 …
…
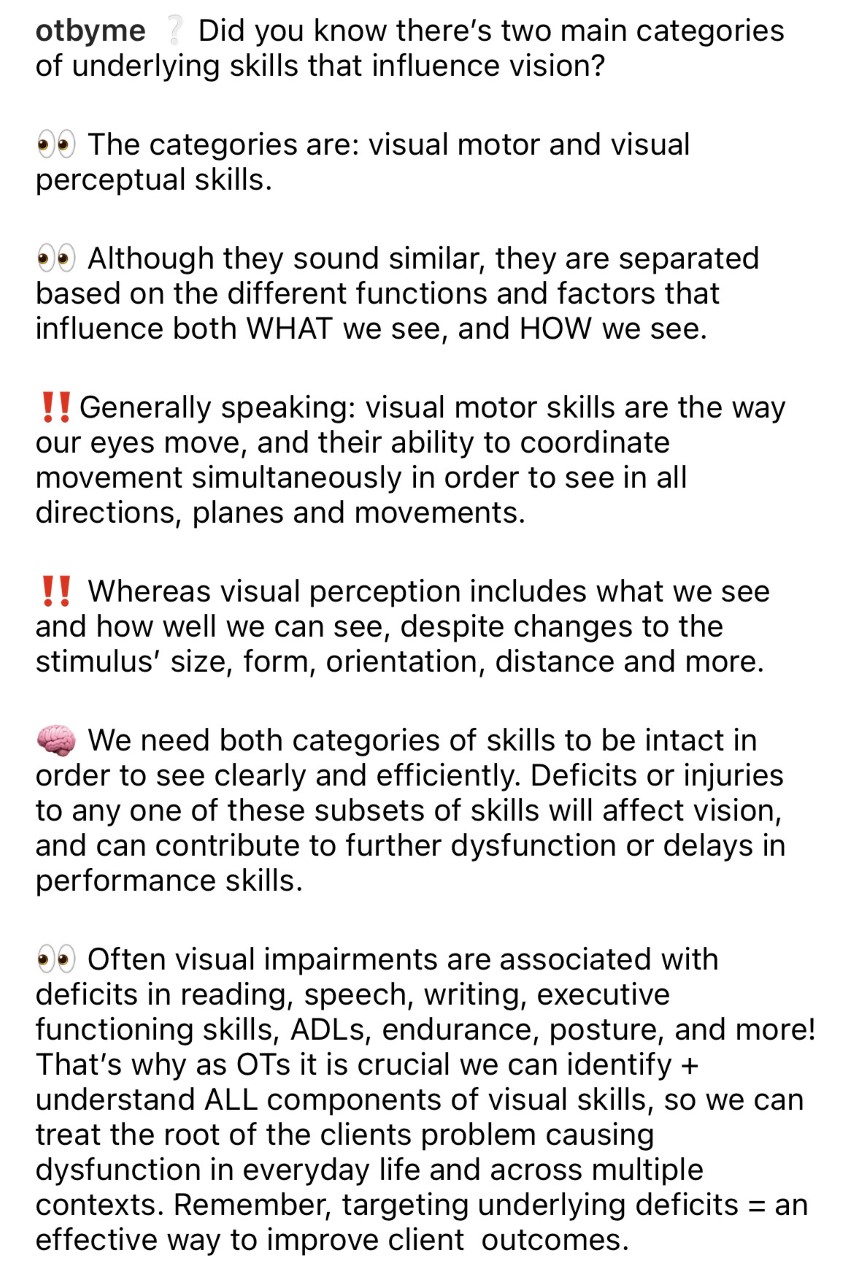
VISION
 …
… 
The following charts review the anatomy of the eye and the more common conditions that can lead to visual impairment, as well as the roles of health care professionals in the treatment of low vision and therapeutic interventions for low vision.

Photoreceptors- 2 Types
Rods – responsible for night and black/white vision, peripheral vision
Cones- responsible for color, fine detail, central vision (the MACULA has the highest concentration of cones)
Anterior Chamber- 7 parts of the anterior chamber/segment of the eye
● Sclera: white part of eye
● Iris: colored part of the eye that adjusts the size of the pupil.
● Cornea: the clear front surface of the eye.
● Pupil: the dark part of the eye that allows light in to reach the lens.
● Lens: the clear part behind the pupil that focuses light.
● Ciliary body: an extension of the iris that produces vitreous humor
● Vitreous humor: a clear fluid that fills the space between the lens and the retina.
Posterior Chamber
The FUNDUS aka the Posterior chamber of the eye is the interior surface, opposite of the lens, includes the retina, optic disc, macula, and fovea.
● Retina: the inner layer of tissue of the eye that creates a focused image and sends it to the brain.
● Optic Disc: the raised disc on the retina located where the optic nerve connects. There are no visual receptors on the optic disc.
● Macula: the functional center of the retina.
● Fovea: the center of the field of vision, located in a small depression in the retina. Visual acuity is the highest in the fovea.
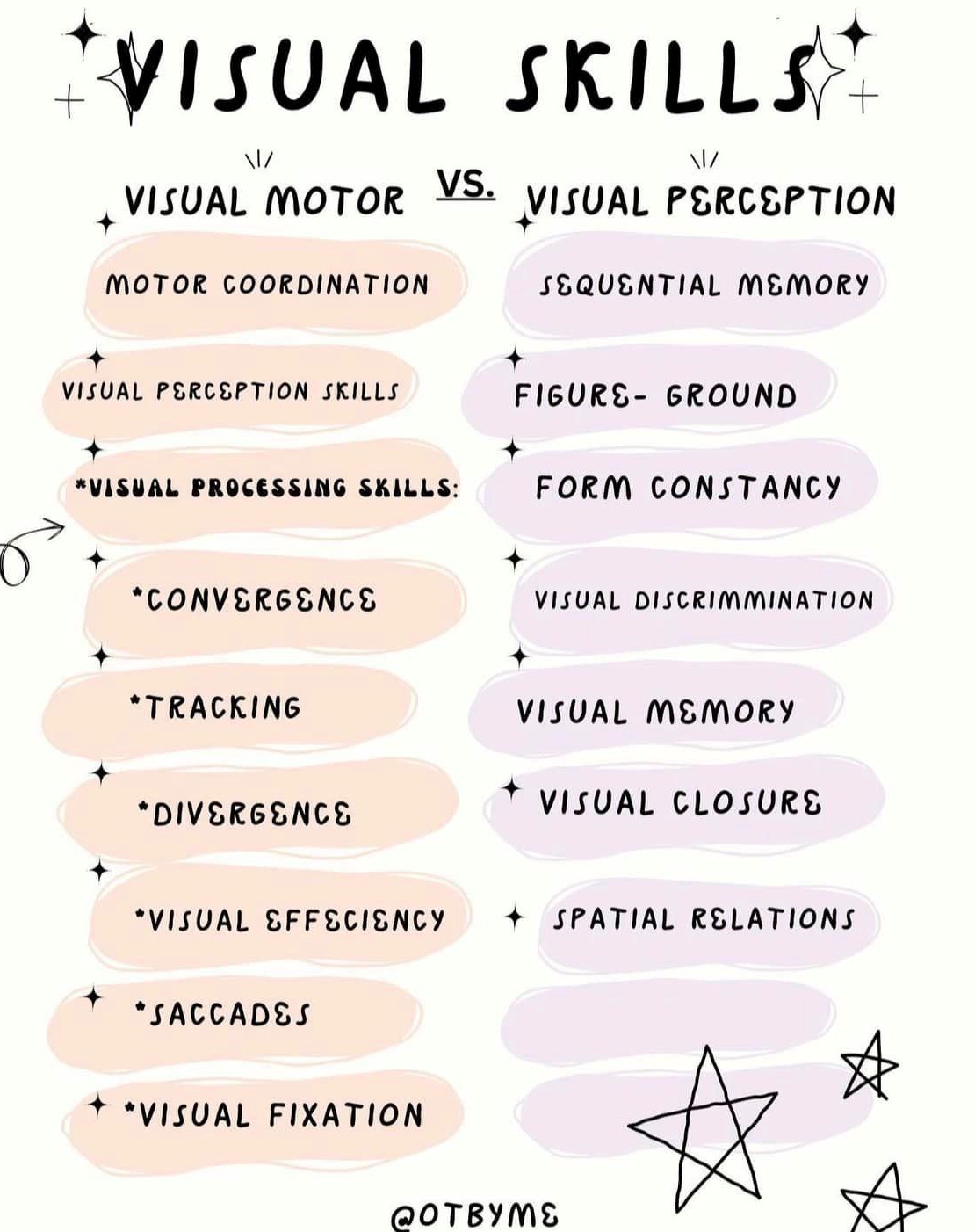
| Condition | Causes | Symptoms | Treatment | Photo – simulated vision |
| Hyperopia – also called farsightedness | The eyeball is too short or the cornea is too flat, causing light entering the eye to not focus correctly. | Objects that are close to the eye appear blurry, while those that are far away are clear. Symptoms may also include difficulty concentrating on work that is close, eye strain, headaches, fatigue, aching or burning eyes, or irritability after sustained concentration. | Correctable with glasses, contact lenses. |  |
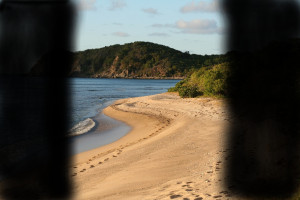
| Myopia – also called nearsightedness | The eyeball is too long or the cornea has too much curvature, causing light entering the eye to not focus correctly. | Objects that are far away appear blurry, while those that are close are clear. Common symptoms include difficulty seeing signs while driving, watching movies in a theater, or seeing the chalkboard in school. | Correctable with glasses, contact lenses or various forms of Lasik surgery. |  |
| Cataracts | Clouding of the lens due to changes in lens proteins, often due to age. | The lens becomes opaque. Loss of visual acuity, visual distortion, darkening of vision, cloudy or blurry vision. Lights may seem too bright or there may be a halo around lights. Other symptoms include poor night vision, double vision, and increased nearsightedness. Colors may seem faded. Contrast sensitivity is reduced. | Early cataracts are managed with adaptations including glasses, magnifiers, and bright lighting. Advancing cataracts that limit functional vision must be removed surgically. |  |
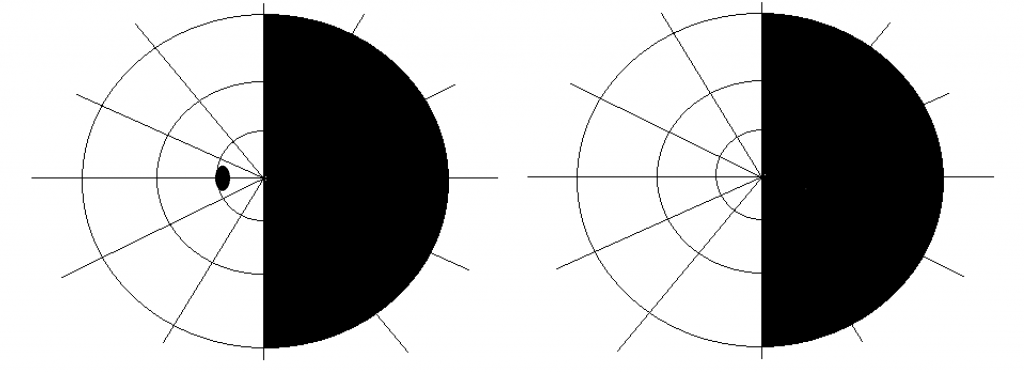
| Glaucoma | The term used for a group of disorders in which the common characteristic is increased intraocular pressure (IOP) with associated optic neuropathy. -Most commonly associated with increased fluid pressure in the eye. -Ocular hypertension occurs when IOP is consistently high, without any optic nerve damage. -Normal or low tension glaucoma occurs when optic nerve damage is present, but IOP is normal or low. |
Symptoms may vary depending on the type of glaucoma:
Acute angle-closure glaucoma: Open-angle glaucoma: |
Eye drops, oral medications, laser and other surgeries are used to relieve IOP. Acute angle-closure glaucoma is an emergency condition and requires emergency procedures.
Damage caused by glaucoma is not reversible. The condition may lead to permanent blindness. -A person with glaucoma must compensate for tunnel vision by moving his or her head and body around to view peripheral visual areas. |
 |
| Macular degeneration | Degeneration of the macula, due to age. Types: –Dry age-related macular degeneration (AMD) – gradual breakdown of the cells in the macula, resulting in progressive blurring of central vision. Also called “blue eyed disease” as people who are caucasian with light eyes are at higher risk of developing the disease. –Wet AMD – angiogenesis causes newly created abnormal blood vessels to grow under the center of the retina. The blood vessels leak, bleed and scar the retina, distorting or destroying central vision. |
Loss of central vision. Other symptoms include sensitivity to glare and difficulty with light changes. Some peripheral vision may remain intact. Dry AMD – blurred vision, need for increased light, difficulty recognizing faces. Wet AMD – straight lines appear wavy. |
Dry AMD – not treatable, but progression can be slowed through a healthy lifestyle and antioxidant vitamins.
Wet AMD – can be stopped or slowed with injections of anti-angiogenic agents into the eye. Laser surgery to cauterize leaking blood vessels is also an option. Treatment must be provided quickly to minimize vision loss, which can be rapid. Patients may compensate for central vision loss by turning the head and body to use peripheral vision using another, unaffected point on the retina. Called Eccentric Viewing Techniques or Pseudo Fovea training. Other treatments include Amsler Grid training, device training to compensate for visual acuity, environmental modifications, and patient education. Support groups help with adjustment. |
 |
| Diabetic retinopathy | Detachment of the retina or damage to the retinal capillaries. Occurs secondary to diabetes. | Blurry or fluctuating vision, “floaters” in the visual field (dark spots or strings), impaired color vision, and dark, patchy areas of visual loss within the visual field. Reduced contrast sensitivity. | Careful management of diabetes can slow progression. Advanced stage leads to permanent blindness. Treatments can include Amsler Grid training, Eccentric Viewing, special tinted glasses to reduce glare and sharpen acuity, environmental modifications, electronic magnification devices, com class=”blur” munity resource training. |  |
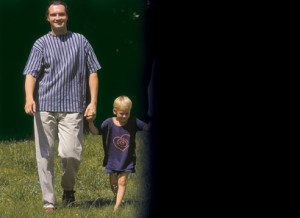
| Homonymous Hemianopsia | Damage to the visual centers of the brain that correspond to one half of the visual field in each eye. The most common cause is cerebrovascular accident (CVA or stroke). May also occur after traumatic brain injury or brain damage from seizures. -Often confused with visual field neglect, which is inattention to one side of the visual field. Hemianopsia may occur concurrent with visual field neglect, or the conditions may occur separately. |
Loss of vision in half of the visual field. Vision is lost in the same half of each eye, while vision is retained in the opposite half of each eye. Loss of visual field is on the same side as physical impairments, such as hemiparesis. | Eye movement therapy and compensation techniques. Experimental treatments to restore vision are currently under investigation, but there is no established method to reverse the condition. |  |
| Diplopia – also called double vision | Multiple possible causes, including damage to the cornea, lens, eye muscles, brain, and nerves that innervate the eye. Diplopia is often a symptom of another health condition. | Two images of the same thing are seen, either side by side or one on top of the other. Other symptoms may include misalignment of one or both eyes (i.e. “cross-eyed), pain around the eyes, pain with eye movement, droopy eyelids, eye weakness, headache, nausea. | Treatment is dependent on the underlying cause of the double vision. Medications may be used if the underlying cause of the double vision is another medical condition. If eye muscles are weak or misaligned, corrective surgery may be used. If surgery will not correct double vision, other methods such as eye patching or using prism glasses may help to correct or reduce the problem. |  |
MACULAR DEGENERATION VS GLAUCOMA
Mnemonic for remembering the difference:
Macular Degeneration is central and Glaucoma is peripheral
Macular as “middle” (M for middle) and glauCOMA as “corner” (C for corner)
Glaucoma is the only vision condition with tunnel vision. So, it’s unique in that way – glauComa like a cave, so it’s tunnel vision.
Draw 2 circles one with a G and one with an M.
The M takes up more room and the middle. That’s the vision that is impacted.
The G goes around the outside! That’s the vision that is impacted.
HEMIANOPIA (also called hemianopsia)
Partial or complete loss of vision in one half of the visual field(s) of one or both eyes. Diminished vision or full vision loss in the left or right half of the visual field of one or both eyes.
Types of hemianopia- each named depending on the region of the visual field that is affected
1. Homonymous hemianopsia
Refers to a visual defect that affects both eyes equally and occurs either to the left or right of the midline of the visual field. It is a visual field defect involving either the two right or the two left halves of the visual fields of both eyes. This is the most common pattern of vision loss.
2. Bitemporal hemianopia – bilateral loss of vision in the temporal fields
3. Altitudinal hemianopia– characterized by a visual defect above or below the horizontal meridian of the visual field.
 -Inferior hemianopia: When loss of vision occurs in the lower visual field of either the left, right, or both eyes.
-Inferior hemianopia: When loss of vision occurs in the lower visual field of either the left, right, or both eyes.
 – Superior hemianopia: When loss of vision occurs in the upper visual field of either the left or right eye or both.
– Superior hemianopia: When loss of vision occurs in the upper visual field of either the left or right eye or both.
4. Binasal hemianopia– loss of vision in the nasal hemifields of both eyes.

5. Quadrantanopia– loss of vision in one quarter of the visual field in one or both eyes.

Clinically
• Lesion of right optic tract will cause visual field defect on the left side, i.e. left homonymous hemianopia.
• Parietal lobe lesion will cause inferior homonymous quadrantanopia.
• Temporal lobe lesion will cause superior homonymous quadrantanopia.
Symptoms of homonymous hemianopsia
• Bumping into or failing to notice things on the side of the hemianopsia. This can make such everyday tasks as crossing the street or driving a car unsafe.
• Missing parts of words or parts of an eye chart on the side of the hemianopsia when reading.
• Not noticing objects on a desk or table, or even food on a plate to the side of the hemianopsia.
• Frustration with reading because it is difficult for the eyes to pick up the beginning of the next line.
• Tendency to turn the head or body away from the side of the hemianopsia.
• Drifting in a direction away from the hemianopsia when walking.
• Visual hallucinations that appear in the form of lights, shapes, or geometric figures or as the image of a recognizable object. Sometimes a movement noted on the normal side of vision is believed to be also seen at the same time on the side of the visual loss.
| Profession | Description | Video |
| Optometrist | Primary healthcare provider who examines, diagnoses, and manges diseases and disorders of the visual system, the eye and associated structures and diagnoses related systematic conditions. Treatment includes: prescription eyeglasses, contact lenses, eye drops and other medications. This is the doctor you go to for your annual check up. | An optometrist describes her job and demonstrates how she works with patients. |
| Ophthalmologist | Physician who specializes in the treatment of diseases and conditions of the eye and visual system that causes visual impairment. Their primary emphasis is on diagnosing the conditions causing vision loss and medically managing the condition either through SURGERY, pharmaceuticals, or optical devices. | An opthamologist explains the difference between ophthalmology and optometry to a news reporter. |
| Orientation & Mobility Specialist | Professional who evaluates and treats performance deficits associated with ambulating and traveling safely, efficiently, and confidently with visual impairment. Training may include developmental visual skills to guide movement in space, use of optical devices and travel aids (aka white cane training and sight dog training). | Orientation & Mobility teachers at a school for the blind explain the aspects of their jobs. |
| Low Vision Rehabilitation Specialist | Professional working in low vision who is certified to provide skilled vision rehabilitation therapy services. | Patients describe their experiences in a low vision rehabilitation program. |
| Teacher of the Blind and Visually Impaired | Professional who provides instruction and guidance to help persons with visual impairment acquire the compensatory skills and knowledge to manage their daily lives with the most highly attainable level of function. | A teacher of the blind and visually impaired explains her job to a news reporter. |
.
1. Amsler Grid
Used as a maintenance tool for clients with age related macular degeneration to monitor vision changes. Clients are instructed to test each eye at a time, then both, for any changes to how the grid typically looks. It is crucial to train patient in daily compliance of its usage!! If a client reports sudden onset of vision changes, they should be instructed to contact their physician immediately as this could be indication of Wet AMD (aka emergency situation!!)

2. Visual Acuity Charts (Snellen Chart)
20/20 vision is a term used to express normal visual acuity (the clarity or sharpness of vision) measured at a distance of 20 feet. If you have 20/20 vision, you can see clearly at 20 feet what should normally be seen at that distance. If you have 20/100 vision, it means that you must be as close as 20 feet to see what a person with normal vision can see at 100 feet.
Having 20/20 vision does not necessarily mean you have perfect vision. 20/20 vision only indicates the sharpness or clarity of vision at a distance. Other important vision skills, including peripheral awareness or side vision, eye coordination, depth perception, focusing ability and color vision, contribute to your overall visual ability.

3. Confrontational Testing for Visual Field Cuts
The visual fields of both eyes overlap; therefore each eye is tested independently. The patient should cover their right eye with their right hand (vice versa when testing the opposite eye). With the examiner seated directly across from the patient, the patient should direct their gaze to the corresponding eye of the examiner. The testing itself can be performed using stationary or moving targets (disk mounted on a stick or examiner’s fingers). To perform stationary testing, the examiner holds up a certain number of fingers peripherally, equidistant between the examiner and the patient. The patient is asked to correctly identify the number of fingers. All four quadrants (upper and lower, temporal and nasal) should be tested. Stationary targets are more precise because they present a finer stimulus to the retina and are less easily identifiable relative to a moving target. In addition, for unknown reasons, colored targets such as red or green discs are more sensitive in detecting deficits when compared to a white test object.
4. Contrast Sensitivity
Contrast sensitivity is a measure of how much a pattern must vary in contrast to be seen (compared with visual acuity, which measures how big an object must be to be seen). Contrast sensitivity is an important factor influencing the quality of vision. A decrease in contrast sensitivity function can lead to a loss of spatial awareness and mobility and increase the risk of injuries. Reduced contrast sensitivity may affect the ability to walk down steps, recognize faces, drive at night or in the rain, find a telephone number in a directory, read instructions on a medicine container or navigate safely through unfamiliar environments. Reading is also compromised, for example letters may be almost invisible if the print is too light. Environmental modifications, such as high contrast colors or strips on the first and last steps of staircases, contrasting colors on door frames and the use of contrast on electrical outlets, can all improve patient safety. Decreased contrast sensitivity function is associated with ocular pathological conditions such as a cataract, age-related macular degeneration, diabetic retinopathy, glaucoma and optic nerve degenerations.

5. Clock Drawing Test for visuospatial deficits and cognition
The Clock Drawing Test (CDT) is a nonverbal screening tool in which the patient is asked to draw a clock. Although there are multiple versions of this test, in general, they all ask the patient to draw the face of a clock and then to draw the hands to indicate a particular time. Placement of the numbers around the circle requires visual-spatial, numerical sequencing, and planning abilities.

| Test Name | What it Evaluates | Administration | Video |
| Pursuit/Tracking | The ability of the eyes to track moving objects within the visual field. | The client is asked to focus on an object and then follow that object with the eyes as the therapist moves it in all planes. The therapist watches for coordination of eye movements and any deviation of gaze from the object. | A young girl is tested for visual pursuit. |
| Convergence | The alignment of the eyes during near distance tasks. | The client is asked to look at a small stationary object, such as the eraser on a pencil. The therapist then moves the object in a straight line toward the bridge of the client’s nose. The client reports or signals when they see two of the object (see double). The distance from the bridge of the nose to the object is measured. The therapist watches for any deviation of one or both eyes away from the object during the test. | A young girl is tested for near point convergence. |
| Saccades | The ability of the eyes to quickly jump from one area of focus to another. | The therapist holds up two fingers or two small objects. The therapist identifies the objects for the client (usually left/right, red/blue or something similar) and instructs the client to look at the object when the therapist says the name of it. The therapist will then alternate stating the names of the objects, first slowly, then faster, until the client is moving his or her eyes back and forth at a rapid speed. The therapist watches for difficulty moving the eyes and deviation from the objects. | A young girl is tested for saccades. |
| Peripheral vision | The ability to see motion from the sides of the eyes. | The therapist will instruct the client to look straight ahead and signal when an object can be seen “out of the corner” of the eye. The therapist will then move an object around the client’s head from the back until the client signals that the object is seen. The therapist will measure the angle between 0 and 90 degrees at which the object is seen. | Students demonstrate a method for testing peripheral vision. |
| Visual field loss, also called confrontational testing. | Whether a visual field cut exists and the severity of that field cut. | The therapist sits in front of the client and moves a finger or an object through the visual planes. The therapist asks the client to report if the object is seen in different locations and watches for loss of visual pursuit. A test of peripheral vision may also be a part of this test. | Confrontational peripheral vision testing is demonstrated. |
Occupational Therapy Interventions for:
a. Low Vision
Occupational therapy intervention for low vision primarily consists of providing adaptations to compensate for vision loss. Most therapists try low tech, low cost interventions with their clients first before introducing higher tech options.
Some of the more common interventions include:
-Increase the level of lighting in areas where activities will occur.
-Use adjustable window treatments (curtains, blinds, shades, drapes) to allow for the adjustment of natural light.
-Place chairs near windows to allow for reading or craft work using natural light.
-Reduce glare, including adjusting the location of mirrors. Use non-skid, non-glare cleaning products on floors.
-Increase contrast, such as placing a dark bath mat on a white bathroom floor or bright orange tape on the edge of a dark step. Use light colored door handles on dark colored doors and vice versa.
-Clear walkways and reduce clutter in common areas.
-Tape down or remove rugs and electrical cords.
-Increase font size during reading, including use of large print books and adjusting computer monitor settings.
-Recommend textured upholstery on furniture to provide tactile cues for seat location.
-If making recommendations for a public hallway, recommend that drinking fountains, fire extinguishers, and other obstacles be located along the same wall, leaving the other wall clear.
-Light stairwells clearly to reduce shadows and glare. Mark landings with a highly contrasting color.
-Mark emergency exits clearly.
In this video, an occupational therapist explains treatment interventions for people with visual impairments:
b. Unilateral Neglect

Unilateral neglect is an attention disorder that arises as a result of injury to the cerebral cortex.
Unilateral neglect is also commonly known as:
• Contralateral neglect
• Visuospatial neglect
• Spatial neglect
• Hemineglect
The defining characteristics of unilateral neglect are:
• Consistent inattention to stimuli on the affected side
• Inadequate self-care
• Lack of looking toward the affected side
• Leaving food on the plate of the affected side
 The Lighthouse Technique
The Lighthouse Technique
The lighthouse technique combines mental imagery and attention training to address unilateral neglect. It is both an evidence-based cognitive rehabilitation intervention and a compensatory strategy for improving unilateral neglect.
The lighthouse strategy combines three strategies (anchor, guide, scan) to help the person scan, plan, and implement functional tasks.
When training a patient to use these strategies, the OT practitioner should grade the functional activities. Start with simple, easy-to-accomplish tasks and gradually increase their length and complexity. For example, the therapist might start scanning or reading tasks with only a few lines that are in large font and gradually increase the difficulty by having the person read more lines with smaller font. The therapist may also grade the cues starting with maximum verbal cues and advancing to self-cueing for ultimate independence in daily functioning.
| Device | Use | Example | Photo/Video |
| Magnifiers | Used to enlarge print or objects within magnified field. -hand held – magnifies a small, defined area -sheet – magnifies an entire page -hands free – mounted on a table or desk, hung around the neck, or worn as glasses. Used for small piece work, needlework, etc. |
A woman with cataracts uses a magnifier with a neck mount and strap to complete a cross stitch project. |  |
| Low vision lighting | Used to provide extra lighting for reading or small piece work. May be hand held, mounted, or incorporated into a magnifier. | A man with early macular degeneration uses a head lamp while tying fishing flies. | 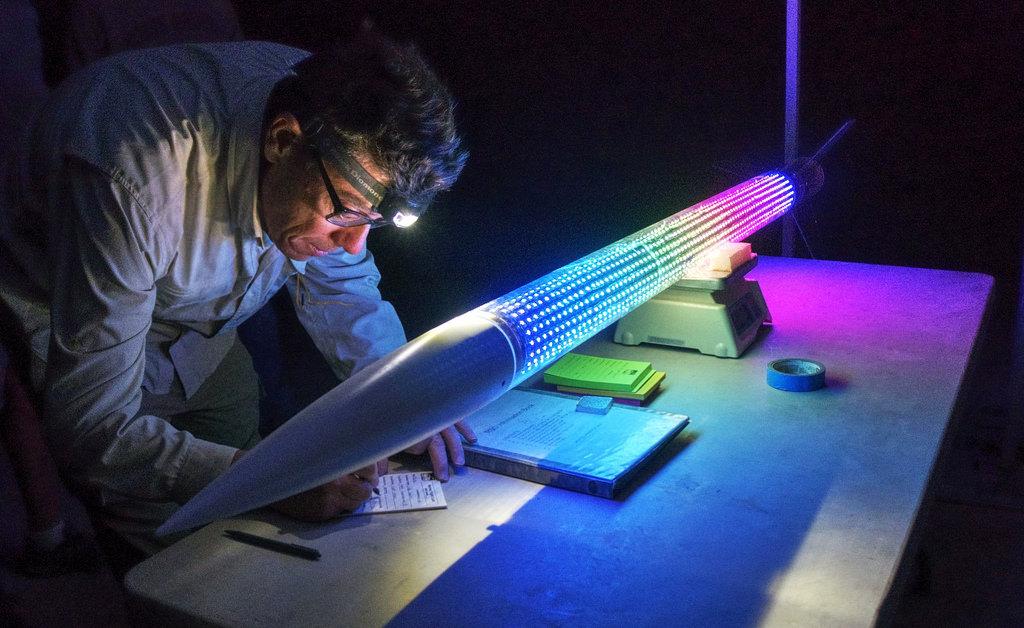 |
| Adaptive clocks | Clocks that use audio output to announce the time and vibration to provide alarms. | A man with severe visual impairment and hearing loss uses a vibration attachment on an adaptive clock to shake his bed, waking him up on time. |  |
| Audio books | Books read aloud and recorded specifically for the visually impaired. People with severe visual impairments can qualify to get audio players and books in specific formats at no cost to them. | A woman with permanent blindness listens to her textbook in DAISY (Digital Audio-based Information System) format on a DAISY audio player. |  |
| Talking and low vision devices | Devices that provide audio output or large print on the controls. Calculators, television remote controls, personal organizers, telephones, timers, daily living devices, and other devices are available with these adaptations. | A man with glaucoma uses a large button remote control to switch channels on his television. |  |
| Labelers | Label makers that use Braille, large print or audio tags to label clothing and other items. | A woman with permanent blindness uses a Braille label maker to label her clothing according to color and style. |  |
| Assistive Technology | These items include adaptations for low vision for computers, tablets, and smartphones. Adaptive display settings, downloadable or up-loadable adaptive software, adaptive keyboards, computer screen magnifiers, and book readers are examples. People with severe visual impairments might require screen reading software. | A woman with severe hyperopia uses the adaptive settings in her work computer software to enlarge the print on the screen. |  |
VISUAL PERCEPTION
. 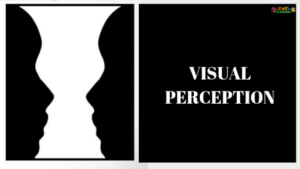
Visual Perceptual skills involve the ability to organize and interpret the information that is seen and give it meaning.
Visual Perceptual Skills
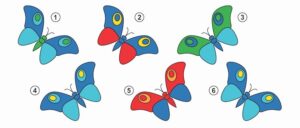
1. Form constancy.
The ability to recognize and label objects even when they are viewed from a different angle or in a different environment.
2. Figure Ground
The ability to focus on one specific piece of information in a busy background. To see an object in a busy background.
3. Visual closure
The ability to correctly perceive an object or word, even when it is partly hidden.
This ability helps you to quickly make sense of what you see, even if it is not all visible to you, which means you do not have to see every little detail in order to recognize something.
4. Visual memory
The ability to store visual details in short-term memory and to recall the visual details of what you have seen.
5. Spatial Orientation
The ability to identify the position or direction of objects or points in space. Position in space (relates to understanding directional language concepts, such as in/out, up/down, in front of/behind/between, left/right, when relating to objects or shapes such as letters).
6.Visual discrimination
This is the ability to see subtle differences between objects or pictures. This visual perceptual skill can be described as “paying attention to detail”.
7. Spatial Relationships
This is the ability to visually perceive two or more objects in relation to each other and to yourself.
| Deficit | Clinical Observations | Picture |
| Form Constancy | • Difficulty recognizing shapes, numbers, and letters when they differ in either color, size, font, or when they are presented in a different context • Difficulty recognizing people wearing different clothing |
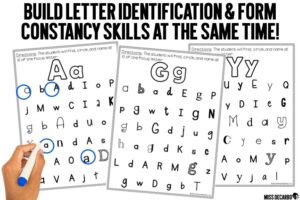 |
| Figure Ground | • Difficulty locating clothing in drawers during ADLs • Missing road signs or vehicles when driving • Unable to locate toys in a toy box • Struggles to find information on a busy blackboard • Loses place when copying work from the board • Loses place on the page while reading • Struggles with navigating around a map |
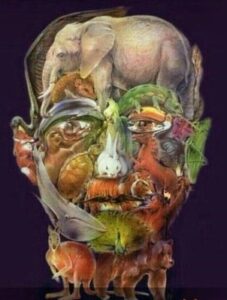 |
| Visual Closure | • Cannot identify traffic signs that are partially hidden behind a tree or other vehicle • Difficulty locating items in the refrigerator that are partially covered • Difficulty making sense of words on a smudged page • Difficulty recognizing an object even when you can only see part of it • Difficulty finding an item of clothing when it is partly hidden |
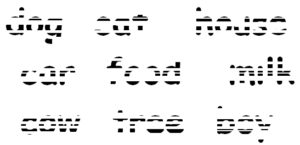 |
| Visual Memory | • Difficulty remembering faces or new people • Reading comprehension is affected when visual memory is deficient • Difficulty recalling a phone number that has just been read • Difficulty remembering sight words • Difficulty copying work from the board or a book |
 |
| Spatial Orientation | • Letter and number reversals | 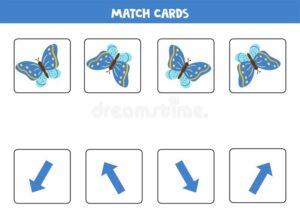 |
| Visual discrimination | • Struggles to match clothing, socks, or cutlery, especially when the differences are subtle • Struggles to see the difference between similar objects (e.g., coins) • Struggles to see differences between similar looking letters and words (eg b / d, b / p, 5 / s, won’t / want, car /cat) |
 |
| Spatial relationships | • Difficulty understanding what it means to “stand first in a line”, “sit in front of Amy” or “put the pencil on top of the paper”. • Difficulty with spacing and organization of written school work • Difficulty with writing on the line/in relation to the lines • Standing in line without bumping into others |
 |
| Test Title | Skills Measured | Administration | Norms | Links |
| Beery Buktenica Developmental Test of Visual-Motor Integration (Beery VMI) | Integration of visual and motor abilities. | The client is asked to copy a series of geometric forms that progress in difficulty. | Norms for ages- Full Form: 2 to 100 years; Short Form: 2 to 7 years | Commercial description of the Beery VMI. |
| Test of Visual-Perceptual Skills (TVPS) | Non-motor visual perceptual skills, including: -visual discrimination -visual memory -visual-spatial relationships -form constancy -visual-sequential memory -visual closure -figure-ground |
The client is asked to match geometric figures through pointing or stating a multiple-choice answer. | Two sets of norms, one for age 4 to 13 and one for age 12 to 18. | Commercial description of the TVPS. |
| Motor-Free Visual Perception Test (MVPT) | Non-motor visual perceptual skills, including: -visual discrimination -spatial relationships -visual memory -figure-ground -visual closure |
The client is asked to match geometric figures through pointing or stating a multiple-choice answer. | Norms for age 4 to 70+. The only non-motor visual perceptual test normed for ages across the lifespan. | Commercial description of the MVPT. |
| Occupational Therapy Adult Perceptual Screening Test (OT-APST) | Visual perceptual skills that may have been affected by stroke, including: -agnosia -body scheme -unilateral neglect -constructional skills -apraxia -acalculia -functional skills (reading, writing, arithmetic, telling time, holding and manipulating an object) |
The client completes a series of tasks related to each test area. | Two sets of norms, one for age 16 to 74 and one for age 75 to 97. | Administering the OT APST |
| Developmental Test of Visual Perception (DTVP) | Both motor and non-motor perceptual skills,,/span> including: -eye-hand coordination -copying -figure-ground -visual closure -form constancy The adult version also includes: -visual-motor search -visual-motor speed |
The client traces paths and copies geometric shapes in an answer booklet, as well as matching figures by pointing to or reporting the letter of multiple choice answers. | Two test are available:
Children’s version: normed for ages 4-0 to 12-11 Adolescent/Adult version: normed for ages 11 to 74 |
Commercial description of the DVTP. Commercial description of the DTVP-A. |
Low Vision Study Resources:
• Vision Aware – www.visionaware.org
• American Foundation for the Blind – www.afb.org
• AMD Alliance – www.amdalliance.org
• Eye Anatomy – www.eyecareamerica.org/eyecare/anatomy
• Occupational Therapy Toolkit – www.ottoolkit.com — HIGHLY RECOMMENDED! Not JUST for Low Vision but an invaluable tool for learning about interventions and tons of easy to read/understand patient education handouts
• https://www.myotspot.com/interventions-unilateral-neglect/
• https://www.medbridgeeducation.com/blog/2016/05/four-basic-strategies-to-improve-hemispatial-neglect/
• https://emedicine.medscape.com/article/2094663-technique
• https://www.sciencedirect.com/topics/medicine-and-dentistry/contrast-sensitivity
• https://miota.org/docs/Assessment_and_Intervention_of_Visual_Perception_and_Cognition3.pdf
• https://www.ot-mom-learning-activities.com/visual-perceptual-skills.html