-with-paralysis/health/secondary-conditions/autonomic-dysreflexia
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3108991/
http://www.wheelessonline.com/ortho/spinal_shock https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6218357/
https://www.sciencedirect.com/topics/neuroscience/neurogenic-shock
https://www.nature.com/articles/3101603