
Documentation is necessary whenever professional services are provided to a client.
Each occupational therapy client has a client record maintained as a permanent file. The record is maintained in a professional and legal fashion (i.e., organized, legible, concise, clear, accurate, complete, current, grammatically correct, and objective).
The purpose of documentation is to:
• Articulate the rationale for provision of occupational therapy services and the relationship of this service to the client’s outcomes
• Reflect the occupational therapy practitioners’ clinical reasoning and professional judgment
• Communicate information about the client from the occupational therapy perspective
• Create a chronological record of client status, occupational therapy services provided to the client, and client outcomes.
Points to consider regarding documentation:
● Daily treatment notes should be recorded using a narrative or checklist format to track data and performance in-between progress reports. Daily documentation should be completed as soon after a treatment session as possible while the information is fresh in the therapist’s mind.
● Third party payers often have requirements regarding documentation. Facilities often write policies and procedures regarding documentation to meet the requirements of third-party payers, especially Medicare and Medicaid. These procedures should be followed to meet the requirements for payment for occupational therapy services.
Elements Present in All Documentation
1. Client’s full name and case number (if applicable) on each page of documentation.
2. Date and type of occupational therapy contact.
3. Identification of type of documentation, agency, and department name.
4. Occupational therapy practitioners’ signature with a minimum of first name or initial, last name, and professional designation.
5. When applicable on notes or reports, signature of the recorder directly at the end of the note without space left between the body of the note and the signature.
6. Countersignature by an occupational therapist on documentation written by students and occupational therapy assistants when required by law or the facility.
7. Acceptable terminology defined within the boundaries of setting.
8. Abbreviations usage as acceptable within the boundaries of setting.
9. When no facility requirements are listed, errors corrected by drawing a single line through an error and by initialing the correction (liquid correction fluid and erasures are not acceptable).
10. Adherence to professional standards of technology, when used to document occupational therapy services.
11. Disposal of records within law or agency requirements.
12. Compliance with confidentiality standards.
13. Compliance with agency or legal requirements of storage of records.
https://ajot.aota.org/article.aspx?articleid=1867123

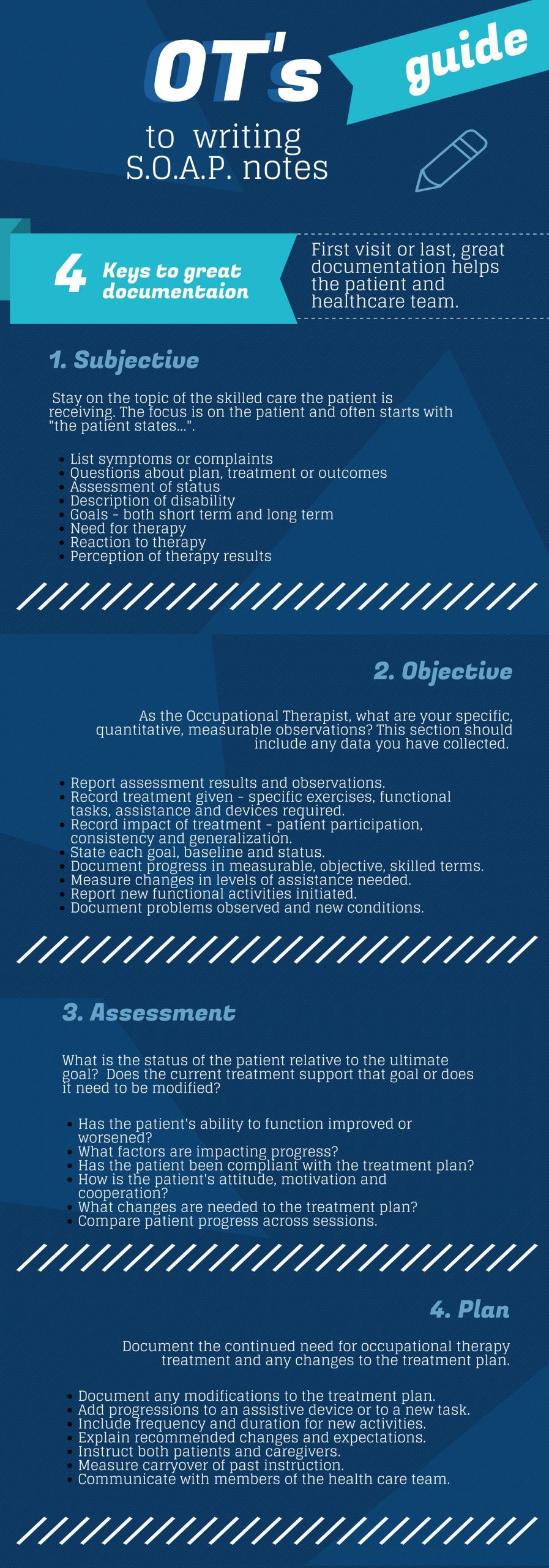
The standard format of documentation for occupational therapy services is the SOAP note.
| Section | Definition | Example |
| S – Subjective | A subjective statement about the patient’s status, performance or emotional state should be included. | “The patient appeared weepy at the beginning of the session and stated that she could not sit up to wash her face.” |
| O -Objective | Objective data related to the patient’s performance should be included. When documenting an evaluation, observations regarding performance and standardized test results are documented. When documenting progress, data related to treatment goals is included. | “The patient’s strength measurements are as follows:
Grip strength: Lateral pinch strength: |
| A – Assessment | A summary of the patient’s performance and conclusions based on the objective data are included here. An evaluation will include a statement on whether or not the patient requires occupational therapy services and what skills should be addressed. A progress report will include a statement on what level of progress the patient demonstrates. | “Slow progress observed. The patient’s progress is partially affected by her lack of motivation to participate in daily ADL tasks.” |
| P- Plan | On an evaluation, this section will include long and short-term treatment goals, treatment methods and modalities, treatment frequency and duration, and treatment billing codes. A progress report will include revisions to treatment goals, methods, modalities, frequency and duration, and billing codes. | “Continue per plan of care to address ADL skills, upper body strength, and general endurance.” |
https://www.ottoolkit.com/blog/soap-notes/
Documentation of Therapy Goals
Goal setting is an important part of the therapeutic process. OTs work in a client centered manner focusing their assessments and treatment plans around a client’s wishes, aspirations and goals. Therefore, it is important for the OT and the client to have open communication about what these are. The goals will then influence the direction of the occupational therapy process.
OTs recognize that treatment should be relevant to a patient’s lifestyle and that outcomes need to be judged in relation to a patient’s goals. A patient who makes a functional, independence-focused goal statement may perceive the treatment activities as more meaningful and, therefore, work harder to attain those goals, thus achieving higher functional outcomes
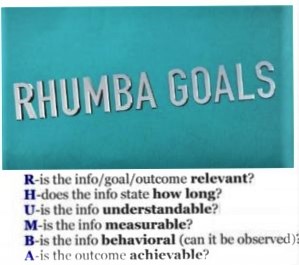
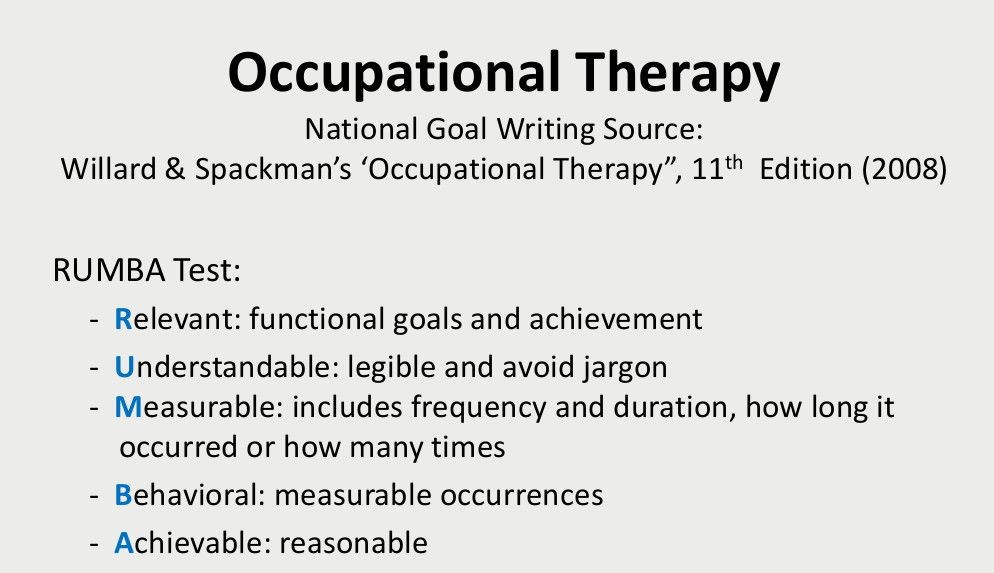
There are several goal setting acronyms, most of which include the same elements.
Below is an outline of the COAST, RHUMBA and SMART methods.

The COAST method for goal writing was introduced in Gateley & Borcherding’s “Documentation Manual for Occupational Therapy”. This framework is great for ensuring that you’re addressing a specific occupation with your goals and establishing specific timelines for goal achievement.

| C – Client will perform |
Matt will
|
| O– Occupation
What occupation? |
feed himself 50% of the meal |
| A – Assist Level
With what level of assistance /independence? |
with minimal physical assistance |
| S – Specific Condition
Under what conditions? |
using a built-up spoon to scoop up the food |
| T – Timeline
By when? |
within 3 treatment sessions |
SMART METHOD
The SMART goal method is used to set goals for people in many different industries, from marketing strategists to occupational therapists. It’s a well-known framework and provides us with high-level guidance by encouraging an emphasis on time-bound, measurable goals

| S- Specific
What are you going to do, why are you going to do it, and how will it be accomplished? |
By the end of next week, Mary will transfer herself from her wheelchair to the toilet with moderate assistance using DME as needed. |
| M- Measurable
What will be the measure of this goal’s success? When will you know it’s been achieved? |
Yes- this goal will be achieved when she is able to transfer with mod assist and using DME to assist her |
| A- Achievable
Is this goal something that can be achieved by your patient with some work or is it too easy/difficult? |
Yes- this is a realistic aim for her |
| R- Relevant
Does this goal target useful skills/behaviors? |
Yes- this is an important goal for her, to regain her independence |
| T- Time-Bound
On what time-frame will this goal be achieved? |
By the end of next week |
This framework for goal writing was introduced by the 11th edition of Willard & Spackman’s “Occupational Therapy”. It’s particularly helpful for making sure the goals you’re setting for your patients are helpful to both the patient and the family – making sure you’re setting understandable and measurable goals.
Goal: By the end of the semester, Amy will be able to cut across a piece of paper in 4 out of 5 trials with minimal assist and no verbal cues to promote separation of the sides of her hands and hand eye coordination for optimal participation in cutting tasks within the school setting.
| R – Relevant (to the LTG)
What function is this goal aiming to achieve? |
Improving Amy’s ability to cut with scissors. This is an essential skill for her to develop so that she can participate in cutting tasks, with the other children in her class. |
| H – How long (to the LTG)
How long to achieve goal? |
How many sessions do you plan to work on achieving Amy’s goal. |
| U – Understandable
Will the patient understand this goal? |
Yes.
Both Amy and her parents are aware that she is having difficulty in this area and her goal is to improve her skills |
| M – Measurable (quantifiable/criteria for success)
How will you measure this goal? |
She will be able to cut across a piece of paper in 4 out of 5 trials with minimal assist and no verbal cues. By the end of the semester
|
| B – Behavior (client behavior observable)
What behavior occurrences will the goal address? |
By promoting separation of the sides of her hands and hand eye coordination, she will be able to improve her ability to cut with a scissors. This in turn will improve her confidence and level of participation in the classroom.
|
| A – Attainable/achievable
Can you reasonably expect your patient to achieve this goal within the stated time? |
Yes |

Reference: https://blog.fusionwebclinic.com/make-goal-writing-easier