TRAUMATIC BRAIN INJURY (TBI)

A Traumatic brain injury (TBI) is defined as a nondegenerative, non congenital insult to the brain from an external mechanical force, possibly leading to permanent or temporary impairment of cognitive, physical, and psychosocial functions, with an associated diminished or altered state of consciousness. TBI can result when the head suddenly and violently hits an object or when an object pierces the skull and enters brain tissue. Symptoms of a TBI can be mild, moderate or severe, depending on the extent of damage to the brain. Mild cases may result in a brief change in mental state or consciousness, while severe cases may result in extended periods of unconsciousness, coma or even death.
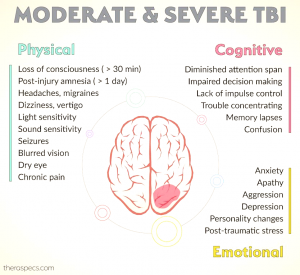
Symptoms
Symptoms vary greatly depending on the severity of the head injury, but may include any of the following:
• Vomiting
• Lethargy
• Headache
• Confusion
• Paralysis
• Coma
• Loss of consciousness
• Dilated pupils
• Vision changes (blurred vision or seeing double, not able to tolerate bright light, loss of eye movement, blindness)
• Cerebrospinal fluid (CSF) (which may be clear or blood-tinged) coming out of the ears or nose
• Dizziness and balance problems
• Breathing problems
• Slow pulse
• Slow breathing rate, with an increase in blood pressure
• Ringing in the ears or changes in hearing
• Cognitive difficulties
• Inappropriate emotional responses
• Speech difficulties (slurred speech, inability to understand and/or articulate words)
• Difficulty swallowing
• Body numbness or tingling
• Droopy eyelid or facial weakness
• Loss of bowel control or bladder control
Classification of TBI
1. Primary and Secondary injuries
Primary injury: Induced by a mechanical force and occurs at the moment of injury- the 2 main mechanisms that cause primary injury are contact (eg, an object striking the head or the brain) and acceleration-deceleration. Primary injuries can manifest as focal injuries (eg, skull fractures, intracranial hematomas, lacerations, contusions, penetrating wounds), or they can be diffuse, as in diffuse axonal injury.
Secondary injury: Not mechanically induced- this type of injury may be delayed from the moment of impact, and it may superimpose an injury on a brain which has already affected by a mechanical injury. Secondary injuries may develop over a period of hours or days following the initial traumatic assault.
2. Focal and diffuse injuries
These injuries are commonly found together; they are defined as follows:
Focal injury: Includes scalp injury, skull fracture, and surface contusions, generally caused by contact
Diffuse injury: Includes diffuse axonal injury (DAI), hypoxic-ischemic damage, meningitis, and vascular injury; usually caused by acceleration-deceleration forces.
Measures of Severity
1. Glasgow Coma Scale (GCS)
A 3 to 15 point scale used to assess a patient’s level of consciousness and neurologic functioning; scoring is based on best motor response, best verbal response, and eye opening (eg, eyes open to pain, open to command).
Glasgow Coma Scale
Eye opening
Spontaneous = 4
To speech = 3
To painful stimulation = 2
No response = 1
Motor response
Follows commands = 6
Makes localizing movements to pain = 5
Makes withdrawal movements to pain = 4
Flexor (decorticate) posturing to pain = 3
Extensor (decerebrate) posturing to pain = 2
No response = 1
Verbal response
Oriented to person, place, and date = 5
Converses but is disoriented = 4
Says inappropriate words = 3
Says incomprehensible sounds = 2
No response = 1
The severity of TBI according to the GCS score (within 48 hours) is as follows:
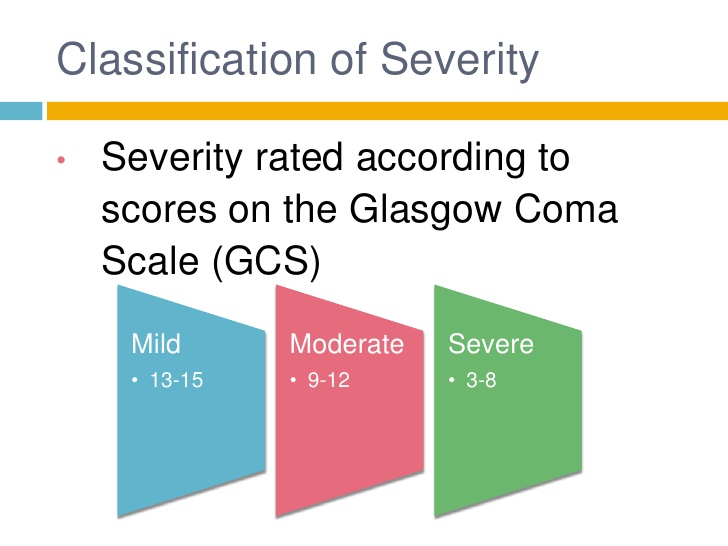
• Severe TBI = 3 – 8
• Moderate TBI = 9 – 12
• Mild TBI = 13 – 15
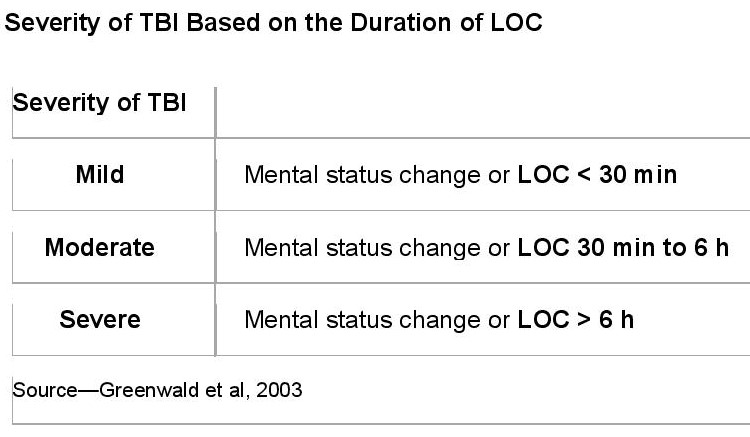
2. Duration of loss of consciousness
• Mild (mental status change or loss of consciousness LOC < 30 min)
• Moderate (mental status change or LOC 30 min to 6 hours)
• Severe (mental status change or LOC >6 hours)
3. Ranchos Los Amigos Scale of Cognitive Functioning
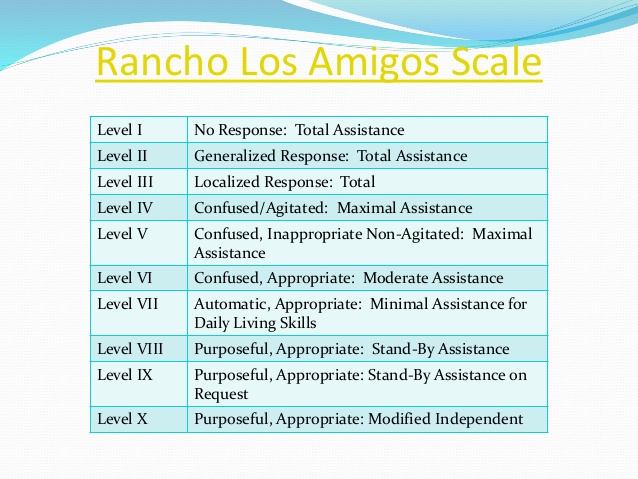 The severity of deficit in cognitive functioning can be defined by the Ranchos Los Amigos Scale.
The severity of deficit in cognitive functioning can be defined by the Ranchos Los Amigos Scale.
Level I = No response
Level II = Generalized response
Level III = Localized response
Level IV = Confused-agitated
Level V = Confused-inappropriate
Level VI = Confused-appropriate
Level VII = Automatic-appropriate
Level VIII = Purposeful-appropriate
4. Posttraumatic amnesia (PTA)

The time elapsed from injury to the moment when patients can demonstrate continuous memory of what is happening around them.
Outcome Measures– Commonly used to measure outcome after TBI:
• Functional Independence Measure (FIM): An 18-item scale used to assess the patient’s level of independence in mobility, self-care, and cognition
• Glasgow Outcome Scale (GOS)
The GOS categorizes the outcomes of patients after traumatic brain injury, as follows:
I. Death
II. Persistent vegetative state: Minimal responsiveness
III. Severe disability: Conscious but disabled; dependent on others for daily support
IV. Moderate disability: Disabled but independent; can work in sheltered setting
V. Good recovery: Resumption of normal life despite minor deficits
• Disability Rating Scale (DRS) : Measures general functional changes over the course of recovery after TBI
Complications
Complications include the following:
• Post-traumatic seizures: Frequently occur after moderate or severe TBI
• Hydrocephalus
• Deep vein thrombosis
• Heterotopic ossification
• Spasticity
• Gastrointestinal and genitourinary complications: Among the most common sequelae in patients with TBI
• Gait abnormalities
• Agitation: Common after TBI
• Chronic traumatic encephalopathy (CTE)
Long-term physical, cognitive, and behavioral impairments are the factors that most commonly limit a patient’s reintegration into the community and their return to employment.
They include:
• Insomnia
• Cognitive decline
• Post-traumatic headache: Tension-type headaches are the most common form, but exacerbations of migraine-like headaches are also frequent
• Posttraumatic depression: Depression after TBI is further associated with cognitive decline, anxiety disorders, substance abuse, dysregulation of emotional expression, and aggressive outbursts
OT Intervention
Assessment Tools
There are several assessments that are recommended for the occupational therapist to use during the evaluation phase. They are recommended to assess somatic, cognitive, and emotional/behavioral symptoms that the patient may have, the patient’s occupational performance and their self-perception of their performance.
Examples:
• Behavioral Assessment of Dysexecutive Syndrome
Purpose: This assessment is used to assess executive functioning skills.
• Behavior Rating Inventory of Executive Function for Adults (BRIEF-A)
Purpose: This assessment is used to help determine a patient’s executive functioning and self-regulation abilities. It assesses the patient’s ability to plan, problem solve, and use their memory to engage in their routine occupations.
• Occupational Self-Assessment (OSA)
Purpose: This assessment is used to help identify the patient’s self-perception of occupational competence, importance of occupational functioning, and environmental adaptation. The OSA connects with the Person-Environment-Occupation Model of Occupational Performance to better understand the person and their subjective views of their ability to perform their occupations as well as the environment in which they are performed.
• Canadian Measure of Occupational Performance
Purpose: This assessment may be used to measure outcomes and allows the patient to identify in which occupational areas they are experiencing difficulty. It provides patient-centered care.
Therapeutic Intervention
Typically, in early stages of recovery remediation approaches are used, with a shift toward compensation approaches during later stages of recovery. Greater improvement occurs within the first 5 months of recovery when compared to the subsequent 7 months (Christensen et al., 2008). However, significant gains in motor and visual spatial areas can happen beyond the initial window.
| Deficits | Example of intervention | |
| Arousal and Alertness | A TBI can cause problems with consciousness, awareness, alertness, and responsiveness. Generally, there are four abnormal states that can result from a severe TBI: I. Minimally conscious state — People with severely altered consciousness who still display some evidence of self-awareness or awareness of one’s environment (such as following simple commands, yes/no responses). II. Vegetative state- A result of widespread damage to the brain, people in a vegetative state are unconscious and unaware of their surroundings. However, they can have periods of unresponsive alertness and may groan, move, or show reflex responses. If this state lasts longer than a few weeks, it is referred to as a persistent vegetative state. III. Coma- A person in a coma is unconscious, unaware, and unable to respond to external stimuli such as pain or light. A coma generally lasts a few days or weeks after which the person may regain consciousness, die, or move into a vegetative state. IV. Brain death– The lack of measurable brain function and activity after an extended period of time is called brain death. |
Multimodal sensory stimulation to improve arousal and enhance clinical outcomes.
|
| Motor Function | Physical deficit can include ambulation, balance, coordination, fine motor skills, strength, and endurance. | Rehabilitation programs to improve motor function.  |
| Performance of ADLS | Physical and cognitive deficits result in poor ADL performance. | Activity-based interventions focused on client-centered goals and delivered in a relevant environmental context to improve occupational performance.
|
| Self-Awareness | TBI survivors often have deficits in self-awareness and subjective well-being; they are often unaware of their acquired deficits. Impaired self-awareness reduces the motivation to participate in the rehabilitation activities, as they are deemed unnecessary, and this imposes significant challenges for recovery. Improving self-awareness is essential for improving cognition, as patients need to recognize their deficits in order to improve them. | A combination of video and verbal feedback can improve self-awareness in patients without increasing emotional distress.
|
| Learning and Memory | Individuals with TBI have difficulty with learning and memory due to encoding deficits. | Use established memory encoding strategies, like self-generation and testing, to enhance encoding and retention of information. • Self-generation is an encoding technique that asks individuals to create their own examples to better understand new material. • Spacing out information is a technique where small amounts of new information are presented in multiple short time periods. • Testing is a remediation approach used for learning and memory • Visual imagery is a useful tool for improving prospective memory * Prospective memory- the ability to remember to perform activities in the future).   |
| Executive Function | Executive functioning (EF) is the ability to plan, organize, strategize, and focus attention. | The cognitive orientation to occupational performance model (CO-OP) encourages individuals who have sustained a TBI to use metacognitive strategies to identify and strengthen weak areas of cognition. Metacognition refers to the ability to recognize one’s cognitive capacity. If a patient recognized, for example, that he had trouble remembering verbally presented information, he could use a metacognitive strategy of requesting written information.
|
| Attention | Attentional deficits are common after TBI and manifest in selective, sustained, and divided attention. | Attention Process Training (APT) is shown to improve selective attention in individuals with TBI by progressively increasing attentional demands.
|
References:
https://emedicine.medscape.com/article/326510-overview
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6730543/
https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Traumatic-Brain-Injury
https://www.brainline.org/article/occupational-therapy-practice-guidelines-adults-traumatic-brain-injury
https://commons.und.edu/cgi/viewcontent.cgi?article=1125&context=ot-grad
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6730543/