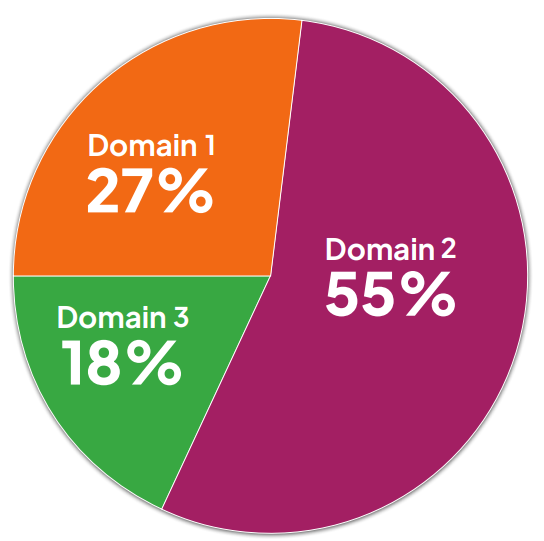
COTA® Exam Outline– for exams from 2024
Why the Test Changes in 2024
Every five years NBCOT® conduct practice analysis studies on the OTR® and COTA® exams. They do this to determine the domains, tasks, and knowledge needed to effectively practice occupational therapy. The goal of a practice analysis is to ensure that the content on the certification exams reflects current entry-level practice.
PLEASE TAKE NOTE: NBCOT® state in their document that examples of specific types of knowledge have been provided for illustrative purposes only, and the examples provided are not an exhaustive list.
DOMAIN 1
Collaborate and Gather Information:
Under the supervision of the OTR®, acquire information on an ongoing basis regarding factors that influence occupational performance.
TASK 1
Recognize the influence of development and lived experience; body function and body structures; values, beliefs, and spirituality; and identity on occupational performance.
Performance of this task requires the following knowledge:
1. Impact of typical development and aging on occupational performance, health, and wellness across the life span.
2. Expected patterns, progressions, and prognoses associated with conditions that limit occupational performance.
Some examples include:
• signs and symptoms of disease
• stages of disease
• secondary complications
3. Impact of body functions and body structures on occupational performance.
Some examples include:
• cognitive impairments
• congenital anomalies
4. Influence of lived experiences and identity on occupational performance.
Some examples include:
• history of trauma and adverse childhood events
• socioeconomic status
• gender, race, culture, religion
TASK 2
Acquire information about a client’s functional skills, roles, prioritized needs and wants, and performance context to inform the development of and updates to an occupational profile.
Performance of this task requires the following knowledge:
1. Resources for acquiring information about the client’s current condition and occupational performance.
Some examples include:
• referrals
• client records
• developmental history
• Individualized Education Program (IEP) plans
2. Purpose, advantages, limitations, and service competency needs related to the administration of standardized and non-standardized assessments and screening methods.
Some examples include:
• criterion-referenced tests
• norm-referenced tests
• client and caregiver interviews
• observation
3. Internal and external factors influencing a client’s engagement in occupation.
Some examples include:
• roles, habits, routines, and rituals
• environmental context
• family and social supports
• medication side effects and interactions
• mental health
TASK 3
Perform an activity analysis to determine the influence of task demands, current conditions, performance skills, and context on occupation.
Performance of this task requires the following knowledge:
1. Task requirements, steps to task completion, and task demands across contexts or settings.
2. Personal and environmental factors that facilitate or inhibit task completion or occupational engagement.
Some examples include:
• compensation patterns
• role of performance context
• influence of current conditions
TASK 4
Collaborate with the client, the client’s relevant others, occupational therapy colleagues, and other professionals using a client-centered approach and therapeutic use of self to provide quality occupational therapy services.
Performance of this task requires the following knowledge:
1. Roles and responsibilities among interprofessional teams when coordinating client care and providing services.
Some examples include:
• referral to and consultation with other services
• interprofessional communication methods
• scope of practice
2. Processes for supporting interprofessional intervention plans.
Some examples include:
• Individualized Education Program (IEP) plans
• discharge plans
• transition plans
• palliative and hospice care plans
3. Client-centered approaches and considerations for coordinating occupational therapy services.
Some examples include:
• therapeutic use of self
• advocacy
• frequency/duration of intervention
• level of service delivery
4. Factors used to prioritize intervention goals and activities in collaboration with the client and family, teacher, caregiver, and relevant others.
Some examples include:
• client-reported outcomes
• level of support required
• context of service delivery
• progress toward goals
5. Strategies for addressing and enhancing health literacy with the client and relevant others.
Some examples include:
• caregiver training
• teaching-learning models
• methods for making health information accessible
• informed decision-making
• navigating challenges to professional expertise
TASK 5
Monitor the intervention plan, approach, context, and goals on an ongoing basis, in collaboration with the OTR®, using clinical reasoning.
Performance of this task requires the following knowledge:
1. Factors for determining and managing context and activities to meet individual and group intervention goals and objectives.
Some examples include:
• client needs and priorities
• response to intervention
2. Strategies for monitoring the effectiveness of individual and group intervention.
Some examples include:
• client-reported outcomes
• reevaluation results
• progress toward goals
3. Clinical decision-making for prioritizing goals and implementing modifications to the intervention plan based on client responses, under the supervision of the OTR®.
Some examples include:
• physiological changes
• behavioral reactions
• emotion regulation
• developmental needs
4. Precautions or contraindications associated with a client condition or stage of recovery.
Some examples include:
• postsurgical precautions
• vital signs
• laboratory values
• suicidal ideation
DOMAIN 2
Select and Implement Interventions:
Implement interventions, under the supervision of the OTR®, in accordance with the intervention plan and level of service competence to support client participation in areas of occupation throughout the occupational therapy process.
TASK 1
Synthesize assessment results to determine eligibility for services and establish a client-centered intervention plan.
Performance of this task requires the following knowledge:
1. Considerations for selecting, preparing, and adapting the intervention technique to support optimal engagement and promote goal achievement.
Some examples include:
• client condition
• client safety
• theoretical approach and frame of reference
2. Considerations for selecting, preparing, and adapting the intervention environment to support optimal engagement and promote goal achievement.
Some examples include:
• ensuring privacy during telehealth sessions
• equipment safety
• line management
3. Indications, contraindications, and precautions associated with wounds and maintaining skin integrity.
Some examples include:
• stage of wound healing
• prevention and management of pressure ulcers
4. Indications, contraindications, precautions, and clinical application of superficial thermal agents.
Some examples include:
• dry whirlpool
• hot packs
• cryotherapy
5. Indications, contraindications, precautions, and clinical application of deep thermal, mechanical, and electrotherapeutic physical agent modalities.
Some examples include:
• transcutaneous and neuromuscular electrical stimulation
• biofeedback
TASK 2
Implement occupation-based strategies to support participation in activities of daily living (ADL), instrumental activities of daily living (IADL), health management, rest and sleep, education, work, play, leisure, and social participation across the life span.
Performance of this task requires the following knowledge:
1. Interventions for supporting leisure and play.
2. Methods for grading an activity, task, or technique based on level of development, client status, response to intervention, and client needs.
3. Considerations for facilitating individual and group participation in shared activities.
Some examples include:
• group processes
• group dynamics
• group type and function
4. Interventions to support cognitive, visual-motor, visual, and perceptual processing and sensory arousal.
Some examples include:
• sensory modulation
• proprioceptive input
• vestibular strategies
• low vision strategies
5. Compensatory and remedial strategies for managing cognitive and perceptual deficits or developmental disabilities.
Some examples include:
• graded cueing
• chaining
• metacognition
• memory aids
6. Adaptive and preventive strategies for supporting optimal engagement in occupation.
Some examples include:
• use of technology/apps
• joint protection
• task simplification
• energy conservation
7. Intervention strategies and techniques used to facilitate oral motor skills for drinking, eating, and swallowing.
Some examples include:
• hand-to-mouth patterns
• mastication
• adaptive utensils
• positioning at mealtime
8. Prevocational, vocational, and transitional services, options, and resources for supporting strengths, interests, employment, and lifestyle goals across the life span.
9. Strategies, techniques, and client-centered education to facilitate functional transfers.
10. Strategies for promoting wellness and mental health.
Some examples include:
• relaxation
• sleep hygiene
• addiction management
TASK 3
Implement interventions for improving sensory, motor, neurological, and physiological status, considering client condition and current stage of recovery, to support occupational performance.
Performance of this task requires the following knowledge:
1. Methods for grading therapeutic exercise and conditioning programs consistent with indications and precautions.
2. Techniques for sensory and motor re-education, pain management, desensitization, edema reduction, and scar management.
Some examples include:
• manual edema mobilization
• nerve gliding
• neuromuscular reeducation
• constraint-induced movement
3. Techniques for promoting improved postural stability, dynamic balance, body mechanics, and breathing patterns during functional tasks.
TASK 4
Select, fabricate, and modify orthotic devices, and provide training in the use of orthotic and prosthetic devices in order to support functional outcomes.
Performance of this task requires the following knowledge:
1. Types and functions of immobilization, mobilization, and restriction orthoses for managing specific conditions and congenital anomalies across the life span.
2. Types and functions of prosthetic devices for upper and lower extremity amputations.
3. Implications of anatomical, physiological, biomechanical, cognitive, and socioeconomic factors and healing principles for orthotic selection, design, fabrication, and modification.
4. Client-centered education and training methods for the safe and effective use of orthotic and prosthetic devices.
TASK 5
Integrate assistive technology options, adaptive devices, mobility aids, and other durable medical equipment into the intervention to enable participation in occupation.
Performance of this task requires the following knowledge:
1. Factors related to measuring, selecting, monitoring the fit of, and recommending modifications to seating systems, positioning devices, and mobility aids.
Some examples include:
• equipment components
• biomechanical considerations
• usability and maintenance
2. Types, characteristics, and features of high- and low-tech assistive technology and adaptive devices.
Some examples include:
• interface options and processor parameters
• equipment components
3. Mobility options, vehicle adaptations, and alternative devices for supporting participation in community mobility.
Some examples include:
• adapted driving controls
• wheelchair tie downs
• alternative transportation options
• dynamic mobile standers
• navigation apps
4. Client factors influencing successful use and maintenance of assistive technology options, adaptive devices, mobility aids, and other durable medical equipment.
Some examples include:
• developmental, physical, functional, cognitive, and mental health status
• prioritized needs
5. Client-centered education and training methods for successful use and maintenance of assistive technology options, adaptive devices, mobility aids, and other durable medical equipment.
TASK 6
Implement environmental modifications, while considering accessibility guidelines, standards, and legislation, to support participation in occupation consistent with client needs and status, task demands, and context.
Performance of this task requires the following knowledge:
1. Principles of ergonomics and universal design for identifying, recommending, and implementing features and reasonable accommodations in the workplace, home, and virtual and public spaces.
2. Processes and procedures for identifying, recommending, and implementing modifications in the workplace, home, and virtual and public spaces.
Domain 3
Uphold Professional Standards and Responsibilities:
Uphold professional standards and responsibilities by achieving service competence and applying evidence-based interventions to promote quality in practice.
TASK 1
Employ evidence-based strategies and approaches to provide safe, effective, and efficient services relevant to individuals, groups, and populations.
Performance of this task requires the following knowledge:
1. Methods for locating, reviewing, and interpreting scholarly research to guide practice-relevant decision-making.
Some examples include:
• applying the Patient, Intervention, Comparison, Outcome (PICO) model
• identifying best evidence
2. Methods for contributing to continuous quality improvement processes and procedures related to occupational therapy service delivery.
Some examples include:
• program evaluation
• acquiring information to measure outcomes
3. Types of evidence-based programming for advancing population health outcomes.
Some examples include:
• aging in place
• fall prevention
• health and wellness
• community support groups
TASK 2
Incorporate risk management techniques at the individual and practice setting levels to protect clients, self, staff, and others from injury or harm.
Performance of this task requires the following knowledge:
1. Infection control procedures and universal precautions for reducing transmission of contaminants.
Some examples include:
• PPE
• isolation precautions
• cleaning equipment
2. Responses to adverse reactions, minor injuries, and emergency situations.
Some examples include:
• minor burns and cuts
• seizures
• diabetic reactions
3. Preventive measures for minimizing risk and promoting safety.
Some examples include:
• proper body mechanics
• safety data sheet (SDS)
• standard operating procedures
• equipment maintenance
• emergency preparedness
• personal safety in the client’s environment
4. Strategies and resources to prevent professional burnout.
Some examples include:
• assessment of personal needs
• self-advocacy regarding workload
• stress management
TASK 3
Provide occupational therapy services in accordance with laws, regulations, state occupational therapy practice acts, and accreditation guidelines to protect consumers and meet applicable reimbursement requirements related to the service delivery setting.
Performance of this task requires the following knowledge:
1. Application of federal regulations, state practice acts, facility policies, and accreditation guidelines related to service delivery across occupational therapy practice settings.
Some examples include:
• health care legislation
• accreditation organizations
• licensing and credentialing
2. Influence of reimbursement policies and guidelines on occupational therapy service delivery.
3. Accountability processes and procedures for justifying, tracking, and monitoring outcomes.
Some examples include:
• relevant practice terminology
• documentation guidelines
TASK 4
Engage in professional development and competency assessment activities relevant to the job role, practice setting, scope of practice, and professional certification standards.
Performance of this task requires the following knowledge:
1. Methods for identifying, documenting, and monitoring service competency and professional development needs.
Some examples include:
• competency self-assessment
• mentoring
2. Application of ethical decision-making and professional behaviors guided by the NBCOT® Practice Standards and Code of Conduct.
Reference:
https://www.nbcot.org/-/media/PDFs/2022_COTA_Content_Outline.pdf