 ….. . ………..
….. . ………..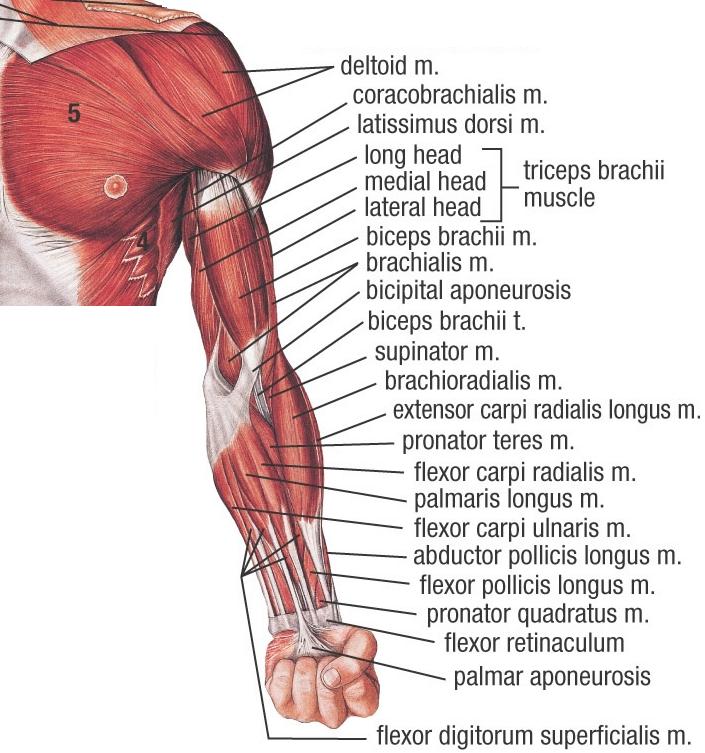
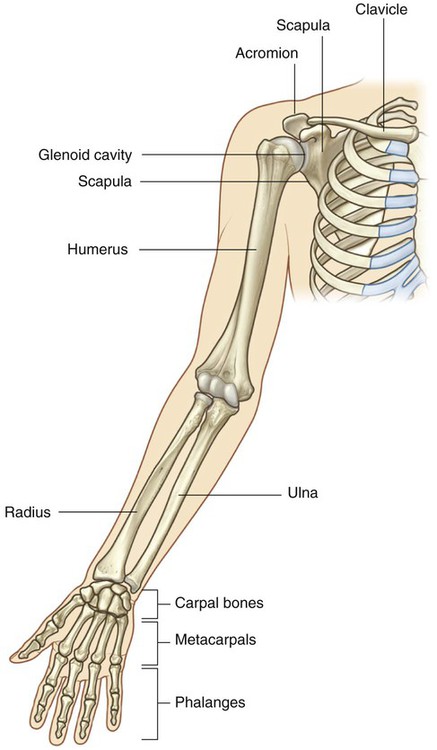
The following charts and illustrations will review conditions of the upper extremities, including the hands. These charts are organized by category of diagnosis.
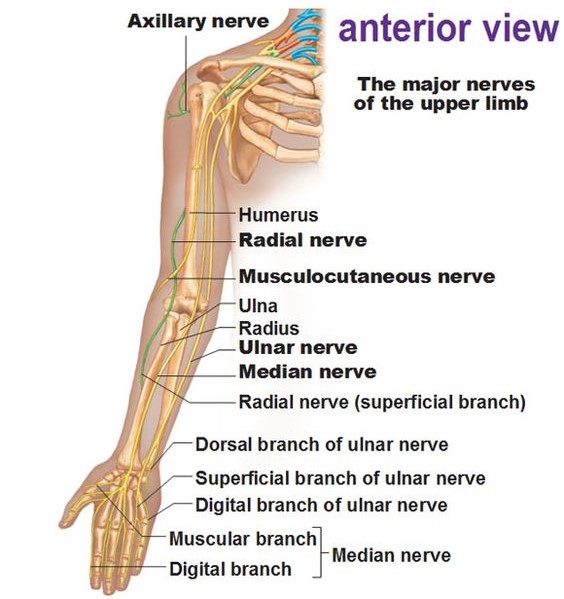
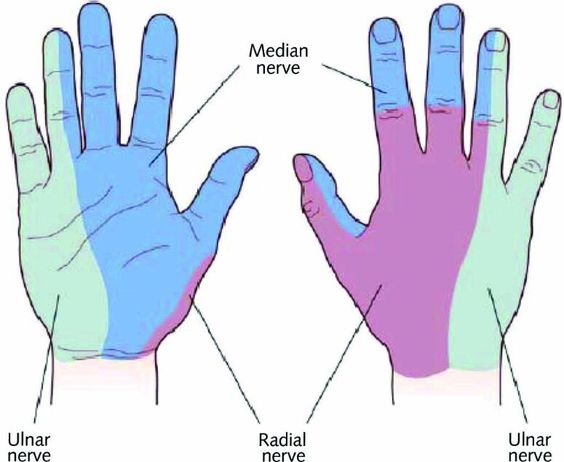
NERVE DISTRIBUTION OF THE UPPER EXTREMITY
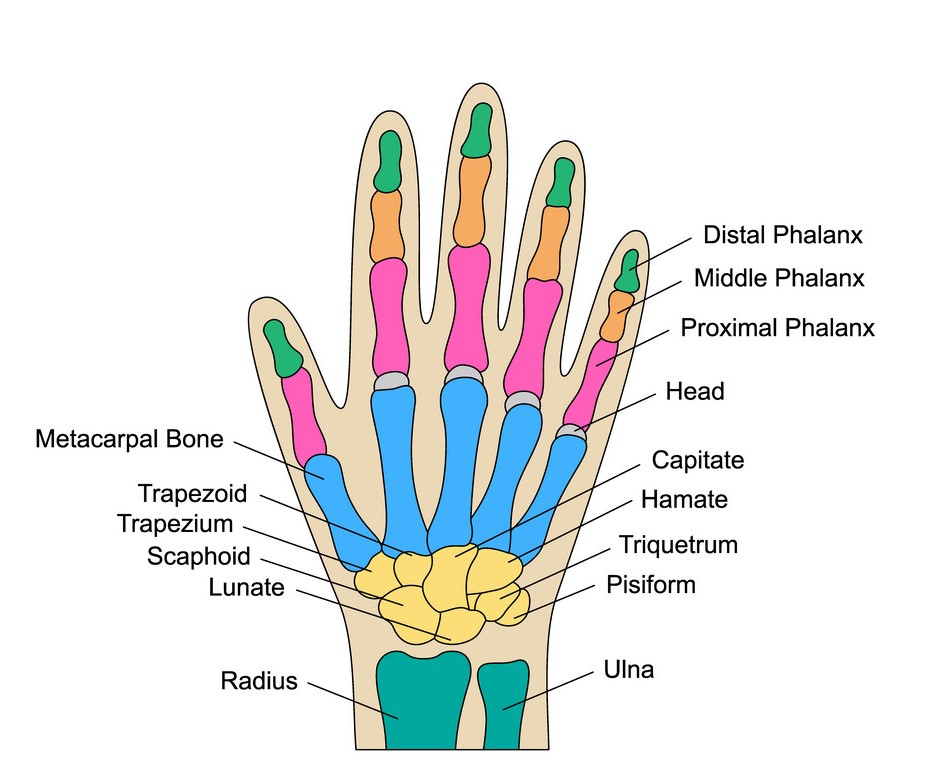
JOINTS OF THE HAND & NERVE DISTRIBUTION OF HAND – know both of these
 ……….
………. 
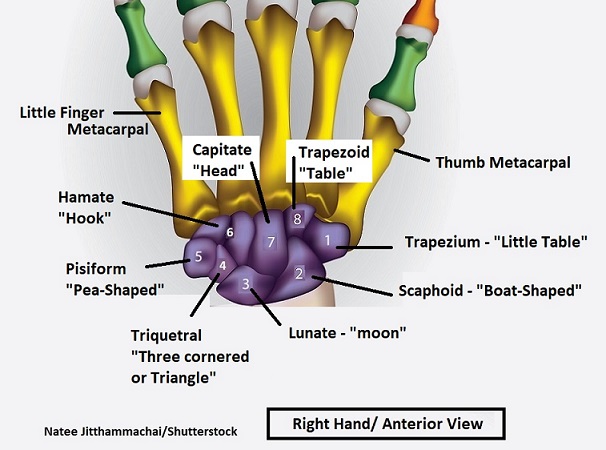
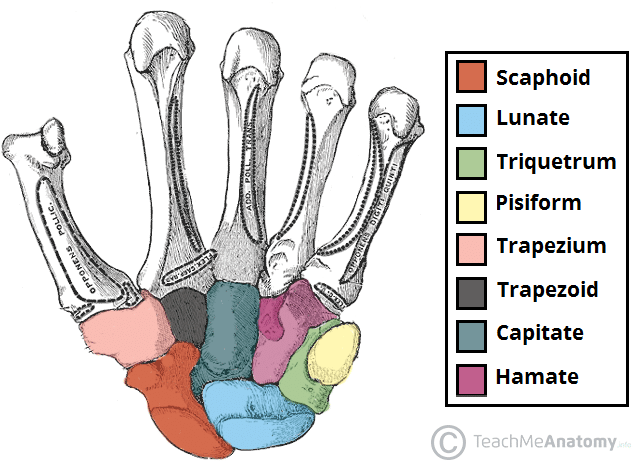
CARPAL BONES
The wrist, contains eight short bones are called carpals (named after Latin and Greek words meaning “wrist”). These bones have bizarre names, but that’s because they are named after ancient words related to their general shape:
 …
… 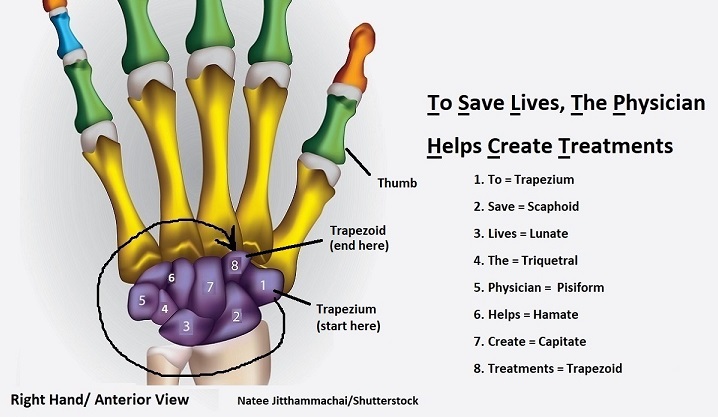
Test your knowledge: Can you identify the carpal bones with a different view?
.
Nerve Compression Syndromes – the nerve is compressed due to entrapment within other tissues, such as muscles, tendons and ligaments. The cause of nerve compression syndromes is most often poor positioning. Severity can range from mild to severe. Once a nerve is severely damaged due to compression, it may never fully recover. Deformities in the affected area may develop.
| Condition and Cause | Symptoms | OT Treatments for Conservative Management | OT Treatments for Post-Surgical Management | Contraindications | Photo |
| Carpal Tunnel Syndrome – caused by compression of the median nerve where it passes through the carpal tunnel. Result of inflammation or repetitive motion with poor positioning. | Palmar numbness and numbness of first digit to half of the fourth digit, with generalized weakness and pain, including pain at night. | Wrist splint with wrist positioned in neutral (Neutral wrist position causes less pressure on the carpal tunnel compared with extension), median nerve gliding exercises, activity modification, ergonomics. | Edema control, AROM, nerve/tendon gliding exercises, sensory re-education, strengthening, activity modification. Pillar pain is pain on either side of the carpal tunnel release surgery site. The source of the pain is unknown and may be ligamentous or muscular in origin. | Avoid repetitive motion, vibration to volar wrist. |  |
| Cubital tunnel syndrome – caused by compression of the ulnar nerve at the elbow. Result of repetitive pressure on the elbow or repetitive or sustained bending of the elbow. | Numbness and tingling along ulnar aspect of forearm/ hand, pain at elbow with extreme , weak power grip; + Tinel’s sign at elbow (pain or sensation) | Elbow pad or elbow splint to decrease compression of nerve, activity modification. | Edema control, AROM, nerve glides, strengthening, MCP blocking splint if clawing is noted. | Avoid movements or postures that aggravate symptoms. | 
|
| Double Crush Injury- occurs when a peripheral nerve is entrapped in more than one location. | Intermittent diffuse arm pain and paresthesias with specific postures. | Treat according to protocols for each nerve syndrome involved. For example, if the two syndromes involved are carpal tunnel syndrome and brachial plexus injury, treat each syndrome. | Treat according to protocols for each nerve syndrome involved, following the surgeon’s orders. |  |
|
| Guyon’s Canal Syndrome – occurs when the ulnar nerve is compressed as it passes through Guyon’s Canal at the wrist. Caused by inflammation or other irritation to the ulnar nerve at the wrist. | Numbness and tingling in ulnar nerve distribution of hand; motor weakness of ulnar nerve innervated musculature; + Tinel’s sign at Guyon’s canal. | Work activity modification, wrist splint in neutral. | Edema control, AROM, nerve glides, sensory re-education, strengthening. | 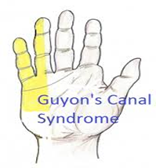 |
|
| Pronator Teres Syndrome – occurs when the median nerve is compressed between the two heads of pronator teres. Caused by trauma to the forearm or repetitive overuse, especially against resistance (i.e. turning a manual screwdriver.) | Palmar numbness and numbness of first digit to half of the fourth digit, with generalized weakness and pain, aching pain in the proximal volar forearm. No pain at night. | Pain control techniques, activity modification, adaptations, elbow splint at 90° with the forearm in neutral. | AROM, nerve gliding exercises, sensory re-education, strengthening 2 weeks post op. Activity modification, adaptations at work. | Avoid repetitive forearm pronation and supination |  |
| Radial nerve palsy – decreased conduction of the radial nerve. Causes include compression, fractures, and laceration. | Weakness/paralysis of extensors to wrist, MCPs, thumb; wrist drop; AKA Saturday night palsy. Slow nerve regeneration. | ROM, nerve gliding exercises, strengthening, Thumb Extension Splint, Duran dorsal protection splint, volar splint with wrist in neutral, dynamic extension splint | Scar management, passive and active ROM, edema control, sensory and motor re-education, strengthening per surgical protocol, activity modification. | Compression caused by fractures is usually treated surgically due to the risk of bony fragments lacerating the nerve. | 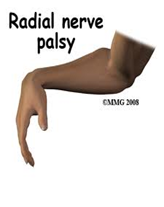 |
| Radial tunnel syndrome– compression of the radial nerve in the proximal forearm. Caused by inflammation, repetitive motion, injury to the lateral side of the elbow, or tumors. | Dull ache and burning sensation along the lateral forearm. | Long arm splint, with the wrist in extension, elbow in flexion, and forearm in neutral rotation, massage or TENS for pain management, pain free ROM, nerve gliding, activity modification | Long arm splint with the wrist in extension, elbow in flexion, and forearm in neutral rotation for 2 weeks, then wrist cock up for 2 more weeks, passive and active pronation and supination, hand strengthening exercise at 3 weeks, resistive exercise at 6 weeks. | Avoid forceful wrist extension and supination. |  |
| Thoracic outlet syndrome- occurs when excess pressure is placed on a neurovascular bundle passing between the anterior scalene and middle scalene muscles. Caused by repetitive motion in the upper arm and shoulder, injury, poor posture, anatomical defects, tumors, or pregnancy. | Vascular symptoms include: swelling or puffiness in the arm or hand, bluish discoloration of the hand, feeling of heaviness in the arm or hand, pulsating lump above the clavicle, deep, boring toothache-like pain in the neck and shoulder region which seems to increase at night, easily fatigued arms and hands, superficial vein distention in the hand. Neurologic symptoms include: paresthesia along the inside forearm and the palm (C8, T1 dermatome), muscle weakness and atrophy of the gripping muscles (long finger flexors) and small muscles of the hand (thenar and intrinsics), difficulty with fine motor tasks of the hand, cramps of the muscles on the inner forearm (long finger flexors), pain in the arm and hand, tingling and numbness in the neck, shoulder region, arm and hand | Modalities to reduce inflammation, such as ultrasound or Neuromuscular Electrical Stimulation. Strengthening of the muscles around the cervical spine and scapula. Wrist splints for postural retraining. | AROM and PROM, edema control, scar management, muscular reeducation to compensate for any muscles removed, postural retraining, activity modification. | Avoid heavy lifting, working with arms overhead, direct weight bearing on the shoulder. | 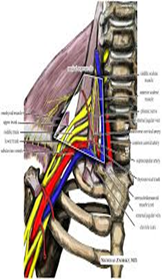 |
Nerve Laceration or Lesion – The nerve is partially or completely severed, or the nerve is damaged by trauma or prolonged compression.
| Condition and Cause | Symptoms | OT Treatments for Conservative Management | OT Treatments for Post-Surgical Management | Contraindications | Photo |
| Ape Hand Deformity – caused by either a high or low median nerve injury. If the median nerve is injured either proximally or distally, the ability to abduct and oppose the thumb will be lost due to paralysis of the thenar muscles.
**Ape hand deformity (simian hand), is not by itself an individual diagnosis. It is seen only after the thenar muscles have atrophied. Ape hand is the default position of the injured hand at rest. |
Loss of thumb abduction. Sensory loss in index, middle, and radial side of the ring finger; loss of pinch, thumb opposition, index finger MCP and PIP flexion; and decreased pronation. | PROM, prolonged stretch to counteract deformity. Strengthening exercises to build atrophied muscles of the thenar eminence, hand and forearm. C-bar splint with thumb positioned in opposition and fingers in a “C” position. | Gentle AROM, tendon gliding exercises, scar management techniques and soft tissue mobilization, splinting per tendon transfer protocols. PROM and strengthening added about 2 months after surgery. | No PROM or strengthening post surgery until authorized by the physician, per tendon transfer protocols. Strengthening too early can cause damage to the transferred tissues. | 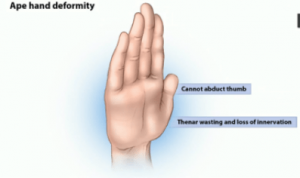 |
| Brachial Plexus Injury – The brachial plexus is a network of nerves that conducts signals from the spinal cord, which is housed in the spinal canal of the vertebral column (or spine), to the shoulder, arm and hand. These nerves originate in the fifth, sixth, seventh and eighth cervical (C5-C8), and first thoracic (T1) spinal nerves, and innervate the muscles and skin of the chest, shoulder, arm and hand. Brachial plexus injuries, or lesions, are caused by damage to those nerves. Can occur as a result of shoulder trauma, tumors, or inflammation. | Pain, including avulsion pain (a burning pain in the injured nerve area), loss of sensation distal to the brachial plexus, muscle weakness, partial or total paralysis of the affected upper extremity. | Passive and active ROM, sensation retraining including techniques to reduce tactile sensitivity, neuromuscular re-education as motor function returns. A flail arm splint provides the needed stability at both the shoulder and elbow for functional positioning of the hand. | Edema control, passive and active ROM, neuromuscular re-education to help the patient learn to recruit muscles in a different way, may use biofeedback training. Strengthening 4-6 weeks after surgery. Brachial plexus injuries may require several surgeries. | ROM is important to keep the affected limb mobile as recovery may take years. | 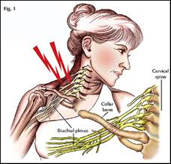 |
| C5 Spinal Cord Injury – the spinal cord is partially or completely severed at the level of the 5th cervical vertebra. | Movements possible: Shoulder, flexion, abduction, extension. Elbow flexion, supination. Scapular adduction, abduction. | AROM and strengthening of innervated muscles. PROM and splinting of hands to maintain functional position and prevent contracture. Wrist cock-up splint with universal cuff. |
Positioning, PROM, AROM, strengthening following any type of surgery performed. Address any return of function following surgery. | Monitor for muscle tightness and spasticity, initiate ROM and splinting before onset of contracture. |  |
| C6-C7 Spinal Cord Injury – the spinal cord is partially or completely severed at the level of the 6th or 7th cervical vertebrae | Movements possible: C6: Scapular protraction (partial horizontal adduction). Forearm supination. Radial wrist extension. C7: Elbow extension Ulnar/wrist extension. Finger extensions. Thumb flexion, extension & abduction |
Practice to allow the proximal interphalangeal (PIP) joints to develop a contracture to facilitate functional grasp. Ranging the hand (wrist extension combined with finger flexion and wrist flexion combined with finger extension) of a client with a spinal cord injury preserves a functional tenodesis grasp while encouraging PIP flexion contractures. Tenodesis splint. (Active wrist extension drives a hinge mechanism in the splint that allows thumb to fingertip pinch.) |
Positioning, PROM, AROM, strengthening following any type of surgery performed. Address any return of function following surgery. | Monitor muscle tightness and spasticity, but allow partial contracture to develop in PIP joints for tenodesis grasp. |  |
| Erb’s Palsy – Paralysis of the arm caused by injury to the upper group of the arm’s main nerves, specifically the severing of the upper trunk C5–C6 nerves. | The arm hangs limp with the shoulder rotated inward due to atrophy and paralysis in the biceps, deltoid, brachialis, and brachioradialis muscles. This significantly limits functional movement. The paralysis can either resolve on its own over a period of months, necessitate rehabilitative therapy, or require surgery.</s class=”blur”pan> | PROM, contracture management. Elbow lock splint stabilizes the elbow to enable the individual to position the hand closer to or away from his/her body for functional use. |
Edema control, scar management at surgical site, positioning. | Monitor for subluxation of the shoulder, frozen shoulder, contractures. |  |
| Long Thoracic Nerve Palsy – the long thoracic nerve sustains damage, causing pain and limited movement in the shoulder. | Shoulder pain, limited overhead movement, and abnormal protruding, or winging, of the scapula. | Pain management techniques, scapular mobilization. | Post-surgical management if surgical grafting is completed. If the long thoracic nerve is permanently damaged, scapulothoracic fusion surgery may be completed, in which the scapula is fused to the thorax for stability. A sling may be used post surgery to immobilize the shoulder. |
 |
|
| Median Nerve Injury – trauma to the median nerve. | Causes ape hand deformity. Symptoms: ape hand deformity, sensory loss in index, middle, and radial side of ringer finger; loss of pinch, thumb opposition, index finger MCP and PIP flexion; and decreased pronation. | Static thenar web spacer splint. | AROM and PROM in splint for digits and thumb, tendon gliding exercises, scar massage, discontinue splint at 6 weeks and begin strengthening exercises. Dorsal wrist blocking splint with wrist in 30 degrees of flexion worn for 4-6 weeks. |  |
|
| Median nerve laceration – the median nerve is partially or completely severed. | Results in loss of thumb opposition, weak pinch. Clawing of index/mid fingers occurs in low level lesions. Ape hand deformity – flattening of thenar eminence. | A/PROM, scar management, strengthening, sensory re-education. Dorsal protection splint (30° wrist flexion if low lesion, 90° elbow flexion at elbow if high), C-Bar splint to prevent thumb adduction contracture |
Edema control, scar management, nerve gliding exercises, AROM, sensory re-education including treatment for tactile sensitivity, strengthening per post-op protocol. | Hypertrophic scarring may lead to compression of the median nerve and additional damage. |  |
| Median and Ulnar nerve injury – Injury to both the median and ulnar nerves results in an impairment of function. Can be caused by car accidents and glass injuries. |
Loss of sensation to the volar surface of all digits, loss or impairment of finger flexion, thumb opposition. Clawing of all digits. | A/PROM, scar management, strengthening, sensory re-education. Figure of eight splint to prevent MP hyperextension or dynamic MCP flexion splint |
Edema control, scar management, nerve gliding exercises, AROM, sensory re-education including treatment for tactile sensitivity, strengthening per post-op protocol. |  |
|
| Radial Nerve laceration – the radial nerve is partially or completely severed. | Results in the inability of the digits to release objects; difficulty manipulating objects.</t d> | ROM, sensory re-education, home program, activity modification, dynamic extensor splint. | Edema control, scar management, nerve gliding exercises, AROM, sensory re-education including treatment for tactile sensitivity, strengthening per post-op protocol. Dynamic extension splint. | Hypertrophic scarring may lead to compression of the radial nerve and additional damage. |  |
| Ulnar Nerve Injury – trauma to the ulnar nerve. | Results in ulnar claw deformity and numbness of the ulnar side of the hand and the fifth and half of the fourth digits, with generalized weakness of the ulnar side of the hand and pain. Trouble cutting with small knife. Trouble with power grip and lateral pinch. | A sling is used for type 1 fractures or comfort if the client has pain and is nervous in public places. Ulnar nerve injury splint, dynamic/static splint to position MP’s in flexion. MCP dorsal blocking splint. If it is a low-level ulnar nerve injury, then a splint that prevents hyperextension of the MCP joints and allows MCP flexion. |
Orthotics are used for immobilization as needed. Dorsal protection splint with wrist in 30 degrees of flexion. ROM is begun early, within 1 week if medically cleared. Edema control, scar management, sensory re-education, nerve gliding exercises, strengthening per post op protocol. |  |
Tendonitis/Tenosynovitis – Tendonitis occurs when the tendon becomes inflamed due to repetitive use of a muscle. Tenosynovitis occurs when the tendon and its sheath become inflamed.
| Condition and Cause | Symptoms | OT Treatments for Conservative Management | OT Treatments for Post-Surgical Management | Contraindications | Photo |
| De Quervain’s Tenosynovitis – inflammation of the thumb muscle/tendon unit. Caused by cumulative microtrauma, repetitive motion. | Pain, swelling, limited motion in the abductor pollicis longus and extensor pollicis brevis, and the tendons in the first dorsal compartment of the wrist. | Ergonomic adaptations to work station, patient education, strengthening exercises. Wrist thumb spica splint. Forearm based thumb spica splint with wrist in neutral and thumb radially abducted for 3 weeks. After 3 weeks, the client can progress to a soft splint and isometric exercises. | Gentle ROM, tendon gliding exercises, isometric strengthening exercises, grip and pinch strengthening after 2 weeks, scar management and desensitization techniques, splint with wrist in 20 degrees extension. | Nonoperative treatment: activity modification to avoid pinching during activities. |  |
| Lateral epicondylitis – inflammation of the tendons of the wrist extensors at the insertion points on and around the lateral epicondyle. Caused by repetitive motion. Also called tennis elbow. | Pain, inflammation, limited movement of the wrist extensors, especially extensor carpi radialis brevis. | Ice/deep friction massage, stretching, activity modification, strengthening. Lateral epicondylitis brace, also called a tennis elbow brace. The splint rests the muscle and tendon and protects against pain with activity. | Edema control, modalities for circulation, active and passive range of motion, activity modification, gentle strengthening per post op protocol. | Control of edema and gradual increases in movement post surgery needed to prevent re-injury to affected area. |  |
| Medial epicondylitis – inflammation of the tendons of the wrist flexors at the insertion points around the medial epicondyle. Caused by repetitive motion. Also called golfer’s elbow. | Pain, inflammation, limited movement of the wrist flexors. | Ice/deep friction massage, stretching, activity modification, strengthening. Medial epicondylitis brace, also called a golfer’s elbow brace. The splint rests the muscle and tendon and protects against pain with activity. | Elbow immobilizer 1-3 weeks post surgery, edema control, modalities for circulation, gentle ROM once immobilizer is removed. Strengthening of flexor and pronator muscles 6 weeks post op. | Activity modification are necessary to avoid re-injuring the area due to the same types of activity. | |
| Rotator cuff tendonitis – inflammation of the tendons of the shoulder that attach to the muscles that make up the rotator cuff. Caused by repetitive motion, chronic joint inflammation. | Pain, swelling, limited movement of the tendons of the shoulder. | Activity modification, educate in sleeping posture (avoid arm overhead), pain management, Codman exercises/pendulum exercises, strengthening. Shoulder support sling or neoprene shoulder support cuff. |
Shoulder immobilizer, Codman’s exercises (pendulum exercises) for two weeks post op, then passive or active-assistive range of motion. AROM and strengthening can begin 6 weeks post op. | No AROM for 6 weeks post surgery due to risk of injuring the affected areas. | 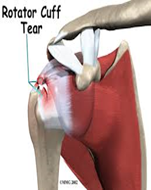 |
| Trigger finger – tenosynovitis of the finger flexors. Caused by cumulative trauma. | Most commonly occurs in the A1 pulley. Trigger finger is a condition in which edema in the tendon and synovium of the digit results in lack of smooth flexion or extension of the finger. | To rest the tendon and prevent snapping as the tendon pulls through the finger pulleys, the MCP joint is blocked by splinting, then gentle pull through with bending and straightening of the distal and proximal interphalangeal joints is recommended 20 times every 2 hours while the client is awake. edema control, tendon gliding, activity/work modification. Hand based TF splint (MCP ⁄DIP and PIP is free), a splint to support the metacarpophalangeal joint in extension |
Edema control, tendon gliding exercises, AROM, activity modification. Blocking splints to protect the released tendon while it is healing. | No active strengthening of the flexor tendons, no forceful grip while recovering from tendon release surgery. | 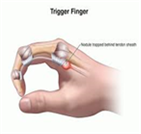
|
| Wrist tendonitis – inflammation of the tendons of the wrist. | Pain, inflammation, limited movement in the wrist. | Dexamethasone is the most widely used medication by therapists using iontophoresis because of its anti-inflammatory properties. AROM, therapeutic activities, joint protection and work simplification. Wrist forearm support splint. |
Edema control, tendon gliding exercises, gentle AROM, strengthening 6 weeks post op. | No forceful grip, no using affected hand to carry heavy objects for 6 weeks post surgery due to risk of injuring tendons. |  |
Tendon laceration and rupture – These injuries result from trauma. A tendon laceration occurs when the tendon is severed by a sharp object. A ruptured tendon is caused by other types of trauma.
| Condition and Cause | Symptoms | OT Treatments for Conservative Management | OT Treatments for Post-Surgical Management | Contraindications | Photo |
| Avulsion Injuries, also called Avulsion fracture | A small piece of bone that is attached to a tendon breaks away from the main bone. Mallet finger is an example of an avulsion fracture. | Icing the affected area, controlled range of motion and gradual strengthening exercises. Splinting may be required. | Scar management at surgical site if graft is completed. Tendon gliding exercises, functional activity as patient will tolerate. Begin strengthening when surgical site is healed or per physician’s protocol. |  |
|
| Extensor Tendon Injury | Injury to the extensor digitorum communis or extensor indicis proprius (EIP). | NA | Tendon gliding exercises promote tendon excursions and prevent adhesions. Modalities include heat, to gradually prepare the tissue for ROM., and NMES to promote tendon excursion and activation. Use of modalities begins once cleared by the prescribing physician. A clearly identified and planned home program is important to ensure the client’s safety and progress toward goals. Strengthening usually not initiated until the late phase of repair, usually 8-12 weeks after surgery. | Strengthening must not be initiated until cleared by the surgeon completing the tendon repair. Overuse of the tendon too early after surgery can result in rupture of the tendon. |  |
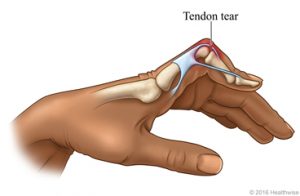
| Flexor tendon injury | A deep cut on the palm side of the fingers, hand, wrist, or forearm can damage the flexor tendons. A flexor tendon injury can make it impossible to bend the fingers or thumb. | NA | Flexor tendon protocol using controlled passive motion. Passive extension of the distal interphalangeal joint if the metacarpal and proximal phalangeal joints are flexed. The distal interphalangeal joint and proximal interphalangeal joint can be passively extended if the other joints of the digit are flexed to initiate tendon glide and prevent scarring of the tendon. Zone II of the flexor tendon system has been called no man’s land because excessive scarring makes it difficult to get good results from a repair. Zone IV consists of the transverse carpal ligament, and the median nerve runs under this ligament; Zone V is distal to this ligament and thus contains the median nerve branch. | Strengthening must not be initiated until cleared by the surgeon completing the tendon repair. Overuse of the tendon too early after surgery can result in rupture of the tendon. | 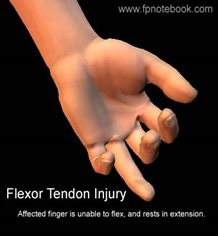 |
| Mallet Finger | Avulsion of the terminal tendon. | Splint the client’s DIP joint in full extension continuously for 6 weeks. The DIP terminal tendon is delicate and requires continuous splinting to prevent extensor lag of the tendon. Old injuries may be splinted continuously for up to 6 months. | Be careful not to hyperextend the DIP joint when splinting or skin breakdown can occur over the dorsal surface of the digit. |  |
Muscle Overuse – These injuries result when microtears and scarring form in the muscles due to overuse.
| Condition and Cause | Symptoms | OT Treatments for Conservative Management | OT Treatments for Post-Surgical Management | Contraindications | Photo |
| Cumulative Trauma Disorder | Trauma to soft tissue caused by repeated force. Patient has muscle fatigue, pain, chronic inflammation, sensory impairment, decreased ability to work. Example: playing piano 10 hours a day. | Acute phase: reduction of inflammation and pain through static splinting, ice, contrast baths, ultrasound, inferential stimulation. Subacute phase: slow stretching, myofascial release, progressive resistive exercises as tolerated, proper body mechanics, education on identifying triggers and returning to acute phase treatment. Return to work, functional capacity evaluation, work hardening. | Dependent on the location and severity of the condition. | Activity modification and proper body mechanics are essential for long-term control of an inflammatory cumulative trauma disorder. |  |
Ligament Injuries – These injuries occur when the ligament attaching one bone to another bone is sprained or ruptured due to trauma.
| Condition and Cause | Symptoms | OT Treatments for Conservative Management | OT Treatments for Post-Surgical Management | Contraindications | Photo |
| MCP flexion limitation | Difficulty flexing the MCP’s due to tightness in the ligaments. The metacarpophalangeal joints (MCP) are of the condyloid kind, formed by the reception of the rounded heads of the metacarpal bones into shallow cavities on the proximal ends of the first phalanges, with the exception of that of the thumb, which is a hinge joint. | Joint mobilization, A/PROM, therapeutic activities. | Edema and scar management, gentle AROM, tendon gliding exercises. Joint mobilization and strengthening when surgical site healed. | Follow surgeon’s protocol for joint mobilization and strengthening after surgery. |  |
| Proximal interphalangeal (PIP) flexion contracture | Shortening and tightening of the tendons and ligaments surrounding the PIP joint due to injury. | Splinting, buddy taping, A/PROM, therapeutic activities. PIP extension splint. A prefabricated dynamic PIP extension assist splint will improve PIP extension and takes less therapy time to fit than to custom make this splint. |
Surgery only done when all conservative management techniques have been tried. Serial casting or external fixation for prolonged stretched are preferred methods of management. |  |
|
| Skier’s Thumb (Gamekeepers Thumb) | Rupture of the ulnar collateral ligament of the MCP joint of the thumb. (i.e., skiing with the thumb held in a ski pole)</s pan> | Wear thumb spica splint at all times. AROM and pinch strength at 6 weeks. ADL’s that require opposition and pinch strength. PROM at 8 weeks and strengthening at 10 weeks. |
Immobilized in thumb spica cast for first 4 weeks, then thumb spica splint for 2 additional weeks. May begin AROM at 6 weeks. Unrestricted use of the hand is allowed at 3 months. | No motion for 4 weeks following surgical repair. Failure rate of conservative management is 50%. |  |
Osteoarthritis and Rheumatoid Arthritis – These conditions result from arthritic conditions. Osteoarthritis is inflammation of the joints that results from “wear and tear”. It is usually caused by repetitive overuse, old sports injuries, or old age. Rheumatoid arthritis is an autoimmune disease that attacks the joints, causing inflammation.
| Condition and Cause | Symptoms | OT Treatments for Conservative Management | OT Treatments for Post-Surgical Management | Contraindications | Photo |
| Arthritis | A form of joint disorder that involves inflammation of one or more joints. Two types: OA and RA. | PROM, AAROM, AROM, edema control, therapeutic activities. Patient education in joint protection, work simplification, energy conservation techniques. Functional splint or safe splints, depending on stage. With a resting splint address the natural aging process of skin and adipose tissue. Use soft straps and thick padding. Specific splints address under specific arthritic conditions. | Strengthening exercises must be graded carefully and gradually to prevent joint damage. Discourage lifting and carrying heavy weights for long distances. |  |
|
| Boutonniere deformity | PIP joint flexed, and the DIP joint hyperextended. | Isolated DIP flexion exercises are performed. Silver rings/ tri tip PIP is splinted in extension. |
 |
||
| CMC arthritis | Most commonly involved arthritic joint in the hand. More common in women, may exist in a localized form or may exists as a systemic form of arthritis, primary form is most common in postmenopausal women, systemic form may be due to RA or gout. | Heat modalities or iontophoresis to relieve pain and improve mobility, AROM, therapeutic activity, joint protection techniques. A hand based thumb spica splint takes pressure off the joint. |
Gradual grading of strengthening exercises to prevent stress and inflammation of the joint. |  |
|
| CMC osteoarthritis | Degenerative joint disease affecting the first carpometacarpal joint (CMC1). This joint is formed by the trapezium bone of the wrist and the first metacarpal bone of the thumb. Occurs when the cushioning cartilage of the joint surfaces wears away, resulting in damage of the joint. | Splinting, heat modalities to relieve pain, joint protection techniques. Wrist/thumb spica splint. May be thermoplastic for more support, neoprene or fabric for less support and more mobility. |
Gradual grading of strengthening exercises to prevent stress and inflammation of the joint. |  |
|
| Rheumatoid arthritis | An autoimmune disease that results in a chronic, systemic inflammatory disorder that may affect many tissues and organs, but principally attacks flexible (synovial) joints. | Edema control in acute phase, gentle AROM exercises, therapeutic activities, education in joint protection and work simplification techniques Volar wrist cock-up in extension up to 30 degrees, based on the person’s comfort level. Ulnar drift splint to align fingers close to neutral. |
 |
||
| Swan neck deformity | Injury to the MCP, PIP, or DIP joints characterized by PIP hyperextension and DIP flexion. | Adaptations for therapeutic activities, education in joint protection and work simplification techniques Silver ring splints/tripoint splint. PIP is splinted in slight flexion, or buttonhole splint |
 |
||
| Ulnar Drift | Hand deformity in which the swelling of the metacarpophalangeal joints (the big knuckles at the base of the fingers) causes the fingers to become displaced, tending towards the little finger. The hand including the fingers move towards the ulna. Ulnar deviation is a disorder in which flexion by ulnar nerve innervated muscles is intact while flexion on the median nerve side is not. | Adaptations, joint protection and work simplification techniques. Ulnar deviation splint |
 |
Bone Fractures – These injuries result in a fracture of a bone due to trauma.
Shoulder Conditions and Other Conditions – These conditions have assorted causes that have not been listed in the previous charts.
| Condition and Cause | Symptoms | OT Treatments for Conservative Management | OT Treatments for Post-Surgical Management | Contraindications | Photo |
| Adhesive capsulitis (frozen shoulder) | Restricted active and passive shoulder range of motion | PROM, modalities, encourage active use, pain management (modalities) Dynamic shoulder splint |
Dynamic shoulder splint, aggressive A/PROM. | Do not immobilize except for a short period after any surgery. Instruct patients not to wear slings or splints unless prescribed by a physician or therapist. |  |
| Burns | A type of injury to flesh or skin caused by heat, electricity, chemicals, friction, or radiation. Burns that affect only the superficial skin are known as superficial or first-degree burns (i.e. sunburn). When damage penetrates into some of the underlying layers, it is a partial-thickness or second-degree burn. In a full-thickness or third-degree burn, the injury extends to all layers of the skin. A fourth-degree burn additionally involves injury to deeper tissues, such as muscle or bone. | Superficial, partial thickness burns: wound care and debridement, sterile whirlpool, dressing changes, gentle A/PROM to individual’s tolerance, edema control, splinting if necessary, ADL’s and role activities. Deep partial thickness burns: wound care and debridement, sterile whirlpool, dressing changes, gentle A/PROM to individual tolerance, edema control, splinting if necessary, ADL’s and role activities, and strengthening (when wounds are healed). Airplane splints. Heal in anatomical position. Resting splints or ball splints may be used for burns to the volar surface of the hands. |
Similar treatments following skin graft surgery. | No scar mobilization until the wound is completely healed. Pay attention to skin integrity around wounds and grafting sites. |
 |
| Burns to the dorsum of the hands | Passively range each digit and joint one at a time. Ranging each joint separately decreases the chance of rupturing finger extensor tendons with dorsal hand burns. The metacarpophalangeal joints to be splinted in 70°–90° of flexion to prevent clawing of the fingers and shortening of the tendons and ligaments. This type of splint is also referred to as an antideformity splint, safe position splint, or intrinsic plus splint. Splinting the hand in the safe position allows the graft to take and the wound to heal and prevents deformities. |
Similar to burns above. | Pay attention to skin integrity around wounds and grafting sites. |  |
|
| Dupuytren’s Contracture | Disease of the fascia of the palm and digits. Results in flexion deformities of the involved digits (i.e., mostly ring finger). Frequently treated with surgical release of the affected fascia. | Wound Care: dressing changes. Whirlpool if infection is suspected. Edema Control: elevation above the heart. A/PROM and progress to strengthening when wound are healed. Scar management, functional tasks that emphasize flexion (griping) and extension (release). Extension splint at all times except to remove for ROM and bathing |
 |
||
| Flaccidity | Lacking firmness, resilience, or muscle tone. No active movement present. | PROM to prevent contracture and preserve skin integrity, positioning. Resting hand splint |
 |
||
| Flaccid wrist | Lacking firmness, resilience, or muscle tone in the wrist. No active movement present. | Support the user’s wrist in 10 to 20 degrees of extension to prevent contracture, but allows digits to function should movement return. Wrist cock-up splint. |
 |
||
| Focal hand dystonia | Involuntary muscle contractions of the hand, causing the fingers to curl into flexion or straighten into extension involuntarily. Abnormal movement of the hand, usually related to specific tasks. Often happens in people who push themselves too hard; musicians, computer programmer. Writer’s cramp is a form of focal hand dystonia. | Adaptations, compensatory strategies, mirror therapy. Tactile and proprioceptive retraining. |  |
||
| Index finger injury | Injury to the index finger, (also referred to as forefinger, pointer finger, trigger finger, digitus secundus, digitus II, and many other terms), is the first finger and the second digit of a human hand. | Edema control, scar management if needed, tendon gliding exercises to prevent scar limitations, AROM, therapeutic activity, strengthening when injury healed. Buddy strap incorporating the index and middle fingers provides passive rom to the index finger. |
 |
||
| Rett syndrome | Under the broad category of pervasive developmental disorders, together with the autism spectrum disorders. Repetitive stereotyped hand movements, such as wringing and/or repeatedly putting hands into the mouth. | Maintain the integrity of the skin such as dynamic elbow splints that inhibit a hand to mouth pattern by limiting full elbow flexion. Lever arch brace, thumb spica splint |
 |
||
| Spasticity | Altered skeletal muscle performance in muscle tone involving hypertonia; it is also referred to as an unusual “tightness”, stiffness, or “pull” of muscles. | A/PROM to reduce contracture, therapeutic activities, home exercise program. Anti-spasticity splint or cone splint |
 |