Documentation and Record Keeping
.. 
Documentation is an essential component of Occupational Therapy practice and is required whenever professional services are provided to a patient. Documentation is an ongoing process that continues throughout the patient’s therapy program and includes keeping a record of what occurred during direct patient care, as well as supportive documentation required to justify the need for occupational therapy intervention.
Documentation incorporates screening reports, initial evaluation reports, re-evaluation reports, progress notes, discharge summaries, other medical record entries (e.g., interdisciplinary care plans, MD telephone orders), intervention and equipment authorization requests, letters and reports to families and other health care professionals, and outcomes data collection.
AOTA’s (2015) Standards of Practice for Occupational Therapy states that an OTP documents the occupational therapy services and “abides by the time frames, formats, and standards established by practice settings, federal and state laws, other regulatory and payer requirements, external accreditation programs, and AOTA documents”. These requirements apply to both electronic and written forms of documentation.
Documents are a legal documents and as such must follow the guidelines that will enable it to withstand a legal investigation. All written and computerized therapy documentation must be able to endure a legal review. The medical record may be the most important document in a malpractice suit because it outlines the type and amount of care or services that were given. All information must be accurate and based on first-hand knowledge of care. Deductions and assumptions are to be avoided; judgmental statements do not belong in the therapy notes. The therapist instead should describe the action, behavior, or signs and symptoms that are observed. As these medical records are legal documents, it is considered fraudulent to alter the medical record in any way.
 According to AOTA, the purposes of documentation are to:
According to AOTA, the purposes of documentation are to:
• Provide an accurate justification for the need of skilled occupational therapy service and reimbursement
• Articulate the rationale for the provision of occupational therapy services and the relationship of these services to the patient’s outcome.
• Reflect the therapist’s clinical reasoning and professional judgment
• Communicate information about the patient from an occupational therapy perspective
• Create a chronological record of patient status, occupational therapy services provided to the patient, and patient outcomes
Guidelines
i. Federal privacy mandates (HIPAA) and the Occupational Therapy Code of Ethics must be adhered to at all times during all methods of documentation, whether written, verbal, or computer generated.
ii. Documentation practices and storage and disposal of documentation must meet all state and federal regulations and guidelines, payer and facility requirements, practice guidelines, and confidentiality requirements.
iii. Documentation needs to have clear, concise, accurate, and objective information and should provide sufficient facts to support the need for occupational therapy services. Reimbursement also depends upon accurate, well written documentation that provides the necessary information to justify the need for occupational therapy services.
Format and Content of Documentation
1. Documents should include:
• Patient’s full name, date of birth, gender, and case number, if applicable, on each page of the documentation.
• Identification of type of documentation (e.g., evaluation report, progress report/note)
• Date and type of occupational therapy contact.
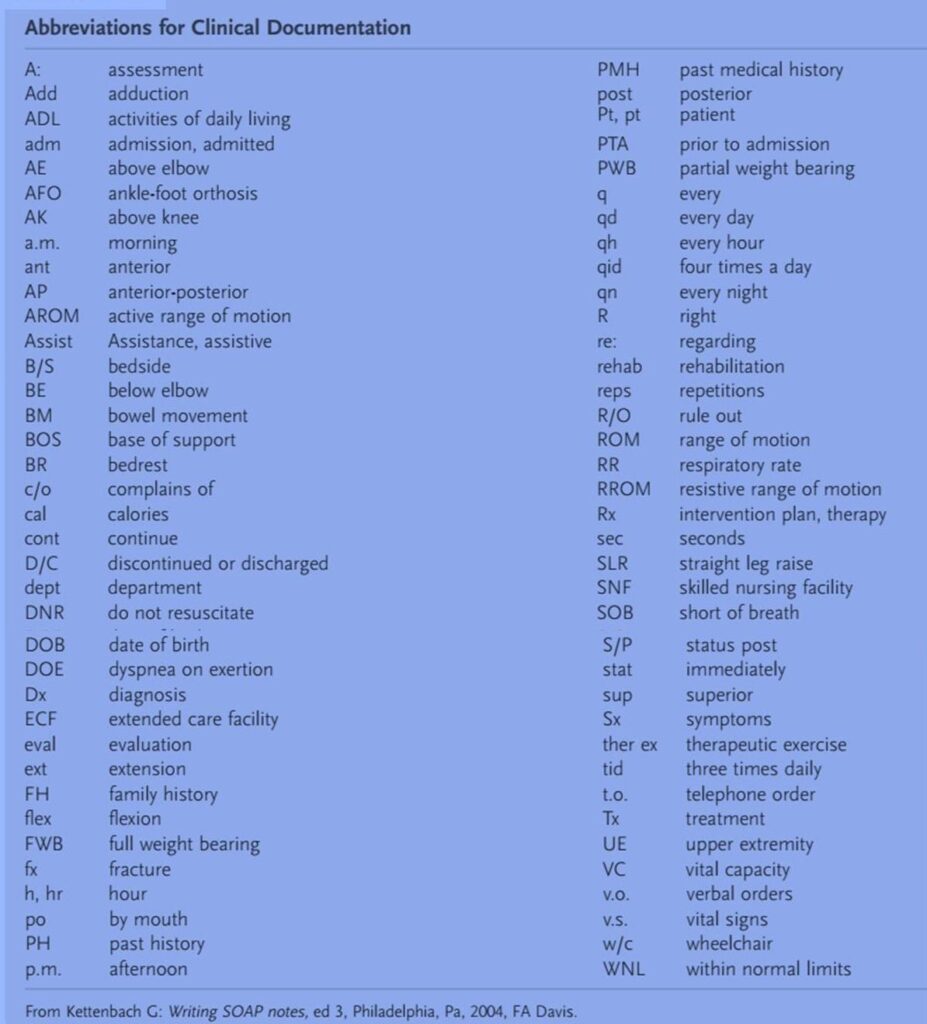
• Acceptable terminology and acronyms as defined within the boundaries of the setting.
• Abbreviation usage as acceptable within the boundaries of the setting.
2. Documentation must be written by the OT practitioner who is providing the intervention. It is never acceptable to write a note for another therapist; in fact, it is considered fraudulent to do so.
All entries made into the medical record must be signed by the OTP.
• The signature must include a first name or initial, last name, and professional designation. I.e.: Your professional initials (OTR®/L, OTL) should follow your signature.
• Do not leave blank spaces at the end of an intervention note. Instead, draw a single line that extends from the last word to the signature. This prevents additional information from being added after the entry has been completed. • Countersignature by an OT may be necessary on documentation written by students and OTAs when required by law or the facility.
3. It is best practice to complete documentation as soon after the therapy session as possible. The longer the time interval between the evaluation or intervention and completion of the written record of the event, the greater the chance that details or other important information will be forgotten.
4. All errors must be noted and initialed or signed.
Altering, substituting, or deleting information from the patient records should never take place. Changes made to the original documentation could be used to support allegations of tampering with the medical record, even when this was not the intent of the writer.
However, at times, when corrections have to be made, several principles should be followed to avoid questioning of the validity of the information.
• Never use correction fluid when correcting an entry in the patient’s record. An acceptable method of correcting an error in the documentation is to draw a single line through the word or words, initial and date the entry, and indicate that this was an “error.”
• Words or sentences cannot be squeezed into existing text “after the fact”. Attempts to do this may be interpreted as adding missing information to support something that occurred after the original documentation was completed.
5. Late entries to the medical record cannot be backdated. If it is necessary to enter information that is out of sequence (e.g., a note that the therapist forgot to write), it must be entered into the medical record as a “late entry” and must be identified as such.
6. Documentation practices and storage and disposal of documentation must meet all state and federal regulations and guidelines, payer and facility requirements, practice guidelines, and confidentiality requirements.
 Types of Documentation
Types of Documentation
Documentation can be paper based (written record) or computer generated. Computerized documentation can be used to record all aspects of the occupational therapy process from the evaluation report to the discharge report.
Use of an electronic documentation program may improve therapists’ efficiency and it guarantees legibility and ensures that no areas are left uncompleted. Computerized evaluation forms and progress notes are usually formatted to meet the needs of the facility and include the information required for reimbursement.
Confidentiality and Documentation
Federal laws have been enacted to protect the consumer against breaches of confidentiality. The privacy sections of HIPAA clearly outline the expectations of health care professionals in issues of confidentiality. The law requires that health care providers adopt privacy and security standards by which to protect confidential medical information of patients.
Ethical practice demands that the OTP understands what is meant by confidential information and is knowledgeable about how to maintain patient confidentiality. Maintaining confidentiality in documentation is the responsibility of the OTP. As outlined by AOTA Code of Ethics: “Occupational therapy personnel shall protect all privileged confidential forms of written, verbal, and electronic communication gained from educational, practice, research, and investigational activities unless otherwise mandated by local, state, or federal regulations.”
Information that is confidential must remain confidential. This means that information cannot be shared verbally, electronically, or in writing without appropriate consent. Information must be shared on a need-to-know basis only with those having primary responsibilities for decision making.
• All occupational therapy personnel shall respect the confidential nature of information gained in any occupational therapy interaction.
• Occupational therapy personnel shall respect the individual’s right to privacy.
• Occupational therapy personnel shall take all due precautions to maintain the confidentiality of all verbal, written, and electronic, augmentative, and nonverbal communications (as required by HIPAA).
To ensure patient confidentiality 
1. Information about patients, including their names, diagnoses, and intervention programs, cannot be discussed outside of the treatment environment.
2. Patient charts should not be removed from the facility. Reports containing personal information (name, social security number, medical diagnosis, etc.) cannot be left out in plain view, where others can read the information.
3. Therapists, students, and staff cannot discuss patients in public areas where others may overhear the conversation.
![]() . .
. .
References:
Pedretti’s Occupational Therapy – E-Book: Practice Skills for Physical Dysfunction (Occupational Therapy Skills for Physical Dysfunction