SCI Terminology & the ASIA Impairment Scale
…………………………………………..
Understanding the ASIA Impairment Scale
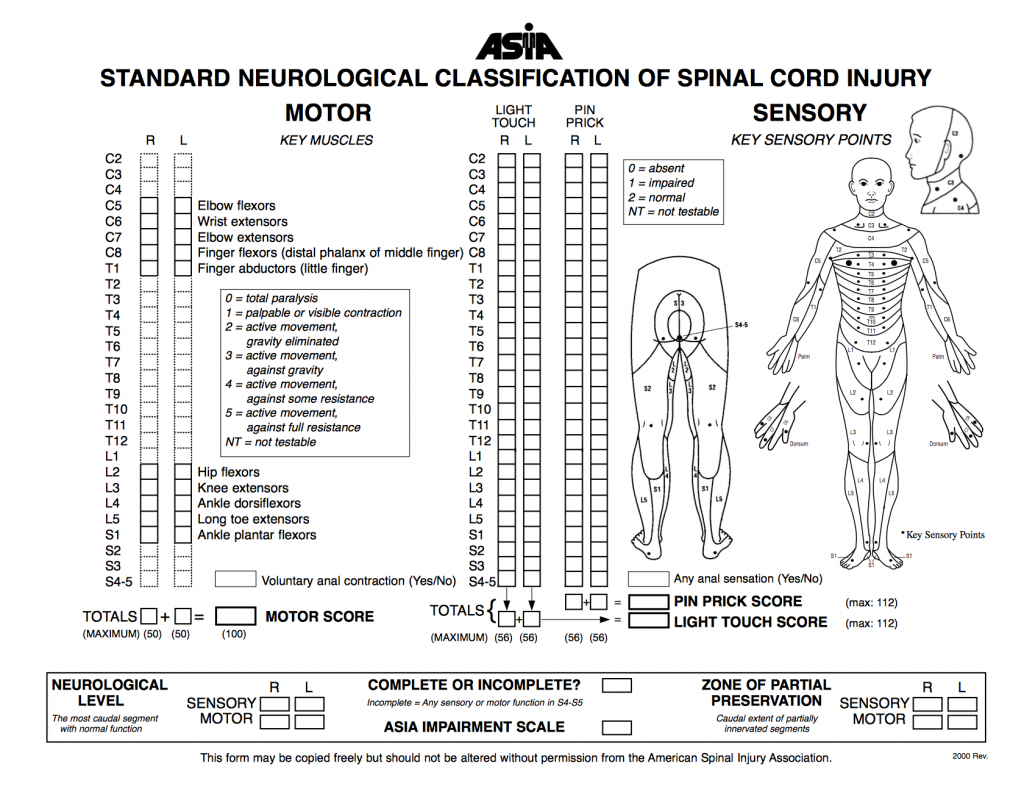
ASIA Examination
• Sensory level
• Motor level
• Neurological level of injury (NLI)
• Complete vs. Incomplete injury
• Sacral sparing
• Zone of Partial Preservation (complete injuries)
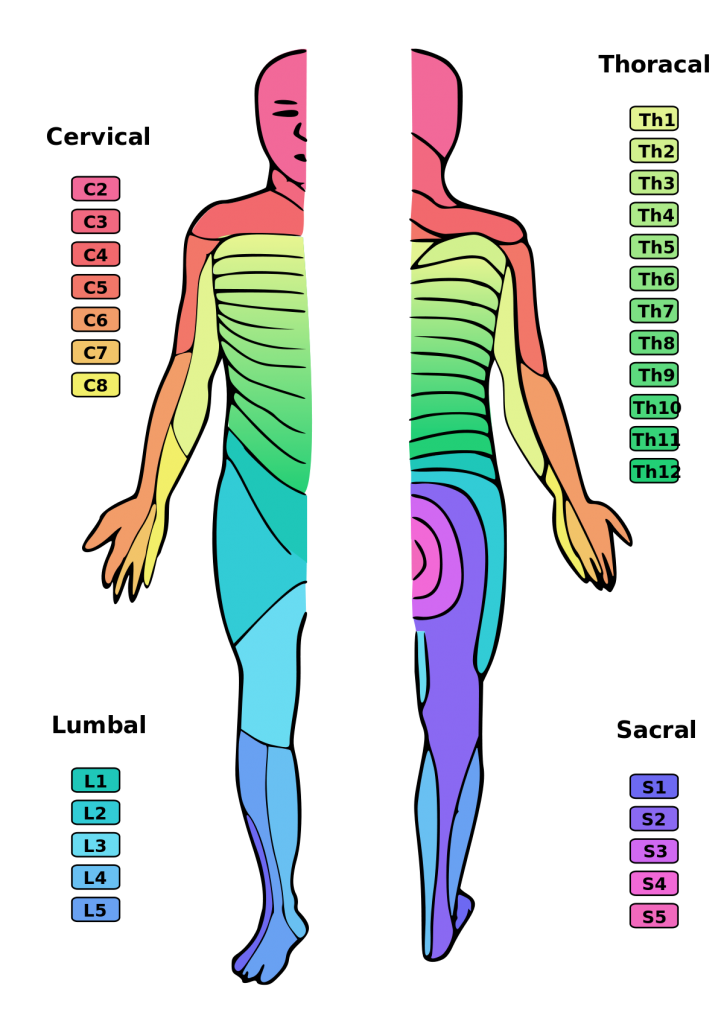
Dermatome:
This term refers to the area of the skin innervated by the sensory axons within each segmental nerve (root). Dermatomes are clinically important and necessary for assessing and diagnosing the level of spinal cord injury in the American Spinal Injury Association (ASIA) Impairment scale.
The spinal cord has 31 segments, each with a pair (right and left) of ventral (anterior) and dorsal (posterior) nerve roots that innervate motor and sensory function, respectively. The anterior and posterior nerve roots combine on each side to form the spinal nerves as they exit the vertebral canal through the intervertebral foramina or neuroforamina. The 31 spine segments on each side give rise to 31 spinal nerves, which are composed of 8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 1 coccygeal spinal nerve. Dermatomes exist for each of these spinal nerves, except the first cervical spinal nerve. Sensory information from a specific dermatome is transmitted by the sensory nerve fibers to the spinal nerve of a specific segment of the spinal cord.
This list details the nerve roots and the approximate area of skin that they provide innervation to. The dermatomes of the head are supplied by branches V1, V2 and V3 of the trigeminal nerve.
• Cranial nerve 5 (trigeminal)
o V1 – ophthalmic branch – top of the head
o V2 – maxillary branch – nares to the top lip
o V3 – mandibular branch – bottom lip to jaw
• C2 – occipital protuberance
• C3 – supraclavicular fossa
• C4 – acromioclavicular joint
• C5 – lateral antecubital fossa
• C6 – thumb
• C7 – middle finger
• C8 – little finger
• T1 – medial antecubital fossa
• T2 – the apex of the axilla
• T3- T12 – bands down the torso
• L1 – upper anterior thigh
• L2 – mid anterior thigh
• L3 – medial femoral condyle
• L4 – medial malleolus
• L5 – dorsum of 3rd metatarsal phalangeal joint
• S1 – lateral heel
• S2 – popliteal fossa
• S3 – ischial tuberosity
• S4-5 – perianal area
Myotome:
The anatomical term myotome refers to the muscles served by a spinal nerve root. A myotome is, therefore, a set of muscles innervated by a specific, single spinal nerve. Ten muscle groups represent the motor innervation to the cervical and lumbosacral spinal cord.
Muscle strength in a particular myotome helps in identifying at which level a nerve root is compromised.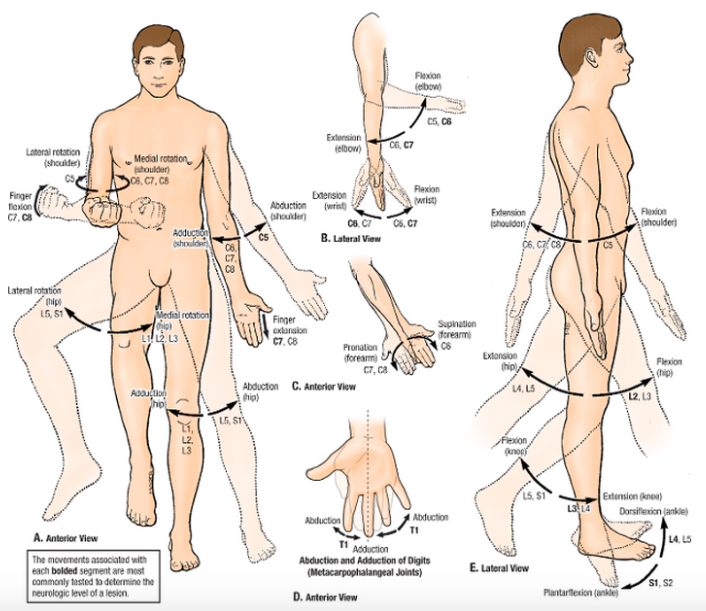
This list details which movement is most strongly associated with each myotome:
• C5 – Elbow flexion
• C6 – Wrist extension
• C7 – Elbow extension
• C8 – Finger flexion
• T1 – Finger abduction
• L2 – Hip flexion
• L3 – Knee extension
• L4 – Ankle dorsiflexion
• L5 – Great toe extension
• S1 – Ankle plantarflexion
Motor level:
The motor level is determined by examining a key muscle function within each of the 10 myotomes on each side of the body, and is defined by the lowest key muscle function that has a grade of at least 3 (on manual muscle testing- MMT) in the supine position, providing the key muscle functions represented by segments above that level are judged to be intact (graded as a 5 on MMT).This may be different for the right and left side of the body.
Motor scores:
This term refers to a numerical summary score of motor function. There is a maximum score of 25 for each extremity, totaling 50 for the upper limbs and 50 for the lower limbs. This score can reflect the degree of neurological impairment associated with the SCI.
Sensory level:
Defined as the most caudal, intact dermatome for both pin prick and light touch sensation. The sensory level is determined by performing an examination of the key sensory points within each of the 28 dermatomes on each side of the body (right and left) and is the most caudal, normally innervated dermatome for both pin prick (sharp/dull discrimination) and light touch sensation. This may be different for the right and left side of the body.
Sensory scores:
This term refers to a numerical summary score of sensory function. There is a maximum total of 56 points each for light touch and pin prick (sharp/dull discrimination) modalities, for a total of 112 points per side of the body. This can reflect the degree of neurological impairment associated with the SCI.
Skeletal level:
This term has been used to denote the level at which, by radiographic examination, the greatest vertebral damage is found.
Neurological Level of Injury (NLI):
The NLI refers to the most caudal segment of the spinal cord with normal sensory and antigravity motor function on both sides of the body, provided that there is normal (intact) sensory and motor function rostrally.
– The sensory level refers to the most caudal, intact dermatome for both light touch and pinprick sensation.
– The motor level refers to the most caudal myotome with a key muscle function of at least grade 3.
If there is a discrepancy between the most caudal intact section between the four possible levels of right sensory level, left sensory level, right motor level, or left motor level, the neurological level of injury is considered the most rostral segment of these four levels. Thus, up to 4 different segments may be identified in determining the neurological level, i.e., R(ight)-sensory, L(eft)-sensory, R-motor, L-motor. The single NLI is the most rostral of these levels.
Complete injury:
This term is used when there is an absence of sensory and motor function in the lowest sacral segments (S4-S5) (i.e. no sacral sparing).
Incomplete injury:
This term is used when there is preservation of any sensory and/or motor function below the neurological level that includes the lowest sacral segments S4-S5 (i.e. presence of “sacral sparing”). Sensory sacral sparing includes sensation preservation (intact or impaired) at the anal mucocutaneous junction (S4-5 dermatome) on one or both sides for light touch or pin prick, or deep anal pressure. Motor sacral sparing includes the presence of voluntary contraction of the external anal sphincter upon digital rectal examination.
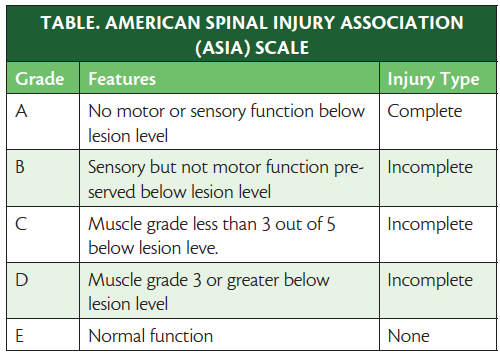
ASIA Impairment Scale- used in grading the degree of impairment
The ASIA Impairment Scale is a system used to classify the severity of spinal cord injury. It was developed by the American Spinal Injury Association in 2006 and is the most widely used classification system today.
| Level | Description | Presentation |
| A | Complete | No motor or sensory function is preserved in the sacral segments S4-S5. |
| B | Incomplete | Sensory but not motor function is preserved below the neurological level and includes the sacral segments S4-S5. |
| C | Incomplete | Motor function is preserved below the neurological level and more than half of key muscles below the neurological level have a muscle grade less than 3. |
| D | Incomplete | Motor function is preserved below the neurological level and at least half of key muscles below the neurological level have a muscle grade of 3 or more. |
| E | Normal | Motor and sensory functions are normal. |
A = Complete. No sensory or motor function is preserved in the sacral segments S4-S5.
B = Sensory incomplete. Sensory but not motor function is preserved below the neurological level and includes the sacral segments S4-S5, AND no motor function is preserved more than three levels below the motor level on either side of the body.
C = Motor incomplete. Motor function is preserved below the neurological level**, and more than half of key muscle functions below the single neurological level of injury have a muscle grade less than 3 (Grades 0–2).
D = Motor incomplete. Motor function is preserved below the neurological level**, and at least half (half or more) of key muscle functions below the NLI have a muscle grade >3.
E = Normal: If sensation and motor function as tested with the ISNCSCI are graded as normal in all segments, and the patient had prior deficits, then the AIS grade is E. style=”background-color: yellow;”>Someone without a SCI does not receive an AIS grade.
**For an individual to receive a grade of C or D, i.e. motor incomplete status, they must have either (1) voluntary anal sphincter contraction or (2) sacral sensory sparing (at S4/5 or DAP) with sparing of motor function more than three levels below the motor level for that side of the body. The Standards at this time allows even non-key muscle function more than 3 levels below the motor level to be used in determining motor incomplete status (AIS B versus C).
Note: When assessing the extent of motor sparing below the level for distinguishing between AIS B and C, the motor level on each side is used; whereas to differentiate between AIS C and D (based on proportion of key muscle functions with strength grade 3 or greater) the single neurological level is used.
Zone of partial preservation (ZPP):
The ZPP is used only with complete injuries (AIS A) and refers to those dermatomes and myotomes caudal to the sensory and motor levels that remain partially innervated. The most caudal segment with some sensory or motor function defines the extent of the sensory or motor ZPP respectively and should be recorded for the right and left sides and for sensory and motor function. A single segment (not a range of segments) is designated on the worksheet for each of these. For example, if the right sensory level is C5, and some sensation extends from C6 through C8, then “C8” is recorded in the right sensory ZPP block on the worksheet. If there are no partially innervated segments below a motor or sensory level, the motor and sensory level should be entered in the box for the ZPP on the worksheet.
Note that motor function does NOT follow sensory function in recording ZPP, but rather the caudal extent of the motor ZPP must be based on the presence of voluntary muscle contraction below the motor level. In a case of where the motor, sensory, and therefore NLI is T4, with sparing of some sensation at the left T6 dermatome, T6 should be entered for the left sensory ZPP, but the box for motor ZPP should remain T4. Non-key muscles are not included in the ZPP.
With an incomplete injury, the ZPP is not applicable and therefore “NA” is recorded in the block on the worksheet.

| Syndrome | Mechanisms | Presentation | Photo/Video |
| Central Cord Syndrome – most common type of incomplete spinal cord injury | -Damage to the large nerve fibers that carry information from the brain to the spinal cord -Signals are reduced but not entirely blocked -Caused by trauma to the neck, herniated disks, narrowing of the spinal column due to age |
-Paralysis or loss of fine motor control in the hands and arms -Milder loss of control in the legs -Loss of sensation below the level of injury and loss of bladder control may also occur |
A doctor explains the symptoms of Central Cord Syndrome in a real patient.
|
| Brown-Sequard Syndrome | -Lesion in the spinal cord -Caused by a tumor, puncture wound to the neck or back, tissue death due to an obstructed blood vessel, or infectious or inflammatory disease |
Weakness or paralysis occurs on one side of the body while loss of sensation occurs on the opposite side. | A doctor explains the symptoms of Central Cord Syndrome in a real patient.A man with Brown-Sequard syndrome moves from a wheelchair to the floor during a physical therapy session. |
| Anterior Cord Syndrome -Also called Beck’s Syndrome or Anterior Spinal Artery Syndrome |
-Caused by occlusion of the anterior spinal artery -Damage occurs to the anterior two thirds of the spinal cord while the posterior third is not damaged -May result from atherosclerosis, aortic blockage, external compression from a herniated disk or other cause, or trauma such as a stab wound. |
-Complete paralysis of motor functions below the level of the lesion -Loss of sense of pain and temperature below the lesion -Intact sense of proprioception, vibration, and 2 point discrimination -orthostatic hypotension -possible bladder, bowel and sexual dysfunction |
A man with anterior cord syndrome demonstrates his movement limitations. |
| Tethered Spinal Cord Syndrome (Conus Medullaris) | -Tissue attachments form within the spinal column that limit the movement of the spinal cord within the column -May be congenital, closely linked to spina bifida -May be caused by scar tissue secondary to spinal cord injury |
-Lower extremity weakness, pain, sensory loss, problems with bowel and bladder function -Children may have lesions, fatty tumors, hairy patches, or dimples on the low back |
Interview with a man diagnosed with tethered cord syndrome, with film clips of movement before and after treatment. |
| Cauda Equina | -Complication secondary to a ruptured disc -Material from the disc is pushed into the spinal canal, compressing the lumbar and sacral nerve roots |
Loss of bowel and bladder control, loss of sensation below the level of the lesion. May lead to paralysis. | A man with autism receives physical therapy for Cauda Equina syndrome.
|
Resources:
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3232636/
https://geekymedics.com/dermatomes-and-myotomes/
https://www.physio-pedia.com/Myotomes#cite_note-2