This worksheet discusses the various aspects of swallowing, the definitions and causes of dysphagia, and various occupational therapy treatments for feeding disorders.
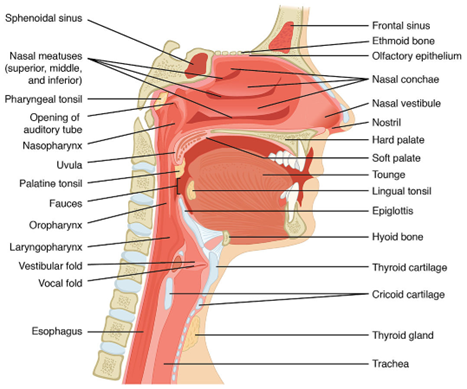
Anatomy of the Mouth and Throat
Oral Structures and their Function in Feeding
 ..
.. 
| Structure | Description | Function During Eating |
| Oral Cavity | Hard and soft palate, tongue, fat pads of cheeks, upper and lower jaw, teeth. | Contains food during chewing and drinking. -performs initial mastication prior to swallowing. |
| Pharynx | Base of tongue, buccinator muscle, oropharynx, tendons, hyoid bone. | Funnels food into the esophagus. -both food and air share the pharynx. |
| Larynx | Epiglottis, false and true vocal cords. | Acts as a valve to the trachea. -closes during swallowing. |
| Trachea | Tube below the larynx, cartilaginous rings. | Allows air into the bronchi and lungs. -closed by the larynx during swallowing. |
| Esophagus | Thin and muscular tube that leads to the stomach. | Carries food from the pharynx, through the diaphragm and into the stomach. |
..
..
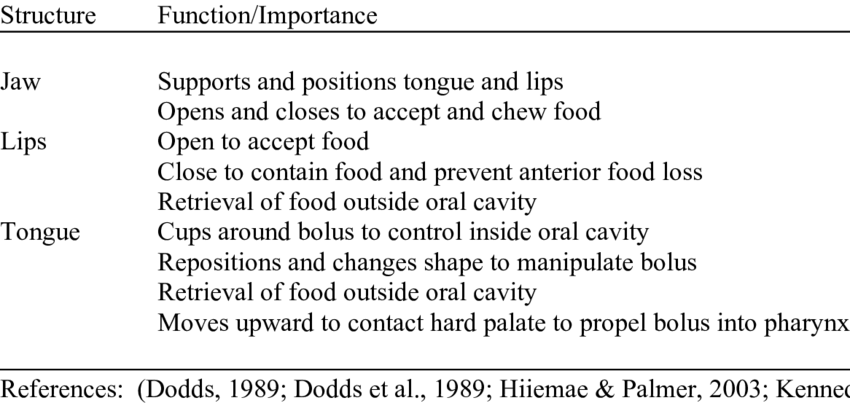
Oral Motor Skills Used During Eating
| Motor Skill | Description | Purpose |
| Sucking | The lips purse and seal around the liquid source, such as a straw. Inward breathing is used to pull liquid into the mouth from the source. The oral cavity and pharynx direct the liquid into the esophagus. | Intake of liquids, especially by infants under the age of 12 months. Also used by adults as an alternative to drinking. |
| Drinking | The lips form a controlled opening. The edge of the cup or glass rests on the lower lip and liquid is slowly poured into the oral cavity. The lips close and the oral cavity and pharynx direct the liquid into the esophagus. | Intake of liquids after the age of 12 months. Becomes the primary method of liquid intake over sucking, although sucking is still used. |
| Biting | The front upper and lower teeth apply force to slice through food and intake it into the oral cavity. | Intake of food in small pieces that fit inside the oral cavity. |
| Chewing | The back upper and lower teeth apply repeated force to break down and soften food. The lower jaw moves in a rotational direction to cause the lower teeth to grind food against the upper teeth. The saliva glands release fluid to assist in softening food. This process is also called mastication. | Initial preparation of food for swallowing and digestion. Chewing is part of the oral preparatory phase of swallowing. |
Phases of Swallowing
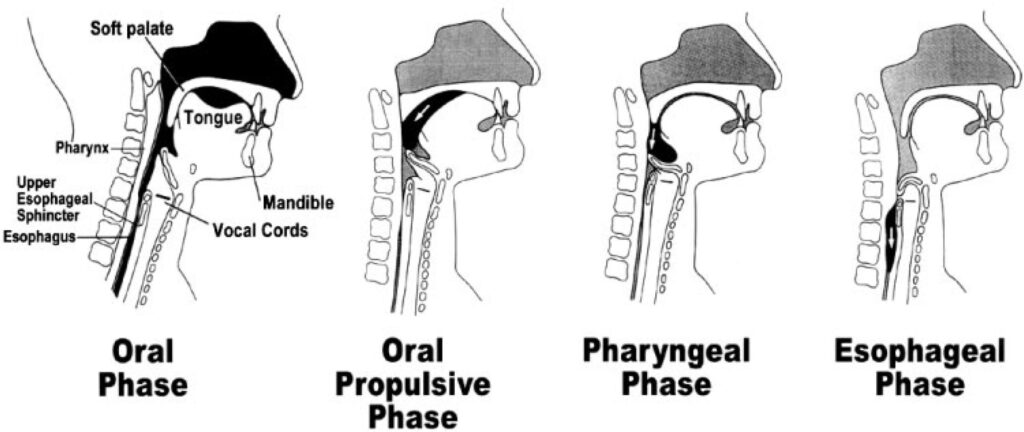
| Phase | Description | Type of Control and Duration |
| Oral Preparatory Phase | Oral manipulation, including chewing described above, to form the food into a soft mass called a bolus. | Voluntary, amount of time varies depending on the consistency of the food. |
| Oral Phase | The tongue elevates against the alveolar ridge and moves the bolus to the back of mouth, ending with the beginning of the pharyngeal swallow. | Voluntary, lasts 1-3 seconds. |
| Pharyngeal Phase | The bolus reaches the anterior faucial arches, which triggers the swallow. Hyoid and larynx move upward and forward, epiglottis retroflexes to protect the airway. Ends with opening/relaxation of cricopharyngeal sphincter | Involuntary, lasts 1-3 seconds. |
| Esophageal Phase | Contraction of the cricopharyngeus muscle that pushes the bolus toward the stomach, ends with relaxation of the lower esophageal sphincter to allow food into the stomach. | Involuntary, lasts 8-10 seconds. |
.Dysphagia
Definition of dysphagia – difficulty or discomfort in swallowing that persists over a prolonged period of time.
Types of Dysphagia
| Type | Symptoms | Causes |
| Esophageal – the sensation that food is sticking in the base of the throat after swallowing has begun. | -pain when swallowing -the sensation of food sticking in the throat -regurgitation -frequent heartburn -back-up of food or stomach acid into the mouth or throat -hoarseness -sudden weight loss |
-muscle spasms or strictures in the esophagus (Achalasia) -esophageal tumors -Gastroesophageal Reflux Disease (GERD) -esophagitis -scleroderma -radiation treatment for cancer |
| Oropharyngeal– the muscles of the mouth and throat are weakened, leading to ineffective movement of food and liquid from the mouth to the esophagus and stomach. | -coughing or gagging when swallowing -drooling -sudden weight loss -inability to swallow -requiring food to be cut up in small pieces or avoiding certain foods |
-neurological diseases or damage -pharyngoesophageal diverticulum (Zenker’s), a small pouch just above the esophagus that collects food particles -cancer and cancer treatment |
Diagnosis & Treatment for Dysphagia
The SLP may request a swallow study for a patient to determine the mechanical cause of choking or aspiration. Treatment for dysphagia is usually directed by a speech and language pathologist (SLP) who specializes in feeding and swallowing disorders.
–Barium swallow study – the patient drinks a barium liquid that coats the GI tract. An x-ray of the GI tract is then performed. The barium helps to distinguish the GI tract from other tissues on the x-ray, helping the clinician to identify problem areas.

–Videofluoroscopy – a “moving x-ray” called fluoroscopy is used to observe food and liquid as it travels down the GI tract.

Occupational therapy support- carry over of specialized feeding and swallowing techniques recommended by the speech and language pathologist during daily activities, based on the results of swallow studies and other evaluation techniques. Knowledge of treatment techniques and adaptations is crucial to implement dysphagia treatment correctly.
The following charts will address the various aspects of treatment for dysphagia patients.
Frameworks for Dysphagia Management
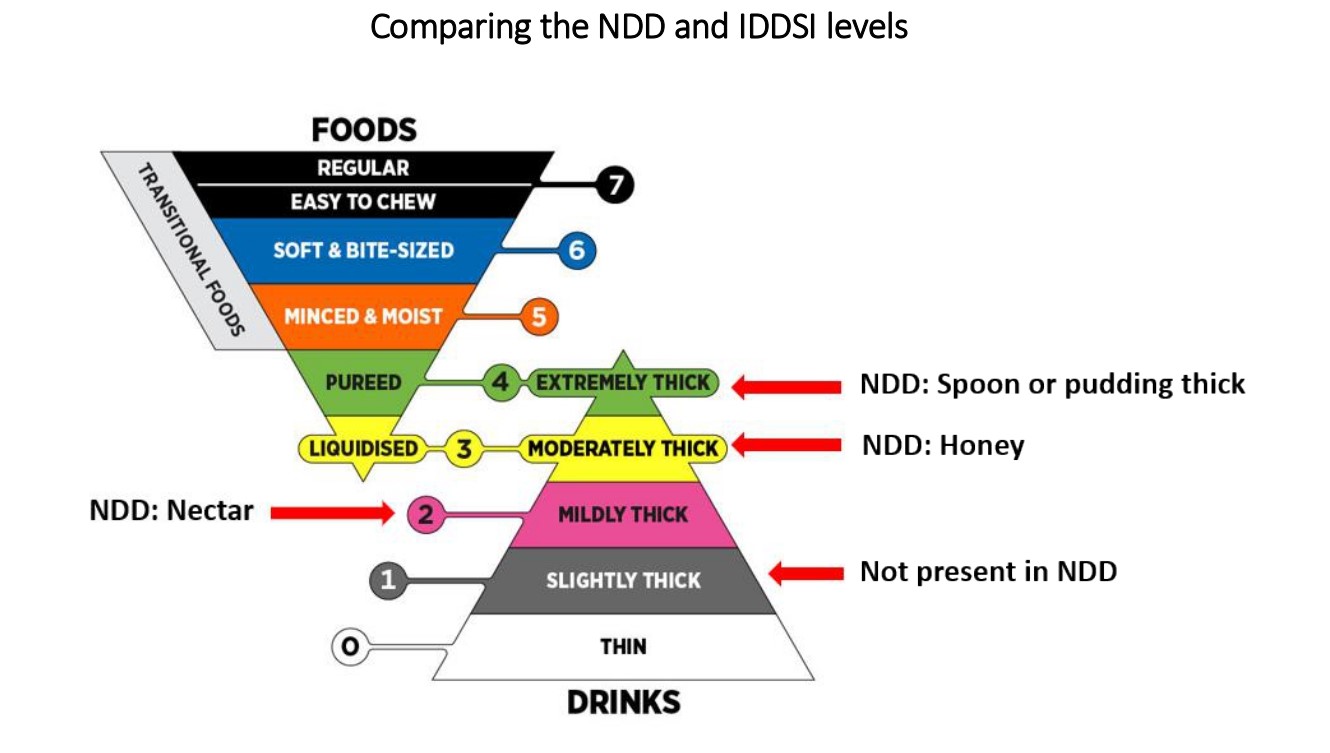
1. The National Dysphagia Diet (NDD) of 2002 (For Your Information)
2. The International Dysphagia Diet Standardization Initiative (IDDSI) Framework which replaced the National Dysphagia Diet
1. National Dysphagia Diet (NDD)
NDD Level 1 (Pureed): These are foods that are pureed or smooth, like pudding. They need no chewing. This includes foods such as yogurt, mashed potatoes with gravy to moisten it, smooth soups, and pureed vegetables and meats.
NDD Level 2 (Mechanical soft): These are moist foods that need some chewing. They include soft, cooked, or mashed fruits or vegetables, soft or ground meats moist with gravy, cottage cheese, peanut butter, and soft scrambled eggs. You should avoid crackers, nuts, and other dry foods.
NDD Level 3 (Soft): This includes soft-solid foods that need more chewing. This includes meat, fruit, and vegetables that are easy to cut or mash. You should avoid crunchy, sticky, or very dry foods. This includes nuts, crackers, chips, and other snack foods.
Regular: This level includes all foods.
2. International Dysphagia Diet (IDDS)
The International Dysphagia Diet is an updated framework to consider foods and liquids with standardized terms. Created to provide clarity and continuity for people with dysphagia on an international scale.
• Created in 2013
• Published in 2015
• Clinical application began in 2018
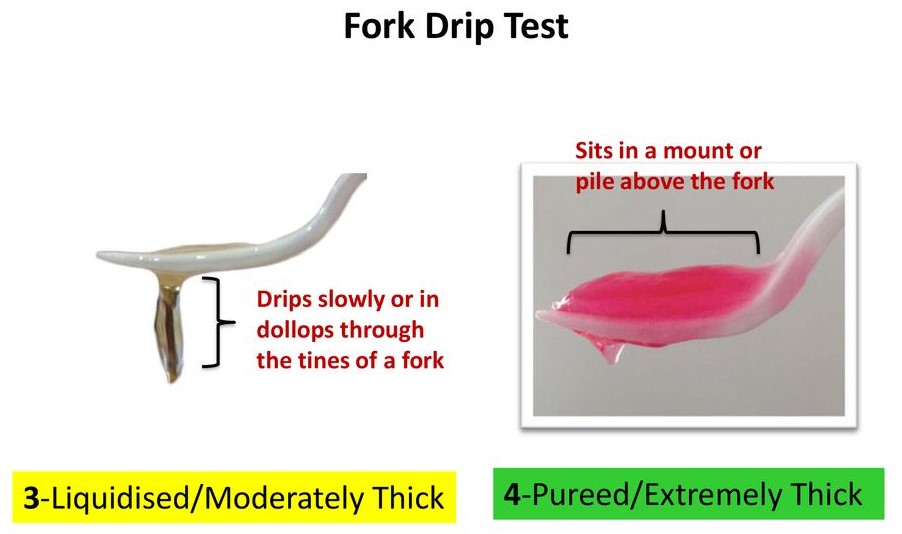
This dysphagia diet framework consists of eight levels (0-7) and includes both foods and liquids on a single continuum. Drinks/liquids are measured from Levels 0-4, while foods are measured from Levels 3-7.
Liquid Consistencies
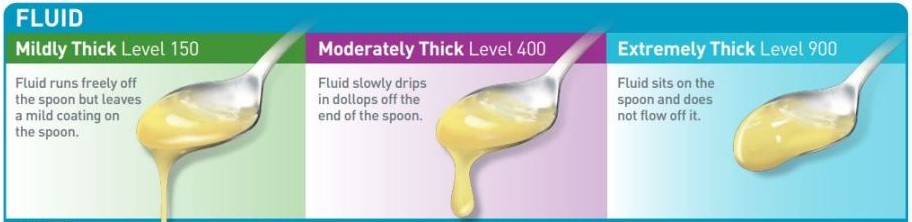
Dysphagia patients may experience difficulty swallowing liquids, requiring that the liquids be thickened. A thickening substance is used to thicken normal liquids to the prescribed consistency. The chart below reviews the four consistency levels.
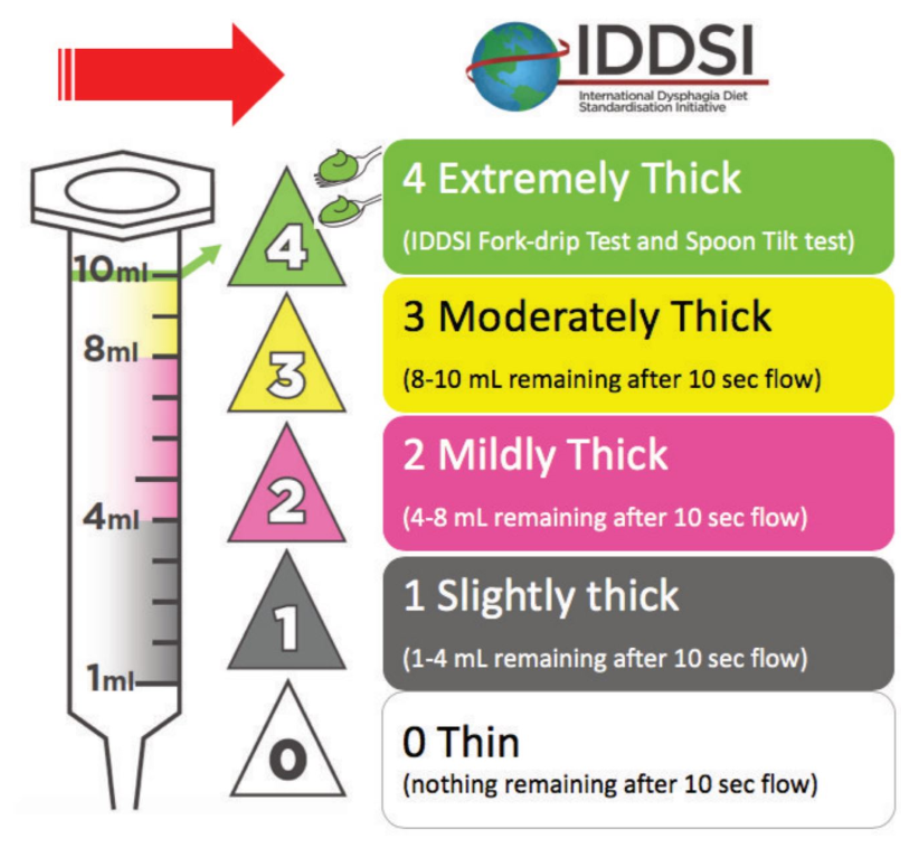
| Consistency | Description | Examples | Photo |
| Thin | Levels 0-1- Thin-Slightly thick
Liquid flows freely; normal liquid consistency. |
Water, milk, juice, broth, foods that melt such as popsicles. |  |
| Nectar | Level 2- Mildly thick
Liquid is slightly thickened, slowing the flow |
Tomato juice, fruit nectar, smoothies.
|
 |
| Honey | Level 3- Moderately thick, Liquidized
Liquid is thickened until it drips or flows slowly off of a spoon. |
Honey, syrup |  |
| Pudding | Level 4- Extremely thick, Pureed
Liquid is thickened to the consistency of pudding so that it does not drip or flow off of a spoon. |
Pudding, ice cream | 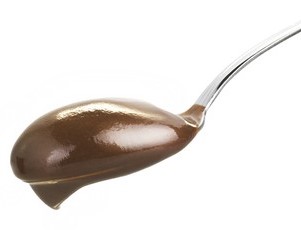 |
.
HOW TO THICKEN LIQUIDS
Food Consistencies
As with liquids, patients with dysphagia may require the consistency of food to be adjusted to increase ease of swallowing. This chart reviews the four levels of food consistencies.

| Consistency | Description | Examples | Photo or Video |
| Level 4 – Pureed | Food is blended to a pudding-like consistency. Liquid is added to dry foods to achieve this consistency. | Mashed potatoes, mashed squash, applesauce. | |
| Level 5 – Mechanical Soft | Soft, cohesive foods are allowed unaltered. Chunkier foods or harder foods are cooked and fork-mashed, ground or softened. Breads are usually not allowed. | Ground meat, mashed vegetables | |
| Level 6 – Soft | Soft solid foods are allowed. Meat must be cooked well and cut into small pieces. Fruits and vegetables should be peeled and/or cooked. Soft breads are allowed. | Diced beef or chicken, canned meat such as tuna, canned vegetables, soft fruits like bananas, strawberries. | |
| Level 7 – Regular | Normal diet. Food does not need to be altered.
|
Normal foods. |  |
.. 
** Level 3 includes moderately thick liquids and liquidized foods, which share similar characteristics and descriptions.
** Level 4 includes extremely thick liquids and pureed foods, which share similar characteristics and descriptions.
** Level 5 contains minced particle sizes of 4mm, which happens to be the size of food particles after chewing and are “swallow-ready” so this diet requires minimal chewing.
* For pediatrics, 2 mm particle size is recommended.
** Level 6 contains bite sizes that are 1.5cm or 15mm, so that if a chunk falls into the airway, the person will not choke/asphyxiate. The size of 15mm is about the size of an adult thumbnail, and is smaller than the typical adult airway.
* For pediatrics, the chunk size should be no larger than 8mm or the size of the child’s fingernail on their little finger.
Summary of Dysphagia Diet
Dysphagia diet 1: Thin liquids (eg, fruit juice, coffee, tea)
Dysphagia diet 2: Nectar-thick liquids (eg, cream soup, tomato juice)
Dysphagia diet 3: Honey-thick liquids (ie, liquids that are thickened to a honey consistency)
Dysphagia diet 4: Pudding-thick liquids/foods (eg, mashed bananas, cooked cereals, purees)
Dysphagia diet 5: Mechanical soft foods (eg, meat loaf, baked beans, casseroles)
Dysphagia diet 6: Chewy foods (eg, pizza, cheese, bagels)
Dysphagia diet 7: Foods that fall apart (eg, bread, rice, muffins) and then finally, mixed textures
Difficulties with Oral Motor Control
Oral motor control is related to dysphagia in that the ability to control and funnel food to the throat can directly affect swallowing. This chart will review problems with oral motor control that could interfere with food intake.
| Oral Motor Problem | Description | Effect on Swallowing | Photo |
| Poor lip closure | The lips do not close tightly after food or liquid enters the mouth. | Food and liquid escape through the lips, causing drooling and loss of food during chewing and swallowing. |  |
| Poor lateralization of tongue movements. | The tongue does not effectively move from side to side in the mouth. | Poor formation of the bolus prior to swallowing, pocketing of food in the cheeks due to the inability of the tongue to clear food. | 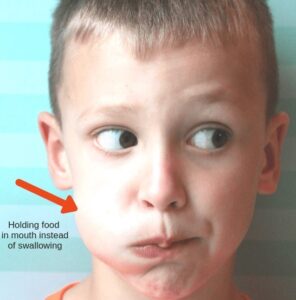 |
| Tongue thrust | During swallowing, the tongue thrusts out of the mouth, rather than up and back. | Food is pushed out of the mouth instead of up and back toward the throat. |  |
| Poor lateral movement of the jaw | The lower jaw moves up and down but displays minimal side to side movement during chewing. | Ineffective formation of the bolus, food particles may be too large to swallow. | 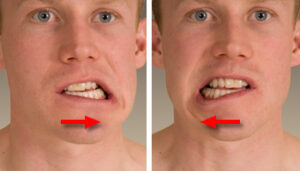 |
| Misaligned or weak bite | The teeth are unable to align correctly to bite food, or the jaws are too weak to exert pressure on the teeth to bite. | Inability to take small pieces of food into the mouth. |  |
Other Factors that Affect Swallowing
| Factor | Description | Effect on Swallowing | Video |
| Postural Control/Positioning | The patient may have poor head, neck or upper body control, resulting in the head flopping forward, sideways, or backward. The patient may be in a slouched or reclined position during feeding. | Food may fall out of the mouth. Drooling may occur during feeding. The patient may choke on food that slides to the back of the throat too quickly. | |
| Upper Extremity Control | The patient may have difficulty holding utensils to bring food to the mouth. He or she may be too weak to use a knife to cut food or may be unable to coordinate hands and head to effectively bring food and drink to the mouth. | Difficulty or inability to place food and drink into the mouth. Spilling of food and drink. Inadequate nutrition. | |
| Cognitive Abilities | The patient may not be aware of the presence of food in the mouth. He or she may not know how to prepare food to place it in the mouth. | Pocketing of food in the cheeks. Bites that are too large or too small. Refusing to eat or forgetting that food is present. |
Occupational Therapy Treatment for Dysphagia and Feeding Problems
General principles when working on feeding skills:
1. Make sure to be aware of any dietary restrictions and prescribed food consistencies.
2. Make sure that food is at a safe temperature – not too hot and not too cold.
3. Have the patient eat in an environment that is appropriate for eating, i.e. the dining room or on the bedside table, not in the bathroom or hallway.
4. Make sure the patient is alert and aware that he or she is about to eat. It is helpful if the patient is hungry.
| Problem | Intervention | Example | Photo or Video | |
| Poor postural control | Position the patient sitting upright with head and spine aligned in neutral, hips and knees at a 90 degree angle, and feet on the floor. -use head, lateral and pelvic supports if the patient is unable to maintain this position independently. -if the patient cannot get out of bed, position the patient in bed as close to the upright neutral position as possible. |
An occupational therapist helps a woman with a diagnosis of Alzheimer’s disease to sit upright prior to eating by placing lateral supports on the sides of her wheelchair. | ||
| Poor upper extremity control | -facilitate hand to mouth movement patterns during neuromuscular treatment. -provide adaptive eating utensils and dishes to compensate for weakness, tremor, athetosis, or other upper extremity problems. |
A man with a diagnosis of Parkinson’s Disease uses a weighted fork to help control his tremor as he loads food from his plate. | ||
| Poor lip closure | Manual stimulation including: -light touch to the midline of the lips -firm maintained pressure around the lips. -stretch pressure around the lips. Sucking and blowing activities: -blow bubbles through a straw -suck on a popsicle -blow up a balloon |
An occupational therapist applies firm pressure around the lips of a 6 year old girl with a diagnosis of cerebral palsy after feeding her a bite of food to facilitate lip closure. | ||
| Poor tongue mobility, tongue thrust | -tongue “exercises” including up/down and side to side movement, repetitive tongue tip sounds, holding the tongue behind the upper teeth. -licking flavor off the lips, i.e. rub a lollipop on the lips and have the patient lick the flavor off. -facilitating tongue retraction during feeding by pressing the bowl of the feeding spoon on the middle of the tongue before withdrawing it from the mouth. |
During feeding with a toddler with a diagnosis of Down syndrome, an occupational therapist presents food on a plastic spoon with a small bowl, then pushes down on the middle of the tongue before withdrawing the spoon from the toddler’s mouth. |
|
|
| Weak or misaligned bite | -use chew tubes for oral motor exercise -bite and hold objects in the teeth (make sure objects are safe to bite) -use handling techniques to align the jaw and facilitate lower jaw mobility during feeding. |
While feeding a patient with advanced Huntington’s chorea, an occupational therapist faces the patient and places her thumb and middle finger along the patient’s jaw line and her index finger along the patient’s cheek to allow her to facilitate lower jaw position and movement. | ||
| Oral sensory problems | -use a z-vibe or other small vibrator to provide vibratory input to the mouth, lips, and facial areas -aromatherapy -deep pressure and proprioceptive activities to all joints -present new food items one at a time in a fun, non-threatening manner. -match food textures and temperatures to the patient’s oral motor abilities. |
An occupational therapist provides brushing, joint compressions, and proprioceptive play activities to a 4 year old child with a diagnosis of autism prior to snack time in his classroom. | ||
| Impaired cognitive abilities | -use sectioned dishes to separate foods of different textures. -use high contrast place settings, i.e. white plate on blue placemat. Make sure food colors contrast with plate. -provide smaller size utensils to control amount of food that enters the mouth. |
An occupational therapist provides a patient with Alzheimer’s disease with a white sectioned place, a dark blue placement, and red utensils to increase contrast while the patient feeds herself. |  |
Examples of Interventions
Recommended Reading
Self-Feeding With the Adult Population: Back to Basics
References
Case-Smith, J. (2005). Occupational Therapy for Children, 5th ed. St. Louis, MO; Elsevier Mosby.
Dysphagia. (2018, February 03). Retrieved February 4, 2019, from https://www.mayoclinic.org/diseases-conditions/dysphagia/symptoms-causes/syc-20372028
Lowsky, D. C., MS, CCC-SLP. (2012, October 16). Easy Oral Motor Exercises to Try – Today! Retrieved February 6, 2019, from https://www.arktherapeutic.com/blog/easy-oral-motor-exercises-to-try-today/
Samelstad, K. M. (1988, May 1). Treatment Techniques to Encourage Lip Closure and Decrease Drooling in Persons with Cerebral Palsy.
Retrieved February 6, 2019, from: https://journals.sagepub.com/doi/abs/10.1177/153944928800800305