Pressure Ulcer

Bedsores, also called pressure ulcers and decubitus ulcers, are injuries to skin and underlying tissue resulting from prolonged pressure on the skin. Bedsores most often develop on skin that covers bony areas of the body, such as the heels, ankles, hips and coccyx.
People most at risk have medical conditions that limit their ability to change positions or cause them to spend most of their time in a bed or chair. Bedsores can develop over hours or days. Most sores heal with treatment, but some never heal completely. You can take steps to help prevent bedsores and help them heal.
Warning Signs of Bedsores or Pressure Ulcers
• Unusual changes in skin color or texture
• Swelling
• Pus-like draining
• An area of skin that feels cooler or warmer to the touch than other areas
• Tender areas
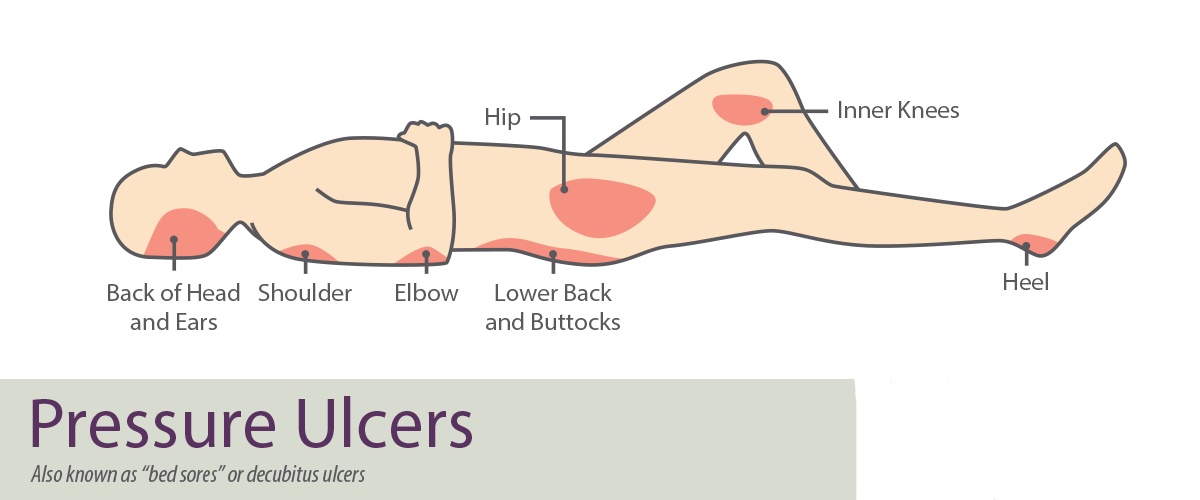
Common Sites for Pressure Ulcers
For people who use wheelchairs, bedsores often occur on skin over the following sites:
• Coccyx or buttocks
• Shoulder blades and spine
• Backs of arms and legs where they rest against the chair
For people who need to stay in bed, bedsores may happen on:
• The back or sides of the head
• The shoulder blades
• The hip, lower back or coccyx
• The heels, ankles and skin behind the knees
Causes
Bedsores are caused by pressure against the skin that limits blood flow to the skin. Limited movement can make skin vulnerable to damage and lead to development of bedsores.
Three primary contributing factors for bedsores:
• Pressure. Constant pressure on any part of the patient body can lessen the blood flow to tissues. Blood flow is essential for delivering oxygen and other nutrients to tissues. Without these essential nutrients, skin and nearby tissues are damaged and might eventually die.
For people with limited mobility, this kind of pressure tends to happen in areas that aren’t well padded with muscle or fat and that lie over a bone, such as the spine, coccyx, shoulder blades, hips, heels and elbows.
• Friction. Friction occurs when the skin rubs against clothing or bedding. It can make fragile skin more vulnerable to injury, especially if the skin is also moist.
• Shear. Shear occurs when two surfaces move in the opposite direction. For example, when a bed is elevated at the head, you can slide down in bed. As the coccyx moves down, the skin over the bone might stay in place — essentially pulling in the opposite direction.
Risk Factors
The patient risk of developing bedsores is higher if you have difficulty moving and can’t change position easily while seated or in bed.
Risk factors include:
• Immobility. This might be due to poor health, spinal cord injury and other causes.
• Incontinence. Skin becomes more vulnerable with extended exposure to urine and stool.
• Lack of sensory perception. Spinal cord injuries, neurological disorders and other conditions can result in a loss of sensation. An inability to feel pain or discomfort can result in not being aware of warning signs and the need to change position.
• Poor nutrition and hydration. People need enough fluids, calories, protein, vitamins and minerals in their daily diets to maintain healthy skin and prevent the breakdown of tissues.
• Medical conditions affecting blood flow. Health problems that can affect blood flow, such as diabetes and vascular disease, can increase the risk of tissue damage such as bedsores.
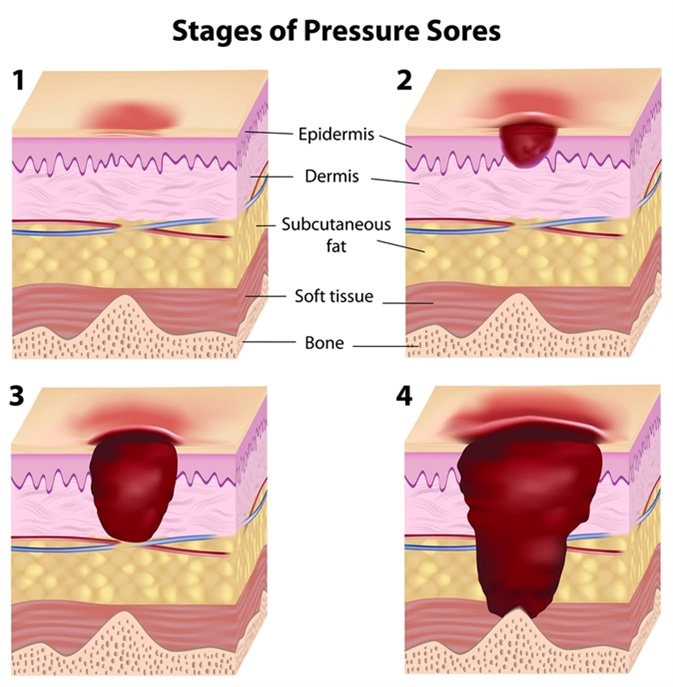
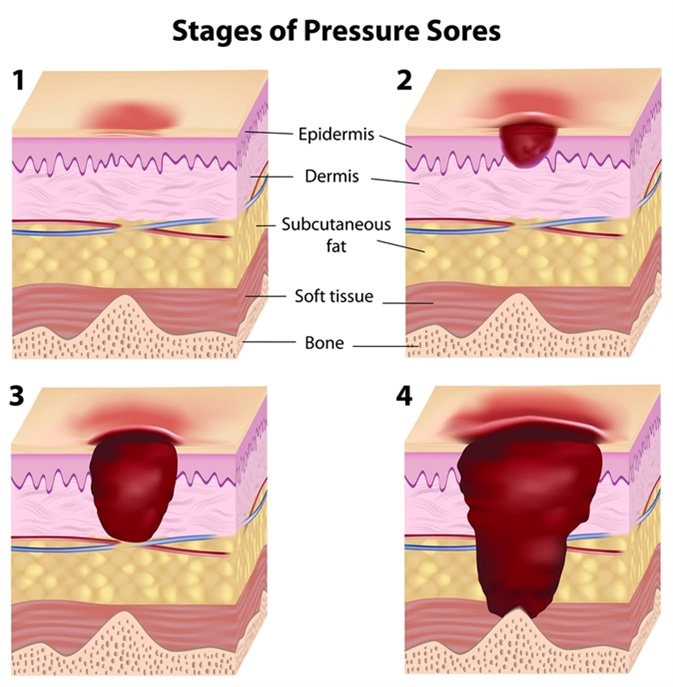
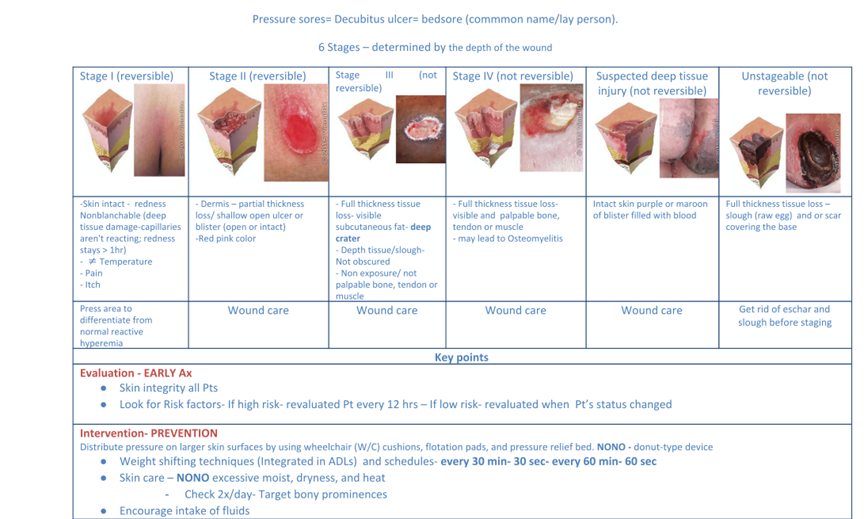
Stages
Pressure ulcers are categorized by the National Pressure Ulcer Advisory Panel into four stages based on the degree of tissue involvement or the depth of the sore.
The tissue layers can be broken down as: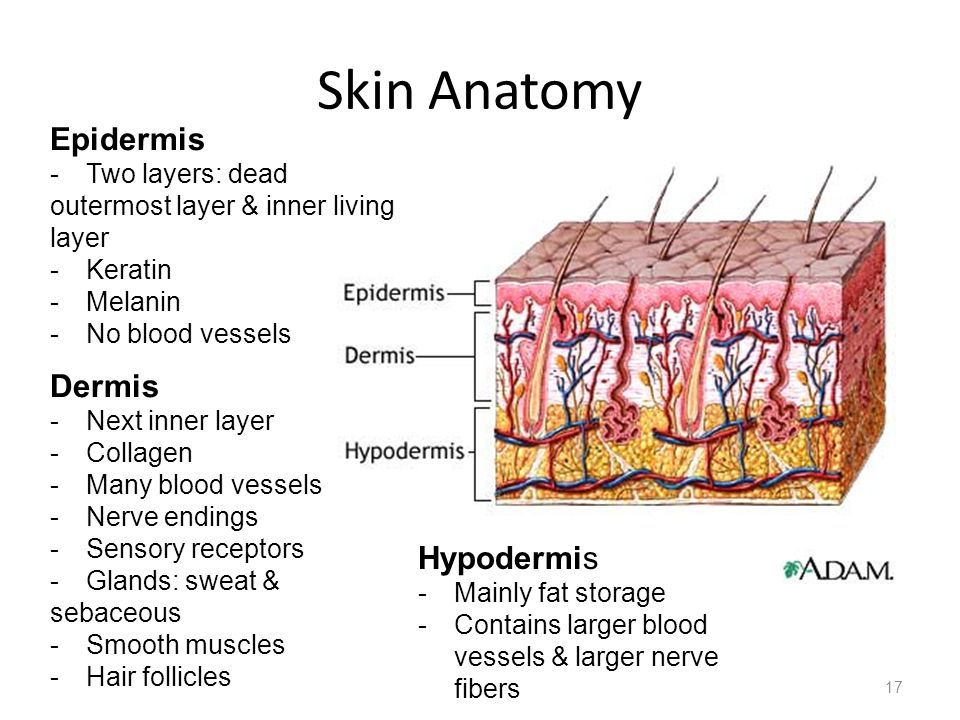
1. Epidermis (the outermost layer of skin)
2. Dermis (the second layer of skin)
3. Hypodermis (the lower layer of skin made up of fat and connective tissues)
4. Fascia (the layer of soft connective tissue below the skin that encloses muscles, nerves, blood vessels, and internal organs)
Stage One
Stage one ulcers are characterized by the superficial reddening of intact skin that does not blanch when pressed. The skin may be warm to the touch and either feel firmer or softer than the surrounding skin. People with darker skin may experience visible discoloration.
Edema (tissue swelling) and induration (the hardening of tissues) may be indications of a stage one pressure ulcer. If the pressure is not removed, a stage one pressure ulcer can progress to stage two. If diagnosed and treated immediately, a stage one pressure ulcer can usually resolve within three to four days.
Stage Two
Stage two ulcers are diagnosed when intact skin suddenly breaks open, exposing the epidermis and sometimes the dermis. The lesion will be superficial and often resemble an abrasion, popped blister, or shallow crater of skin. Stage two pressure ulcers will usually be red and warm to the touch. There may also be clear fluid in the broken skin.
To prevent progression to stage three, every effort must be made to pad the sore and alter the body’s position frequently. If treated properly, a stage two pressure ulcer can take anywhere from four days to three weeks to resolve.
Stage Three
Stage three ulcers are characterized by a lesion that extends well into the dermis and begins to involve the hypodermis (also known as the subcutaneous layer). By this stage, the lesion will form a small crater. Fat may begin to show in the open sore but not muscle, tendon, or bone. In some cases, there may be visible pus and a foul smell.
This type of ulcer opens the body to infection and leads to serious complications, including osteomyelitis (a bone infection) and sepsis (caused by an infection entering the bloodstream). With aggressive and sustained treatment, a stage three pressure ulcer can resolve in one to four months depending on its size and depth.
Stage Four
Stage four pressure ulcers occur when the hypodermis and underlying fascia are breached, exposing muscle and bone. This is the most severe type of pressure ulcer and the most difficult to treat. Damage to deeper tissues, tendons, nerves, and joints may occur, usually with copious amounts of pus and drainage.
Stage four pressure ulcers require aggressive treatment to avoid systemic infection and other potentially life-threatening complications. Even with effective treatment in a care facility, a stage four pressure ulcer can take two to six months (or even longer) to heal.
Suspected Deep Tissue Injury (SDTI). Some pressure ulcers may appear on first glance to be stage one or stage two, but the underlying tissues may be more extensively damaged. In this case, the ulcer may be classified as stage one with a suspected deep tissue injury. Upon further examination, an SDTI can sometimes turn out to be a stage three or four pressure ulcer.
Complications
Complications of pressure ulcers, some life-threatening, include:
• Cellulitis. Cellulitis is an infection of the skin and connected soft tissues. It can cause warmth, redness and swelling of the affected area. People with nerve damage often do not feel pain in the area affected by cellulitis.
• Bone and joint infections. An infection from a pressure sore can burrow into joints and bones. Joint infections (septic arthritis) can damage cartilage and tissue. Bone infections (osteomyelitis) can reduce the function of joints and limbs.
• Cancer. Long-term, nonhealing wounds (Marjolin’s ulcers) can develop into a type of squamous cell carcinoma.
• Sepsis. Rarely, a skin ulcer leads to sepsis.
Prevention
You can help prevent bedsores by frequently repositioning the patient to avoid stress on the skin. Other strategies include taking good care of the patient skin, maintaining good nutrition and fluid intake, quitting smoking, managing stress, and exercising daily.
Tips for skin care
• Keep skin clean and dry. Wash the skin with a gentle cleanser and pat dry. Do this cleansing routine regularly to limit the skin’s exposure to moisture, urine and stool.
• Protect the skin. Use moisture barrier creams to protect the skin from urine and stool. Change bedding and clothing frequently if needed. Watch for buttons on the clothing and wrinkles in the bedding that irritate the skin.
• Inspect the skin daily. Look closely at the patient skin daily for warning signs of a pressure sore.

Resources:
https://www.mayoclinic.org/diseases-conditions/bed-sores/symptoms-causes/syc-20355893
https://www.verywellhealth.com/stages-of-pressure-ulcers-2696692