SPLINTING STRATEGIES
……………… .. 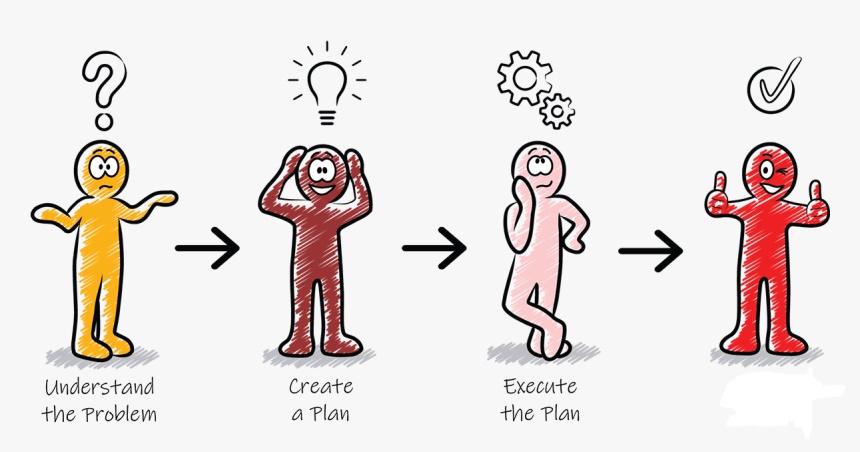
4 basic steps for designing /choosing the right splint for your patient
1. Know your upper limb conditions
2. Work out what the problem is for the patient
3. Work out how you can solve this problem
4. Decide which splint will help you achieve this goal
To help guide you through these steps, consider the following:
Purpose of splint
• Protection
• Positioning for function
• Immobilization for healing
• Restriction of undesired motion
• Correction or prevention of deformity
• Substitution of absent or weak muscles
Immobilization, restriction or mobilization
Immobilization Splints
Immobilization splints are used to protect, to prevent injury, for rest, to reduce inflammation or pain, or for positioning to facilitate proper healing after surgery.
Restriction Splints
Restriction splints limit joint ROM but do not completely stop joint motion. Semiflexible splints are available that limit motion at the extremes of range but allow motion in the middle of the range.
Mobilization Splints
Mobilization splints are designed to increase limited ROM or to restore or enhance function. A mobilizing splint may assist a weak muscle or substitute for motion lost because of nerve injury or muscle dysfunction. The splint may attempt to balance the pull of unopposed spastic muscles to prevent deformity or joint changes and to assist function. A splint may provide resistance against which a weak muscle can exercise to improve its strength or to facilitate tendon gliding after tendon surgery. Frequently, mobilizing splints are used to increase the ROM of contracted joints.
Resting vs Functional
Resting splints—generally used to immobilize the joints and provide a prolonged stretch to tight muscles.
2 types of positioning are achieved by a resting hand splint: a functional (mid-joint) position and an antideformity (intrinsic-plus/safe) position.
i. Functional position
ii. Anti-deformity (POSI) position
i. Functional Position
To rest the wrist and hand joints, the resting hand splint positions the hand in a functional or mid-joint position. This positon provides the best balance of resting length and force production so the hand can function when the patient mobilizes it again. The exact specifications of the functional position of the hand in a resting hand splint and the recommended joint positions vary.
One of the splints most frequently fabricated by OTs is the resting pan (also known as the resting hand or functional position splint), which is used to maintain the hand in a functional position. The purpose of this positioning splint is to keep the soft tissues of the hand in midrange to maintain optimal mobility and to prevent shortening of the soft tissue structures around the joints.
Wrist- 20º to 30º extension
MCP- 45º to 60º flexion
PIP and DIP- 15º to 30º flexion
Thumb- in opposition
ii. Anti-deformity/Safe position (POSI)– also known as the Intrinsic plus position, Edinburgh position and Clam digger position.
The hand can be immobilized in this position for long periods of time without developing as much stiffness as would occur if the digits were positioned differently. Commonly used for burns, trauma and invasive surgery.
Guidelines:
• MCP joints are most protected from contractures in flexion.
• PIP joints, conversely, are most protected in extension & extremely unsafe if immobilized in flexion.
POSI:
MCP flexion 70-90°
PIP in full extension
DIP in full extension
Thumb in wide abduction and opposition
Wrist extension 20-30°
Functional splints- designed to support the joints in more optimal positions for functional hand use. Functional splints are prescribed for use during activities to directly improve task performance, such as a wrist cock-up splint designed to stabilize the wrist during tasks such as handwriting.
Static vs Dynamic
A static splint has no movable components and immobilizes a joint or part of a limb. Static splints are fabricated to rest or protect, to reduce pain, or to prevent muscle shortening or contracture.
Dynamic splints are designed to protect and assist weak musculature to perform tasks, to increase passive motion, to increase active motion by assisting a joint through its range, or to substitute for lost motion. They are characterized by their mobility which is derived from resilient components (elastics, rubber bands, or springs) that produce motion. The objectives of dynamic splints are to encourage the patient to recover their mobility as quickly as possible (e.g. post surgical procedure) and thus prevent the adhesion of soft tissues, and to assist muscle imbalance in order to prevent muscular contractures and to enable the hand to rapidly regain its functional use.
References:
https://www.orfit.com/physical-rehabilitation/information/#guideshttps://musculoskeletalkey.com/hand-immobilization-splints/
http://www.fixhands.com/how-to-refer/splintorthotics/
https://www.ncmedical.com/categories/Hand–Wrist_14464146.html
https://www.rehabmart.com/product/long-opponens-hand-orthosis-32934.html
https://www.slideshare.net/AbeyPRajan1/hand-rehabilitation-following-flexor-tendon-injuries
https://www.slideshare.net/StephanvanBreenenCli/occupational-therapy-and-therapeutic-technologies-interventions
http://otandsplinting.blogspot.com/2010/10/variety-of-splint.html
https://slideplayer.com/slide/246174/
https://www.slideshare.net/AndrewAntonioOTRL/091914-orthotics-project-final