
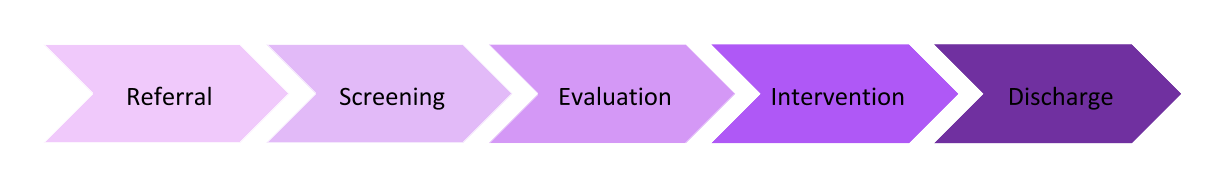
 The provision of occupational therapy services follows a specific sequence of steps.
The provision of occupational therapy services follows a specific sequence of steps.| Step in the Process | Description | Who is Involved | Points to Consider |
| Referral | Patients are referred to occupational therapy by a variety of sources, including family members, caregivers, physicians, health care centers, employers, etc.
–Occupational therapists cannot work with any patient because the patient may have a therapeutic need; patients must be referred. |
Anyone can refer a patient to occupational therapy, including the patient. Occupational therapy services cannot be provided, however, without an evaluation. A prescription, also called an order, for an evaluation must be issued by the patient’s physician (including medical doctor, doctor of osteopathy, psychiatrist, or other holding a medical degree), nurse practitioner (subject to state law), chiropractor, or dentist.
–Physician’s orders for occupational therapy are required in most states and by most insurance providers. |
Therapists can also refer to other therapeutic practitioners. -Visual acuity issues=refer to the optometrist -Eye disorders= refer to the ophthalmologist -Not following dietary recommendations=refer to the dietician -Speech delay=refer to the speech language pathologist -Gait disorders=refer to the physical therapist.A referral can be very specific such as asking for a neoprene splint or general by asking to test for a developmental delay. |
| Screening | After the referral, the occupational therapist needs to screen the patient in order to determine if an evaluation is needed. A screening is used to obtain preliminary information of the patient’s situation. | The occupational therapist or occupational therapy assistant may complete observation of the patient, checklists, and medical record review. –The occupational therapist may also use a quick screening tool such as the ACL. |
Occupational therapists should discuss the patient’s status with other health care providers and with the patient’s family before pursuing an evaluation.
Before conducting a screening, the OT should summarize the benefits and reasons for administering the type of screening tool. If the patient does not want to answer the questions from a questionnaire then the OT must acknowledge the view of the caregiver and transition to asking informal interview questions. You cannot document the results of the screening tool if the caregiver does not complete it.
|
| Evaluation | An occupational therapist can use a standardized assessment such as the Peabody Developmental Motor Scales, Functional Independence Measure (FIM), or the Sensory Profile. If a standardized assessment is used, then the therapist needs to follow the assessment word for word and step by step.
-Criterion referenced assessment: the patient’s scores on the assessment are compared to predetermined criteria or standards. The Functional Independence Measure (FIM) is an example of a criterion referenced assessment. An occupational therapist can also use a non-standardized assessment. |
The occupational therapist completes the evaluation, including administering evaluation tools, scoring the results, and writing the evaluation report. –The occupational therapy assistant may assist with the evaluation by completing those portions of the assessments that he or she has been trained to administer under the supervision of the occupational therapist. |
Therapists should consider any language or cultural barriers prior to or while conducting an evaluation. For example, if the therapist has an accent that is different from the patient’s and the patient cannot understand verbal directions due to the therapist’s accent, the therapist should arrange for an alternate means of communication, such as written instructions or asking another staff member to act as an interpreter. |
| Intervention | Intervention is provided based on 4 levels. These levels will be discussed in a separate chart. See below. | The occupational therapist or occupational therapy assistant may provide intervention. The occupational therapy assistant is supervised by the occupational therapist based on the occupational therapy assistant’s experience, complications that may arise during intervention, and any pertinent rules, regulations and insurance requirements. | An occupational therapy aide may not provide occupational therapy intervention. An occupational therapy aide may assist the occupational therapist or occupational therapy assistant in providing portions of the intervention under close supervision. Occupational therapy aides should be trained in providing portions of intervention before assisting therapists with patients.
When designing a program, the OT needs to research relevant literature to support the process of evidence-based decision-making.
|
| Discharge | The patient is discharged from occupational therapy services when goals are met, when progress has plateaued, or when the patient’s medical condition changes and the patient is unable to tolerate occupational therapy services.
–Planning for discontinuation of services begins at the evaluation. |
The occupational therapist recommends discharge from occupational therapy services to the referring physician, who approves the dismissal.
–In the public schools, the occupational therapist recommends dismissal to the IEP team, who must agree with the recommendation. |
Discharge from occupational therapy services may be dictated by the patient’s insurance company and the limits on the amount of occupational therapy that is allowed by the patient’s policy.
Occupational therapy assistants may give the occupational therapist input regarding the discharge of patients but may not recommend discharge themselves. |
Name the part of the service delivery process that applies to each situation:
1. A manufacturing company consults with an OT about the increased number of back injuries among the employees. The company wants all employees in identified jobs to be trained in injury prevention.
2. The OT works with a person following a myocardial infarction in an outpatient clinic three times weekly for strengthening to improve work related skills.
3. A 30-year-old woman with a brain stem CVA presents for a wheelchair assessment with her mother. She independently uses an augmentative communication device. She has been seated in a manual wheelchair for 5 years and is dependent on her aging mother and father for all mobility and activities. During the assessment, the mother informs the OT that she is not ready for her daughter to regain independence.
4. An inpatient who has borderline personality disorder has been hospitalized due to an exacerbation of suicidal and self-mutilating behavior. An initial evaluation has been completed and it indicates that the patient is functioning at Allen Cognitive level V (exploratory actions). The patient reports being overwhelmed by a new personal relationship, experiencing job dissatisfaction, and feeling a lack of control in many daily situations.
5. An individual with chronic undifferentiated schizophrenia is referred to a day hospital. The referring psychiatrist notes that the patient’s positive symptoms have responded well to a new medication, but the negative symptoms remain.
6. An OT is evaluating a patient who has an ulnar nerve injury at the wrist level of the right dominant extremity.
7. A therapist has just received a referral for a resting hand splint. The therapist is in the process of determining the need for an in-depth evaluation.
Answers:
1. Screening
2. Intervention
3. Evaluation
4. Intervention
5. Screening
6. Evaluation
7. Screening
The Occupational Profile 
The evaluation portion begins with the OT and patient developing an occupational profile that reviews the patient’s occupational history and describes the patient’s current needs and priorities. This includes the patient’s previous roles and the contexts for occupational performance.
The Occupational Profile is most often initiated with an interview with the patient, and significant others in the patient’s life, and by a thorough review of available records. Interviews may be completed using a formal instrument or informal tools.
Although the Occupational Profile is used to focus subsequent intervention, this profile is often revised throughout the course of intervention to meet a patient’s needs.
The purpose of the Occupational Profile is to answer the following questions as outlined by the American Occupational Therapy Association (AOTA):
1. Who is the patient?
This requires consideration of not only the individual but the significant others in the patient’s life. In some settings the patient may be identified as a group and not as an individual. For example, a patient who sustained a traumatic brain injury resulting in memory deficits and slight difficulties with coordination, is a wife and a mother to two young children. During the evaluation process, the OT considers not only the patient’s occupational needs but also the needs of her family and her roles as a family member.
2. Why is the patient seeking service?
This relates to the occupational needs identified by the individual and significant others.
3. What occupations and activities are successful or are problematic for the patient?
This includes understanding which occupations are successfully completed by the patient and which the patient would have difficulty resuming.
4. How do contexts and environments influence engagement in occupations and desired outcomes?
Some contexts may be supportive, whereas others present challenges or prohibit occupational performance.
5. What is the patient’s occupational history?
This includes the level of engagement in various occupations and activities along with the value attributed to those occupations by the patient.
6. What are the patient’s priorities and targeted outcomes?
These may be identified as occupational performance, role competence, adaptation to the circumstance, health and wellness, prevention, or quality-of-life issues.
The OT directs the evaluation by completing an occupational profile, interpreting the data collected from the profile, and then analyzing the patient’s occupational performance prior to proceeding to assessment of patient factors.
After the Occupational Profile is developed, the OT identifies the necessary additional information to be collected, including areas to be evaluated and what assessment instruments should be used prior to the analysis of occupational performance. The OT may delegate some parts of the evaluation, such as the administration of selected assessment tools, to the OTA. The interpretation of data is the responsibility of the OT.
The selection of additional information beyond the Occupational Profile should answer the following questions:
1. What additional data are needed to understand the patient’s occupational needs including contextual supports and challenges?
2. What is the best (most efficient and accurate) way to collect these data?
3. How will this information support the intervention plan?
4. How will this information influence potential outcomes?
The ability of the patient to successfully plan, initiate, and complete various occupations is then evaluated. The occupations chosen are based on the occupational profile. The OT then analyzes the data to determine the patient’s specific strengths and weaknesses that impact occupational performance. The impact of contextual factors on occupational performance is included in the analysis of data.
 Clinical Reasoning
Clinical Reasoning
Clinical reasoning can be defined as the process used by OT practitioners to understand the patient’s occupational needs, make decisions about intervention services, and as a means to think about what we do.
There are 5 basic forms of clinical reasoning which can be applied to practice.
1. Procedural Reasoning
Procedural reasoning is concerned with getting things done, with what “has to happen next.” This reasoning process is closely related to the medical form of problem solving. The emphasis is often placed on patient factors and body functions and structures. A connection between the problems identified and the interventions provided is sought using this form of reasoning.
2. Interactive Reasoning
Interactive reasoning is concerned with the interchanges between the patient and therapist. The therapist uses this form of reasoning to engage with, to understand, and to motivate the patient. Understanding the disability from the patient’s point of view is fundamental to this type of reasoning. This form of reasoning is used during the evaluation to detect the important information provided by the patient and to further explore the patient’s occupational needs. During intervention, this form of reasoning is used to assess the effectiveness of the intervention selected in meeting the patient’s goals. The therapeutic use of self fits well with this form of clinical reasoning as a therapist employs personal skills and attributes to engage the patient in the intervention process.
3. Conditional Reasoning
Conditional reasoning is concerned with the contexts in which interventions occur, the contexts in which the patient performs occupations, and the ways in which various factors might affect the outcomes and direction of therapy. Using a “what if?” or conditional approach, the therapist imagines possible scenarios for the patient. The therapist engages in conditional reasoning to integrate the patient’s current status with the hoped-for future. Intervention is often revised on a moment-to-moment basis to proceed to an outcome that will allow the patient to participate in various contexts.
4. Narrative Reasoning
This type of reasoning relies on story telling in order to identify problem areas and solutions. It requires interaction between the patient and therapist in order to gain an understanding of the situation. Therapists also use narrative reasoning to plan the intervention session, to create a story line of what will happen for the patient as a result of therapy. The therapeutic use of self is critical when using this type of clinical reasoning. Providing an opportunity for the patient to share the meaning of their disability experience helps with formulating plans and projecting future occupational performance. This is where the context and occupational performance intersects.
5. Pragmatic Reasoning
Pragmatic reasoning recognizes the constraints faced by the OT practitioner by forces beyond the patient-therapist relationship. It focuses on logistics such as cost, time, resources, therapist’s skills, patient’s wishes, and physical location. It looks at the problems and focuses on developing practical and realistic solutions. These challenges to providing intervention would be considered when developing an intervention plan.
Questions a therapist may consider using related to each type of clinical reasoning:
Pedretti’s Occupational Therapy – E-Book (Occupational Therapy Skills for Physical Dysfunction (Pedretti)) (p. 36).
| Type of Reasoning | Questions |
| Procedural Reasoning | What is the diagnosis?
What prognosis, complications, and other factors are associated with this diagnosis? What is the general protocol for assessment and intervention with this diagnosis? What interventions (adjunctive methods, enabling activities, purposeful activities) might be employed? What evidence supports the use of specific interventions to foster occupational performance? |
| Interactive Reasoning | Who is the patient?
What are the patient’s goals, concerns, interests, and values? How does the patient view his or her occupational performance status? How does the illness or disability fit into the patient’s performance patterns? How might I engage this patient? How can we communicate? |
| Conditional Reasoning | What contexts has the patient identified as important in his or her life?
What future(s) can be imagined for the patient? What events could or would shape the future? How can I engage the patient to imagine, believe in, and work toward a future? |
| Narrative Reasoning
|
What does the change in occupational performance mean to this patient?
How is this change positioned within the patient’s life history? How does the patient experience the disabling condition? What vision does the therapist hold for the patient in the future? What “unfolding story” will bring this vision to fruition? |
| Pragmatic Reasoning
|
What organizational supports and constraints must be incorporated into the provision of services?
What physical environmental factors must be considered when designing an intervention plan? What is the therapist’s knowledge and skill level? |
Experienced clinicians use all forms of reasoning to develop and modify their plans and actions during all phases of the occupational therapy process,
OCCUPATIONAL THERAPY INTERVENTION
The Four Levels of Intervention
 Intervention is adjusted based on a patient’s needs, but usually aligns with one of 4 levels
Intervention is adjusted based on a patient’s needs, but usually aligns with one of 4 levels
| Level | Description | Examples | Photo |
| Adjunctive | This may be the initial step in the intervention process in order to prepare the patient for occupational performance. These methods are often used to prepare the patient for meaningful activities and are often used in the acute care setting. Education, physical agent modalities, and resources are used at this level. | A customized exercise pamphlet with stretches and strengthening exercise that the patient can do at home 1-2 times every day Providing electrotherapeutic agents to improve muscle strength, modulate pain, and relax targeted muscles with other physical agent modalities Educating the patient on ways to prevent pain by including exercise, diet, sleep, and stress avoidance into their daily life Teaching relaxation, breathing, mediation, and coping techniques Providing the patient with community resources, workshops, and associations so the client can have access to a support system Verifying whether the patient was provided with the right wheelchair for the right purpose |
 |
| Enabling Activities | These are exercises or ways to condition the body in order to get to the patient’s end goal.
-Together the occupational therapist and the patient can work on range of motion, muscle conditioning, schedules, pacing activities, coping strategies, time management, and medication management. |
Practicing exercise techniques such as stretching and strengthening with an elastic band or with other types of adaptive equipment, such as a reaching stick, in order for the patient to do his or her morning grooming routine.
The patient can write in a daily journal to document performance, accidents, injuries, and emotions |
 |
| Purposeful Activities | These activities have a relevant goal and are meaningful to the patient.
The performance of purposeful activities includes compensatory strategies and adaptations to facilitate a patient’s involvement in activities. |
Practicing gardening techniques with adaptive equipment in the therapy clinic to work toward a goal of returning to gardening at home.
Work tabletop practice activities, practice boards, simulators, driving simulators, and hooks for mastering dressing along with methods that stimulate Compensatory strategies examples: A teenage boy with a diagnosis of advanced muscular dystrophy uses a head pointer to type on a computer keyboard since he cannot use his hands to type. |
 |
| Occupation-Based Activity | Interventions at this level include client centered activities and goals. The therapist’s involvement begins to decrease as the client performs ADLs, IADLs, play, and leisure to his or her own maximum capacity. | A patient cooks eggs for her kids in their home. A patient plays softball in the community with a friend. |
 |
Intervention Approaches
5 Intervention Approaches
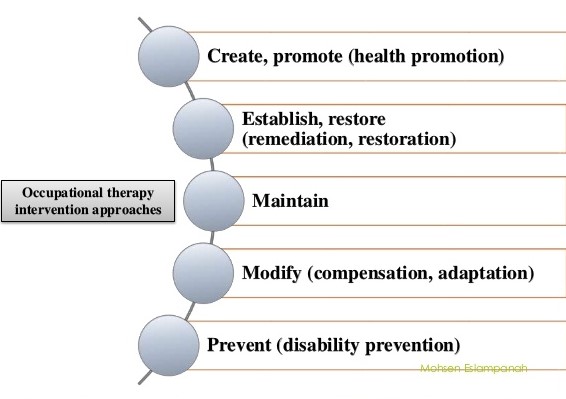
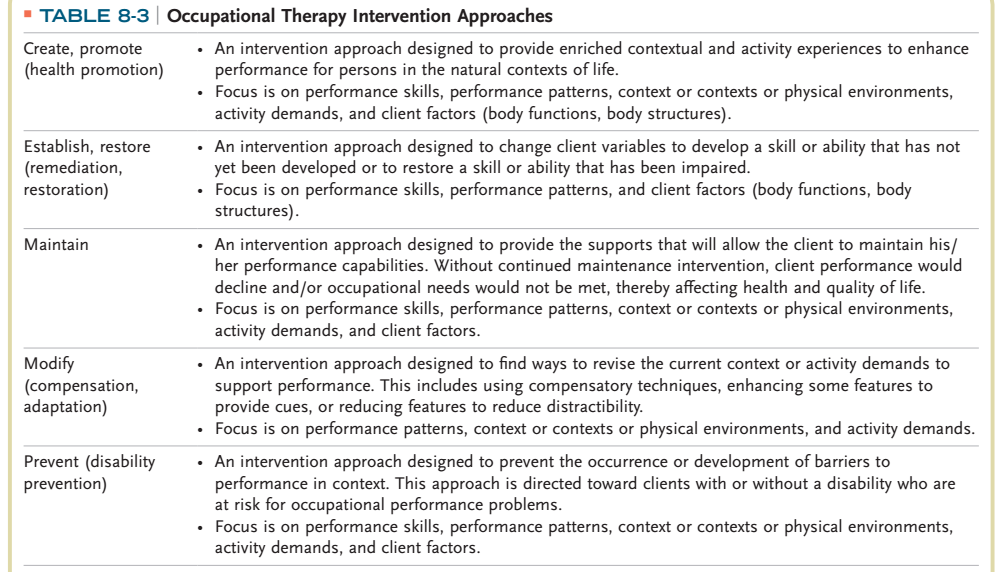
Table reference: Pendleton, Heidi McHugh. Pedretti’s Occupational Therapy – E-Book (Occupational Therapy Skills for Physical Dysfunction (Pedretti)) (p. 125). Elsevier Health Sciences. Kindle Edition.
The unique role of the OT is to contribute to the patient’s care plan and the rehabilitation process, by establishing a method that assists the patient to reach a state of physical, mental, and social wellbeing, to identify and attain their aspirations, to satisfy their personal needs, and to change or cope with their environment.
Each patient’s intervention plan is formulated using selected theories, frames of reference, practice models, and evidence. This process is directed by the patient’s goals, values, beliefs, and occupational needs, and is based on the patient’s goals and priorities. Establishment of the intervention plan is a collaborative effort between the therapist and the patient or, if the patient is unable to collaborate, the patient’s family or caregivers.
Summary of Intervention Approaches
1. Health promotion and wellness to enable or enhance performance in everyday life activities.
2. Establishment, remediation, or restoration of a skill or ability that has not yet developed or is impaired.
3. Maintenance and enhancement of capabilities without which performance in everyday life activities would decline.
4. Compensation, modification, or adaptation of activity or environment to enhance performance.
5. Prevention of barriers to performance, including disability prevention.
Focus on the Intervention Approach of Modification, Adaptation and Compensation
In a remediation approach, intervention is targeted towards improving performance components, with the assumption that such improvements will lead to enhanced occupational performance.
If a patient’s previous abilities cannot be restored, utilizing an adaptive or compensatory approach can promote participation in occupations. This approach focuses on the patient’s remaining abilities and aims to improve function by compensating for deficits in performance components. Ultimately, optimal occupational performance is achieved through successful adaptation.
OTs view individuals to be independent whether they perform the component activities by themselves, perform the occupation in an adapted or modified environment, use various devices or alternative strategies. The OT facilitates the achievement of occupational performance goals by finding ways to revise the current context or activity demands to support performance.
Including:
• Modifying or adapting tasks, activities and environments
• Using assistive devices to maximize function and compensate for lost function
• Using compensatory strategies
Adaptations
In simple terms, an adaptation makes performing an activity easier. An adaptation is a change in the structure, function, or form of the activity to promote a better adjustment to the environment in which the patient lives. Adaptation may involve changing the tool or the technique used to complete a task. It is important to note that, although adapting may involve making changes to an activity to make the task possible for a patient according to their abilities, adaptation does not change the outcome of the activity. The manner of how the activity is accomplished, is purposefully altered to make it achievable for the patient.
Adaptations may require:
– Restructuring of the physical environment to assist occupational performance.
– Changing the technique used to perform an activity.
– Modifying or substituting objects used in performing an activity to make it easier to complete.
– Using adaptive equipment, assistive technology, and environmental modifications to compensate.
Examples of Adaptations:
• Applying Velcro to replace shoelaces
• Listening to music to filter out certain stimuli while working
• Putting different textured surfaces onto individual keys to aid in finding the correct one
• Adapting working conditions- physical space and lighting to maximize productivity
• Adjusting the height of the table to improve posture
• Assistive devices such as basic a long-handled sponge for bathing.
• Adapting a wheelchair for a respiratory unit
• Recommending environmental adaptations to assist with physical, perceptual, and cognitive functioning, such as labeling cupboards and drawers, or using lighting to improve vision and/or attention to task
Providing assistive devices is an important element of OT intervention to support the patient’s performance and increase their participation in their occupations. Assistive devices are classified as adaptive equipment as the patient requires the assistance of an external device (assistive device or aid) to be independent in their occupations. i.e.: The patient is Modified Independent. If the assistive technology acquired does not match the skills and abilities of the patient, the OT then adapts them accordingly.
Modifications
Types of Environmental Modifications
1. Changes to the Physical Environment
• Modify the layout (remove a door to make the opening wider)
• Provide adaptive equipment (a tub bench)
• Architectural modifications (provide a ramp, bathroom modifications)
2. Modification of the Occupation (modify behavior)
• Education about how to use the environment in a different way (always turn on lights before entering a room for an individual who has low vision)
• Use everyday items to achieve goals (always carry a mobile phone to call for help if needed)
Examples of Modifications
• In a work environment, the OT can modify the way that the worker performs the work or modify the work environment to allow the worker to perform optimally.
• Home Modifications: The main goal of home modifications is maximizing safety and independence in the home. This involves reviewing aspects of the home that may require modification to facilitate performance and making changes to adapt living spaces to increase usage, safety, security, and independence. It includes recommendations for alterations, adjustments, or additions to the home environment through the use of specialized, customized, off-the-shelf, or universally designed technologies; low- or high-tech equipment, furnishings; and other features that affect the layout and structure of the home. Common home modifications include increasing lighting with nightlights or increased light bulb wattage, replacing faucets and door knobs with levers, installing non-skid materials in bathing areas and on stairs, adding handrails or grab bars, widening doorways, and adding ramps.
• To make a bathroom accessible for a patient in a wheelchair, the bathroom can be modified to allow independence with BADLs.
• A patient who has been diagnosed with a progressive disease will experience a decline in their ability to function independently. As the disease progresses, there is a greater need for environmental support such as durable medical equipment, modifications to the home, and adaptive equipment.
• Recommending modifying a patient’s diet in terms of changing the texture if they have difficulty swallowing thin liquids.
Compensation
Determining new ways of accomplishing an activity. Finding strategies/techniques or using specially adapted tools that work around the patient’s limitations. In comparison to adaptation which involves altering the setting or demands of a task to facilitate performance. Compensatory strategies do not usually involve equipment, technology, or modifications to the environment.
Examples of Compensatory Techniques/Strategies
• Teaching a patient who presents with muscle weakness in their shoulders how to use a compensatory technique of propping their elbows and bringing their hand to their mouth when eating.
• Fatigue management or energy conservation techniques for COPD
• Teaching hemi-dressing techniques (dressing affected side of body first, using adaptive dressing aids such as a button hook)
• Techniques for completing tasks with functional use of one hand (for example, using a dycem mat to stabilize a mixing bowl while breaking an egg into the bowl with one hand)
• Using a daily planner or reminder functions on mobile phones to compensate for poor memory
• Shopping during quieter supermarket hours to manage social anxiety
• A patient with COPD sits at the kitchen table to chop vegetables for dinner rather than standing at the counter to conserve energy.
• A patient with a left above elbow amputation holds a jar of pickles between his knees and uses his right hand to open the jar.
SUMMARY
Adaptation = Add
Modification = Change
Compensation = Use what the patient has available/use the strengths the patient already possesses