GUIDELINES FOR PROPER
PERSONAL PROTECTIVE EQUIPMENT (PPE)
DURING OT INTERVENTIONS
…. ..
. … .
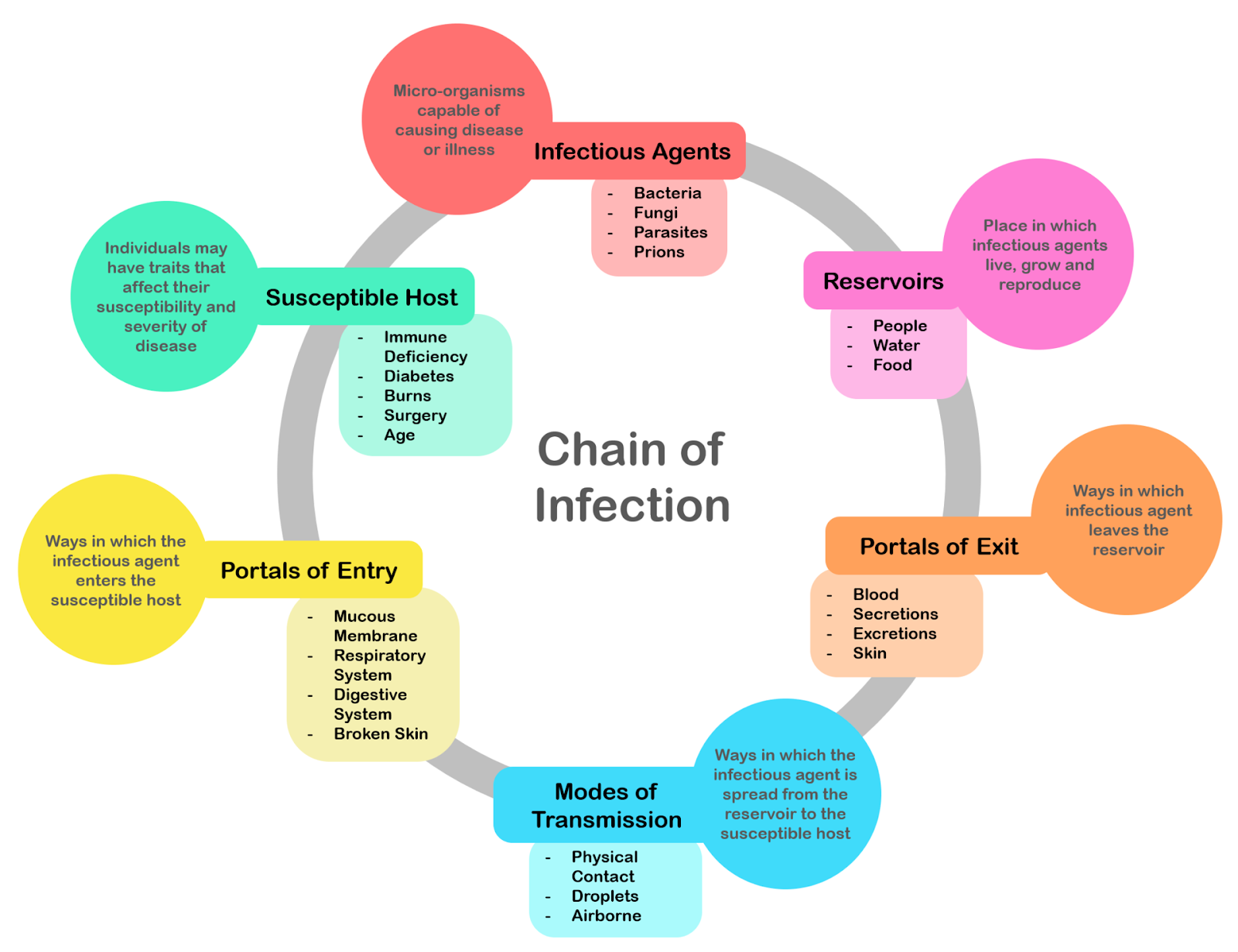
 How Infection Works
How Infection Works
There are five major categories of infectious agents: Viruses, bacteria, fungi, protozoa, and helminths.
1. Viruses are responsible for a wide range of diseases, including the common cold, measles, chicken pox, genital herpes, and influenza. Many of the emerging infectious diseases, such as AIDS and SARS, are caused by viruses.
2. Bacterial infections are associated with diseases such as strep throat, tuberculosis, staph skin infections, and urinary tract and bloodstream infections.
3. Fungi (spore-forming organisms that range from bread mold to ringworm to deadly histoplasmosis)
4. Protozoa (such as the agents behind malaria and dysentery)
5. Helminths (parasitic worms like those that cause trichinosis, hookworm, and schistosomiasis).
6. Prions, or proteinaceous infectious particles consisting only of protein. Prions are thought to cause variant Creutzfeldt-Jakob disease in humans and “mad cow disease” in cattle.
Microorganisms capable of causing disease (pathogens) usually enter our bodies through the mouth, eyes, nose, or urogenital openings, or through wounds or bites that breach the skin barrier.
Some diseases spread via direct contact with infected skin, mucous membranes, or body fluids. Diseases transmitted this way include cold sores (herpes simplex virus type 1) and sexually transmitted diseases such as AIDS. Pathogens can also be spread by indirect contact when an infected person touches a surface such as a doorknob, countertop, or faucet handle, leaving behind microbes that are then transferred to another person who touches that surface and then touches his or her eye, mouth, or nose. Droplets spread by sneezes, coughs, or simply talking can transmit disease if they come in contact with mucous membranes of the eye, mouth, or nose of another person. SARS, tuberculosis, and influenza are examples of diseases spread by airborne droplet transmission.
 . . ..
. . ..
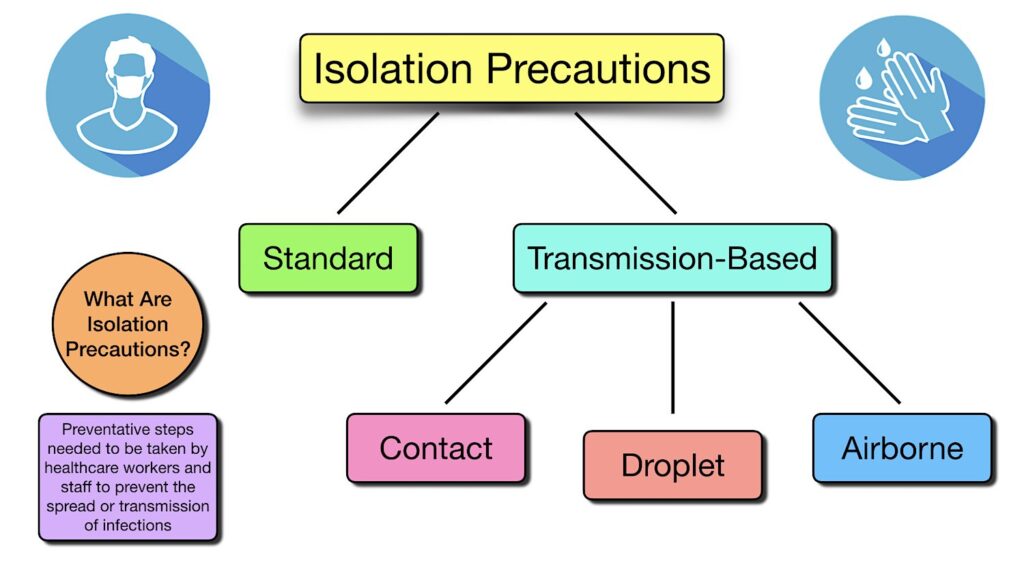
INFECTION PREVENTION AND CONTROL
A. STANDARD PRECAUTIONS
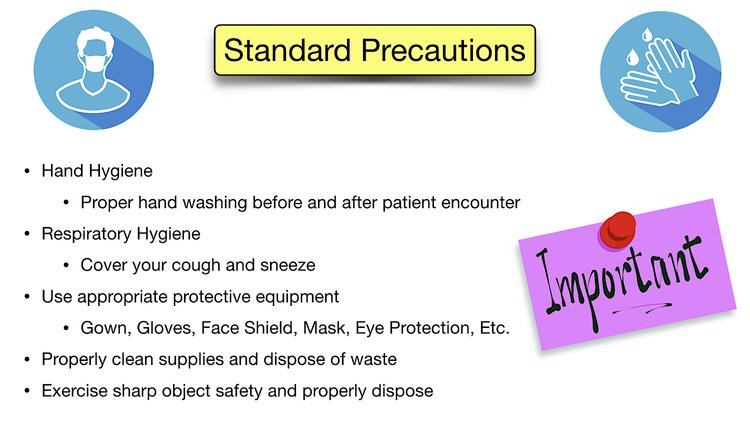
Standard Precautions are used for all patient care. They’re based on a risk assessment and make use of common sense practices and personal protective equipment use that protect healthcare providers from infection and prevent the spread of infection from patient to patient.
Standard precautions are the minimum steps that should be taken with all patients to prevent the spread of infections and diseases and include:
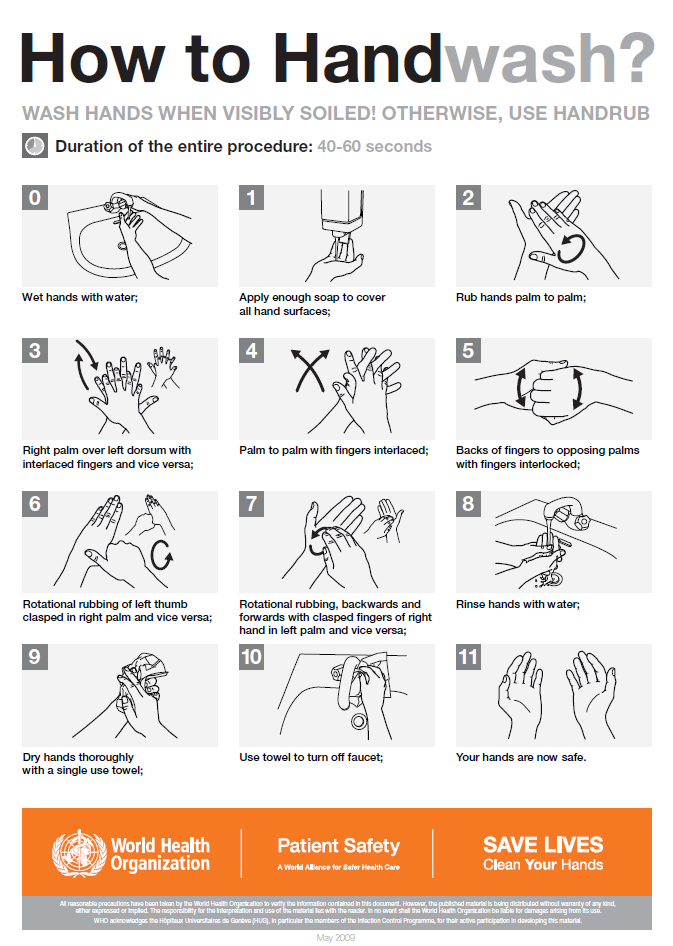
• Proper Hand Hygiene – some diseases require hand washing with soap and water rather than alcohol-based products or sanitizers.
** Hand washing before and after patient encounter
• Proper Respiratory Hygiene
** Covering your cough and sneeze
• Use of Appropriate Protective Equipment
** While certain PPE is required when a patient is in transmission-based isolation, appropriate protective equipment should be used as a standard precaution if the task being performed necessitates it. The items selected for use by the healthcare worker will depend on the type of interaction they have with a patient and the likely modes of disease transmission. This includes gown, gloves, face shield, mask and eye protection being used to create barriers that protect your skin, clothing, mucous membranes, and the respiratory tract from infectious agents.
* Wear gloves when touching blood, body fluids, non-intact skin, mucous membranes, and contaminated items.
* Wear a surgical mask and goggles or face shield if there is a reasonable chance that a splash or spray of blood or body fluids may occur to the eyes, mouth, or nose.
* Wear a gown if skin or clothing is likely to be exposed to blood or body fluids.
• Cleaning of Supplies – surfaces should be cleaned, disinfected, and/or sterilized appropriately.
• Proper Disposal of Sharp Objects and Waste
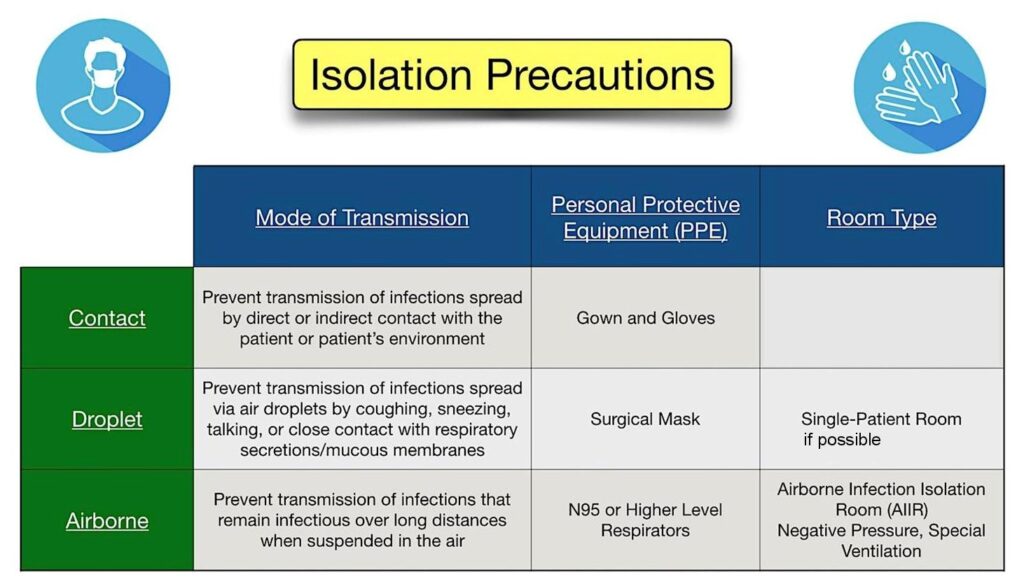
B. TRANSMISSION-BASED PRECAUTIONS
Transmission-based precautions are extra steps that must be taken, in addition to the standard precautions, in order to prevent the transmission of certain diseases. Transmission-based precautions typically require some form of personal protective equipment (PPE).
Respiratory particles can be classified as being droplets or aerosols (fine droplets) based on particle size and their aerodynamic behavior. According to the WHO and the CDC, infections transmitted by particles larger than 5 µm are considered droplet transmission and infections transmitted by particles 5 µm or smaller are considered aerosol transmission. Both droplets and aerosols can be generated during coughing, sneezing, talking, or exhaling. The difference is that large droplets settle rapidly, whereas small aerosols can remain airborne and travel over longer distances by airflow. As for the respiratory tract, aerosols are more likely to be inhaled deeply into the lower respiratory tract (affecting the lungs and alveolar tissues), while larger droplets will remain trapped in the upper airway. For this reason, infections caused by aerosols can lead to more serious illnesses.
THERE ARE 3 MAIN TYPES OF TRANSMISSION-BASED PRECAUTIONS:
1. Contact Precautions
2. Droplet Precautions
3. Airborne Precautions
The main difference between airborne and droplet precautions is that airborne precautions protect against particles that travel through the air, while droplet precautions protect against particles that travel through the air and drop onto surfaces.
1. CONTACT PRECAUTIONS
Contact precautions help prevent the transmission of infections spread by direct or indirect contact with the patient or patient’s environment. Contact precautions require a gown and gloves be worn in addition to the standard precautions. The gown and gloves are put on when entering the room and taken off when leaving the room. This is done to contain the pathogen and prevent contamination.

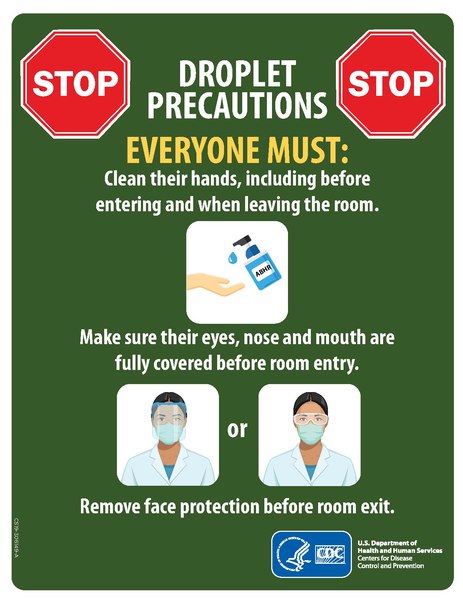
2. DROPLET PRECAUTIONS
Droplet precautions help prevent the transmission of infections spread through air droplets by coughing, sneezing, talking, or close contact with respiratory secretions or mucous membranes. In addition to following standard precautions, a surgical mask is required for droplet precautions. The mask is put on when entering the room. Pathogens in the droplet precaution category do not remain infectious over long distances, which is one of the reasons why an airborne infection isolation room is not required. Patients should be placed in individualized rooms, if possible.
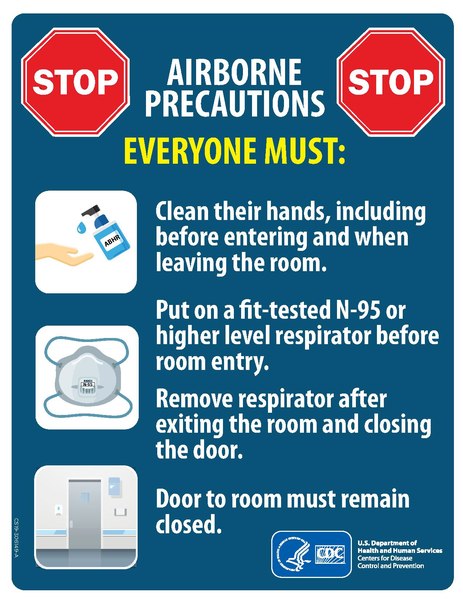
3. AIRBORNE PRECAUTIONS
Aerosol generating procedures (AGPs) are defined as medical and patient care procedures that result in the production of airborne particles ≤5 µm in size, which can remain suspended in the air and travel over a distance. If they contain infectious microorganisms they may cause infection if they are inhaled. AGPs create the potential for airborne transmission of infections that may normally be transmissible primarily by the droplet route.
Mode of Transmission: Droplet nuclei that remain infectious over long distances when suspended in the air. Airborne precautions help prevent the transmission of diseases that remain infectious over long distances when suspended in the air. Airborne infections live as tiny residue particles in the air, called droplet nuclei, and they are waiting to be inhaled. That is why in addition to following standard precautions, an N95 or higher level respirator must be worn for airborne precautions. The respirators must be put on prior to entering the room.
Patients who require airborne precautions should be placed in a special room called an Airborne Infection Isolation Room (AIIR). AIIRs are single-patient rooms with special air handling and ventilation. They are negative pressure rooms with 6-12 air exchanges every hour depending on when the facility was built. Air is released directly to the outside or recirculated through a special filtration system.
Summary
| Contact Diseases | Droplet Diseases | Airborne Diseases | |
| Examples | • Staph infections • Hepatitis A, B & C • HIV • Cold sores • Coxsackievirus (hand-foot-mouth disease) • Diarrhea (infectious) • Lice • Ringworm • Scabies • Conjunctivitis (Pink-eye) • Polio. • Roseola. |
• Seasonal influenza virus • Neisseria meningitidis (meningococcal meningitis) • Rubella virus (German measles) • Bordetella pertussis (pertussis) |
• Anthrax • Chickenpox • Adenovirus • Rotavirus • Influenza • Rhinovirus • Streptococcus pneumoniae • Measles • Mumps • Smallpox • Tuberculosis • Bordetella pertussis • Severe acute respiratory syndrome (SARS) • Middle East Respiratory Syndrome (MERS) • Coronavirus Disease 2019 (COVID-19) |
| Precautions | Use Contact Precautions for patients with known or suspected infections that represent an increased risk for contact transmission.
• Use personal protective equipment (PPE) appropriately
|
Use Droplet Precautions for patients known or suspected to be infected with pathogens transmitted by respiratory droplets that are generated by a patient who is coughing, sneezing, or talking.
• Surgical mask & goggles |
Use Airborne Precautions for patients known or suspected to be infected with pathogens transmitted by the airborne route
• N95 mask – OT practitioner |
CONSIDERATIONS BEFORE BEGINNING DIRECT CONTACT TREATMENT
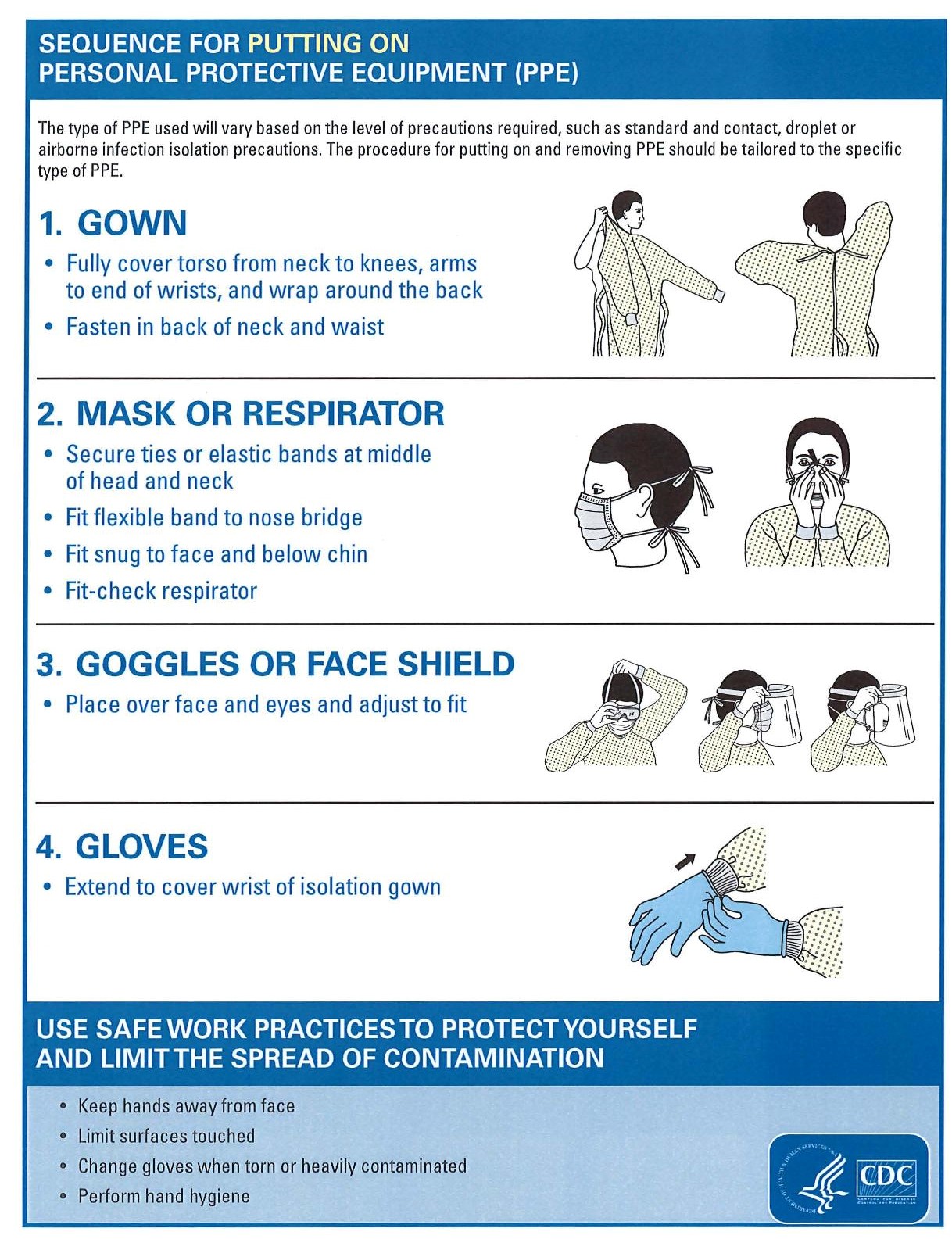
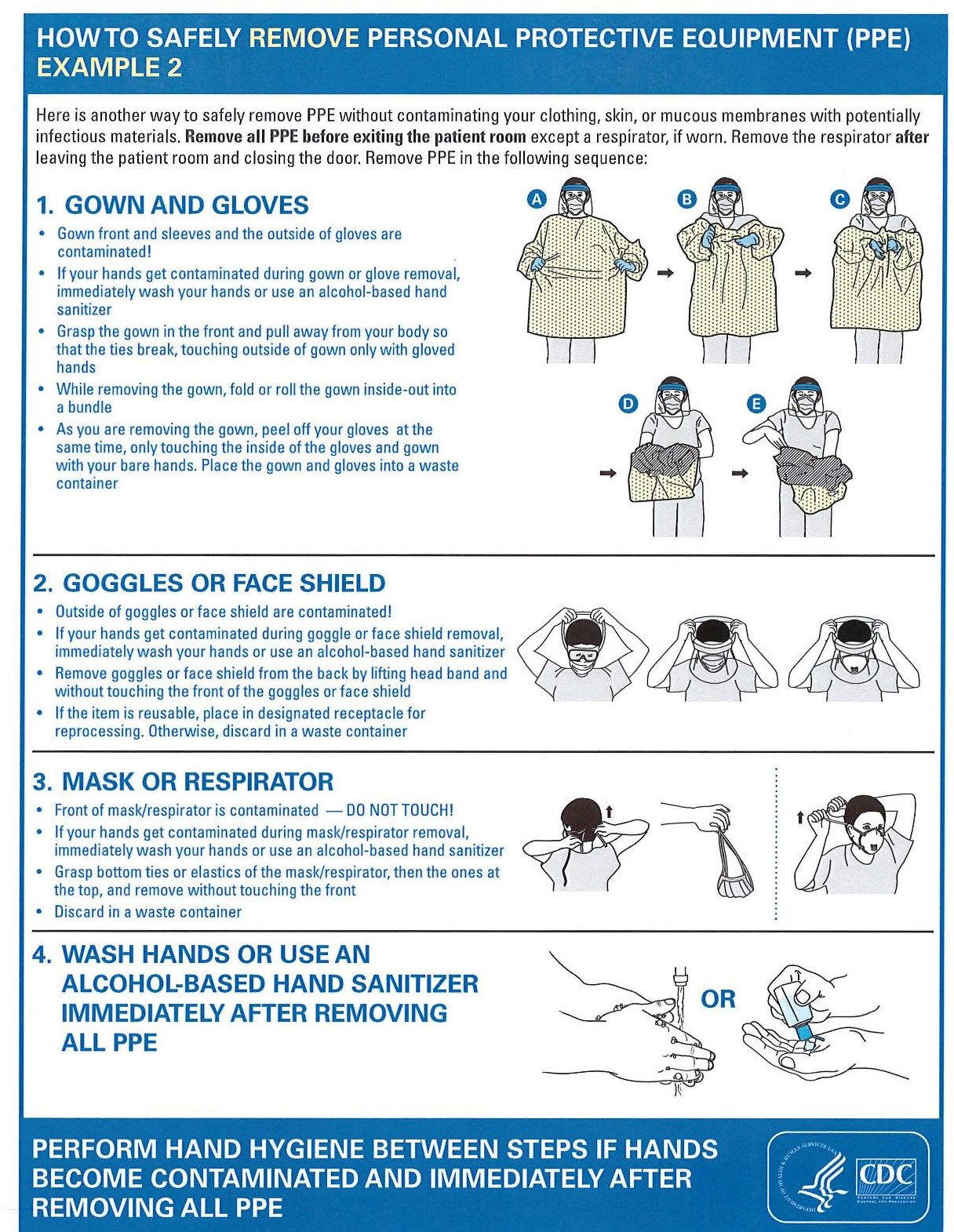
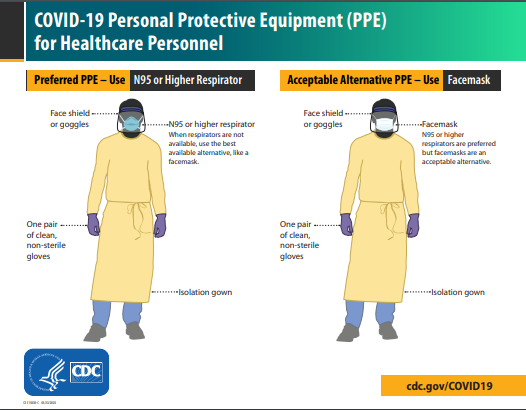
1. Determine type of Personal Protective Equipment (PPE) needed for direct patient contact:
– Some procedures may require droplet and contact protection only.
– Aerosol Generating Procedures (AGPs) require airborne precautions.
2. Ensure a step-by-step process for donning and doffing PPE to avoid contamination.
3. Identify the minimum number of people required to safely conduct a session.
4. Consider bundling care with other healthcare professionals (e.g., coordinating activities; grouping care for all patients with COVID-19).
5. Carefully consider equipment use and discuss with infection control services to ensure it can be properly decontaminated. Avoid moving equipment between infectious and non-infectious areas. Wherever possible, single patient use, disposable equipment is preferred (e.g., low tech AAC equipment that can be discarded after use, TheraBand rather than hand weights).
PRECAUTIONS SPECIFIC TO OT
Three-Tiered Risk Classification- where occupations are classified as high, moderate, or low risk for AGPs.
1. Low-Risk Occupations
Suggested level of PPE: CDC and WHO Standard Precautions
❏ Practice hand hygiene
❏ Masks should be worn by both the patient and practitioner
❏ Gloves should be worn when appropriate
2. Moderate-Risk Occupations
These occupations are not necessarily aerosol generating; however, control parameters relevant to context could affect the risk of performing these occupations.
Suggested level of PPE:
❏ Practice hand hygiene
❏ Masks should be worn by both the patient and practitioner
Bathing/Showering are high-contact care activities where splashes and sprays are anticipated, and high contact patient/patient care activities provide opportunities for transfer of pathogens to the hands and clothing of the practitioner.
❏ Wear a gown to reduce risk from splashes and sprays
Toileting is considered a high-contact care activity where splashes and sprays are anticipated and provide opportunities for transfer of pathogens to the hands and clothing of the practitioner.,/span> Bio-aerosol transmission via toilet plumes is associated with flushing toilets and is a potential concern to health care practitioners.
❏ Wear a gown to reduce risk from splashes and sprays
❏ If toilet has a lid, it should be lowered during flush to minimize toilet plumes
Functional & Community Mobility should be considered moderate risk activities, as long as standard precautions are utilized.
** Consider factors such as proximity, duration, and potential for mobilizing secretions during mobility activities.
** Complete these activities in well-ventilated areas, including outdoors, when appropriate.
Exercise should be considered a moderate-risk activity, as long as standard precautions are utilized. There are no available studies that indicate that exercise promotes generation of aerosols.
** Consider factors such as proximity, duration, and potential for mobilizing secretions during exercise
** Complete these activities in well-ventilated areas, including outdoors, when appropriate.
3. High-Risk Occupations
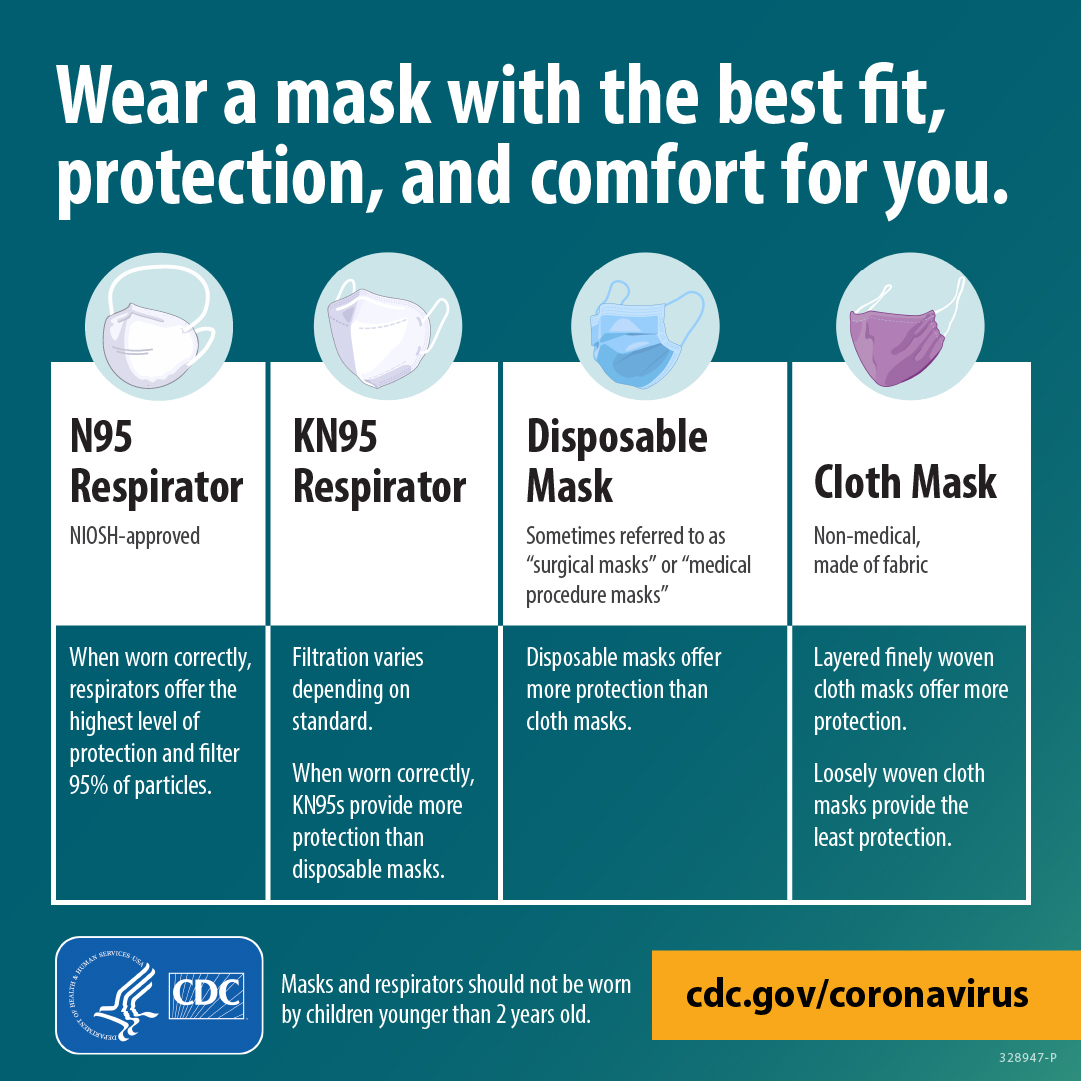
Suggested level of PPE (WHO, 2020):
❏ N95 (or higher) respirator
❏ Gown
❏ Eye Protection (goggles/face shield)
❏ Gloves
Feeding & Swallowing, including dysphagia care, swallowing assessments, and related preparatory activities (i.e., sensory & oral motor) result in the generation of aerosols with close proximity to a patient and high risk of coughing.
Hygiene & Grooming is performed in close proximity to an unmasked patient, which increases instances of saliva splatter and patient coughing, which results in particle transfer. Spread through aerosols can happen with low-speed hand-held dental brushes, water picks, and manual tooth brushing.
Sleep Preparation using a CPAP or BiPAP machine will generate aerosols. Situations where practitioners are in the same room as a patient who is using a CPAP or BiPAP or are working with patients to clean these machines should be considered high risk.
** Practice donning/doffing CPAP or BiPAP with the machine off. This activity would still constitute a moderate risk to the practitioner as the patient is not able to wear a mask.
………………. …. 
HOW TO WASH YOUR HANDS
HOW TO DON & DOFF A MEDICAL MASK
Use of well-fitting masks in healthcare settings are an important strategy to prevent the spread of respiratory viruses.
– Before touching the mask, clean your hands with an alcohol-based hand rub or soap and water.
– Inspect the mask for tears or holes; do not use a mask that has previously been worn or is damaged.
– Verify which side is the top – this is usually where the metal strip is.
– Then, identify the inside of the mask, which is usually the white side.
– Place the mask on your face covering your nose, mouth and chin, making sure that there are no gaps between your face and the mask. Place the straps behind your head or ears. Do not cross the straps because this can cause gaps on the side of the mask.
– Pinch the metal strip so it conforms to the shape of your nose.
– Remember, do not touch the front of the mask while using it to avoid contamination; if you accidentally touch it, clean your hands.
How to take off a medical mask:
– Before touching the mask, clean your hands with an alcohol-based hand rub or soap and water.
– Remove the straps from behind the head or ears, without touching the front of the mask.
– As you remove the mask, lean forward and pull the mask away from your face.
– Medical masks are for single use only; discard the mask immediately, preferably into a closed bin.
– Clean your hands after touching the mask.
– Be aware of the condition of the mask; replace it if while working with a patient, it gets soiled or damp.

HOW TO DON & DOFF PPE
 COVID-19
COVID-19
Transmission of COVID-19 from inhalation of the virus in the air can occur at distances greater than six feet. Particles from an infected person can move throughout an entire room or indoor space. The particles can also linger in the air after a person has left the room – they can remain airborne for hours in some cases. People who are infected with COVID can release particles and droplets of respiratory fluids that contain the SARS CoV-2 virus into the air when they exhale (e.g., quiet breathing, speaking, singing, exercise, coughing, sneezing). The droplets or aerosol particles vary across a wide range of sizes – from visible to microscopic. Spread may also occur through contact with contaminated surfaces, though this route is now considered less likely.
Symptoms
The most common symptoms of COVID-19:
• Fever
• Chills
• Sore throat.
Other symptoms that are less common and may affect some patients include:
• Muscle aches
• Severe fatigue or tiredness
• Runny or blocked nose, or sneezing
• Headache
• Sore eyes
• Dizziness
• New and persistent cough
• Tight chest or chest pain
• Shortness of breath
• Hoarse voice
• Heavy arms/legs
• Numbness/tingling
• Nausea, vomiting, abdominal pain/ belly ache, or diarrhea
• Appetite loss
• Loss or change of sense of taste or smell
• Difficulty sleeping.
Symptoms of severe COVID‐19 disease which need immediate medical attention include:
• Difficulty in breathing, especially at rest, or unable to speak in sentences
• Confusion
• Drowsiness or loss of consciousness
• Persistent pain or pressure in the chest
• Skin being cold or clammy, or turning pale or a bluish color
• Loss of speech or movement.
How to protect yourself and your patients
You can protect yourself and others from COVID-19 by following preventive measures, such as keeping a distance, wearing a mask in crowded and poorly ventilated spaces, practicing hand hygiene, respiratory etiquette (covering your mouth and nose with a bent elbow or a tissue when you cough or sneeze), getting vaccinated and staying up to date with booster doses.
When treating patients who are infectious follow the highest level of precautions- Airborne Precautions
Latest Update: WHO announced in May 2023 that COVID-19 is now an established and ongoing health issue which no longer constitutes a public health emergency of international concern (PHEIC).
References:
https://www.aota.org/-/media/Corporate/Files/Practice/Health/Aerosol-Generating-Procedures-Decision-Guide.pdf
https://www.who.int/emergencies/diseases/novel-coronavirus-2019/question-and-answers-hub/q-a-detail/coronavirus-disease-covid-19