Sensory Integration (SI)

Sensory Integration theory was developed by A. Jean Ayres, PhD, OT during the 1960s and 1970s. The basic premise of this theory is that adequate sensory processing in the nervous system plus the integration of sensory information in the brain will lead to adaptive behavior and functional abilities. The theory is based in neuroscience, developmental psychology, occupational therapy, and education.
Sensory integration theory proposes that sensory integration is the neurobiological process that organizes sensation from one’s own body and from the environment and makes it possible to one’s body effectively within the environment. The spatial and temporal aspects of input from different sensory modalities are interpreted, associated, and unified. Sensory integration is information processing and praxis and perception are both end products of sensory integration.
THE MAIN POINTS OF SENSORY INTEGRATION THEORY:
● An individual’s interaction with the environment influences the development of the brain.
● The nervous system is plastic, i.e. able to change.
● Sensorimotor experiences affect the brain’s plasticity.
● Sensorimotor development is a part of learning.
Sensory Input
This chart reviews the different types of sensory input.
| Type of Input | Description | Example | Photo/Video |
| Visual (sight) | Input that enters the brain through the visual structures in the eyes. Input is affected by levels of light and whether objects are standing still or moving. | A child watches a pinwheel spin in circles.
A teenager scans for and reads street signs while learning to drive. |
 |
| Auditory (sound) | Input that enters the brain through the auditory structures of the ear. Input is affected by volume and quality. | A teenager listens to music through headphones connected to his tablet.
A toddler babbles to himself to hear his own voice. |
 |
| Tactile (touch) | Input enters the brain through the small nerve endings under the skin. They get different feelings from texture, consistency and temperature (hot or its cold). | A child pets a soft kitten.
Two children squish homemade slime between their fingers. |
 |
| Olfactory (smell) | Input that enters the brain through the olfactory neurons in the nasal cavity. | A child repeatedly smells his teacher’s perfume.
A young woman uses an essential oil diffuser to help relieve her headache. |
 |
| Gustatory (taste) | Input that enters the brain through the taste buds on the tongue. | A small child licks glue to determine its taste.
A third grader sucks on sour candy to increase his level of alertness. |
 |
| Vestibular (balance) | Input that enters the brain through the structures of the inner ear. | A group of 5th grade students swing high on the playground swings and then jump off.
A 12 year old girl rides a scooter down the sidewalk. |
 |
| Proprioception (position in space) | Input that enters the brain through the stretch receptors in the muscles, ligaments, and joint tissues. | A group of 3rd grade girls play jump rope.
A 5 year old boy pulls a wagon with his 2 year old sister seated inside. |
 |
Sensory Processing Disorders
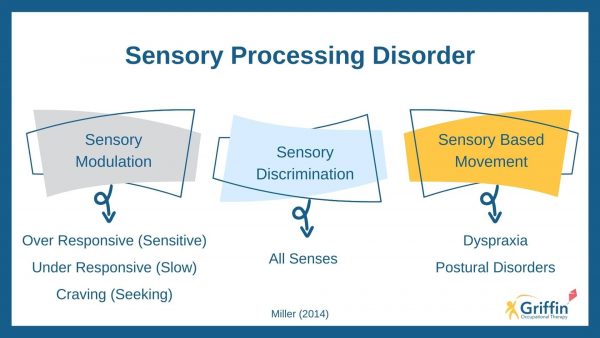
Sensory processing disorder is now an independent diagnosis. It is defined by the inability to adequately process sensory information from multiple sources, resulting in maladaptive responses to the environment. Sensory processing disorder is divided into three categories for diagnostic purposes.
| Category | Description | Example | Video |
| Sensory Modulation Disorder
|
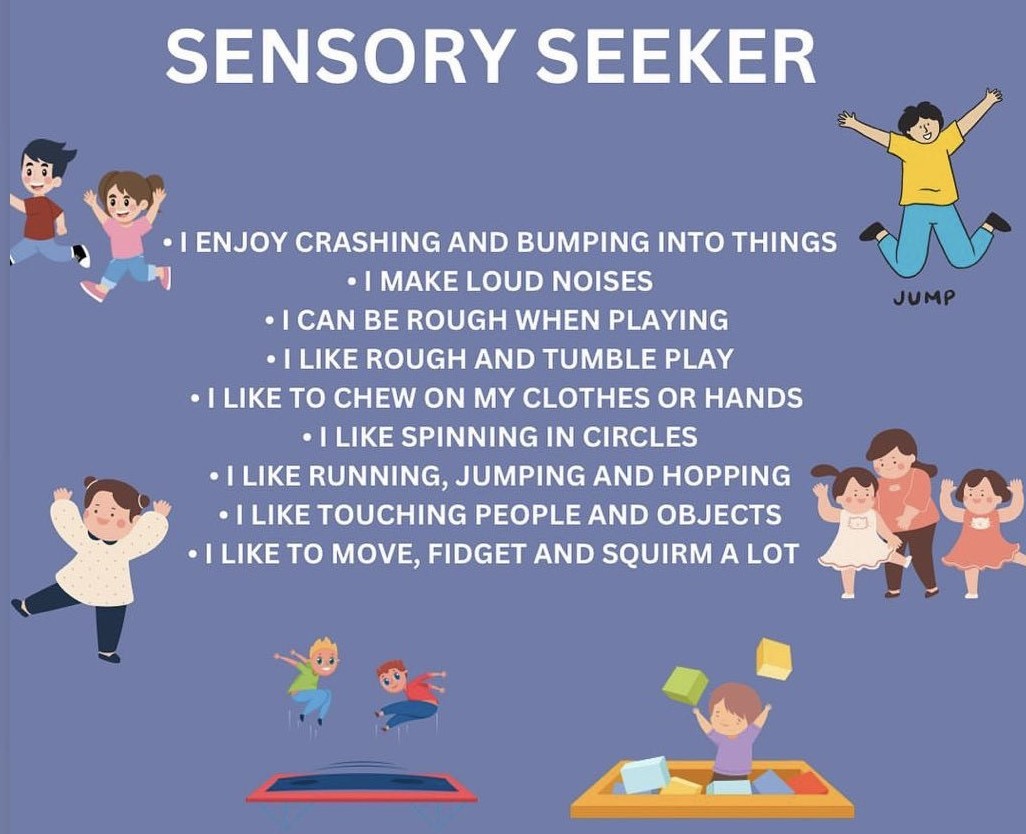
Difficulty adjusting the nervous system to changes in sensory input. -frequency -intensity -duration -complexity -novelty .. There are 3 subcategories of sensory modulation disorder: i. Sensory Over-responsivity ii. Sensory Under-responsivity iii.. Sensory Seeking.... i. Sensory Over-responsivity: * Responds to sensation faster, more intensely, longer duration. * Sensory overload causes a “Fight, Flight, or Freeze” reaction. * Can occur in one or more sensory systems * Difficulty in new environments * Sensory Defensiveness .. ii. Sensory Under-responsivity * Decreased awareness, orientation & response to sensory input * Requires intense sensory input to notice and therefore takes longer to respond * Appears sedentary, lethargic, apathetic * Mislabeled “lazy” or “unmotivated” as appears to lack inner drive for socializing .. iii. Sensory Seeking * Preference for intense & extreme sensory input. * Impulsive, intense, highly energetic, constantly moving, careless, restless, unsafe * High pain tolerance * Viewed as “Dare Devils” * Displays attention-seeking behavior |
A 9-year-old boy with autism spectrum disorder behaves normally in his classroom, but becomes distressed and covers his ears when he enters the school lunchroom.
A 13 year old boy with ADHD takes 2 minutes longer to organize his materials for his class than his peers, causing him to miss the main point of the teacher’s lecture. Sensory Over-responsivity Sensory Under-responsivity Sensory Seeking |
Therapists explain sensory modulation and use sensory modulation techniques with adult mental health patients.
Sensory over-responsivity – auditory system Sensory under responsivity – short animated video on tactile hyposensitivity |
| Sensory-based Motor Disorder | Incorrect processing of sensory information leads to motor problems that affect postural control and/or motor planning (praxis). | A 6 year old girl with Developmental Coordination Disorder cannot sit upright at her desk, but instead slouches forward and leans on her elbows.
A 7 year old boy with Sensory Processing Disorder attempts to use a ball chair to meet his movement needs in his classroom, but he keeps falling off the ball. |
Therapists discuss sensory-based motor disorders. |
| Sensory Discrimination Disorder | Incorrect processing of sensory input. | A 16 year old boy with autism spectrum disorder wears several layers of clothing to insulate himself from touching other people.
A three year old boy with autism stares for long periods of time and spins in circles when he sees rows of beads. |
A brief explanation of sensory discrimination disorder. |
..

Sensory processing disorder often occurs secondary to other diagnoses
The following chart reviews how sensory processing disorder manifests itself as a part of these diagnoses.
| Diagnosis | Associated Sensory Processing Difficulties | Example | Video |
| Autism Spectrum Disorder | Multiple sensory processing problems to varying degrees. | A 12-year-old boy with autism spectrum disorder obsesses over objects that light up or spin, spending a large portion of his day playing with and staring at objects that provide this type of input.
An 8 year old girl with autism spins rapidly when allowed to swing independently, obsesses over puzzles and electronic games, refuses to write on paper or complete simple work tasks, and screams, kicks, and throws objects when prompted to transition away from an activity that she prefers. |
A really cute kid with autism spectrum disorder explains sensory processing disorder. |
| Attention Deficit and Hyperactivity Disorder (ADHD) | -sensitive to visual input resulting in distractibility -under-responsive to auditory input -often seek vestibular and proprioceptive input |
A 7 year old girl with ADHD gets up from her desk in her classroom 5 times in a 10 minute period and requires 2-3 verbal cues from her teacher each time to return to her seat.
A 10 year old boy with ADHD does not display any behavior problems in his classroom but is never able to give appropriate answers when the teacher calls on him in class. |
2 OTs from the STAR Institute for Sensory Processing Disorder discuss their experience working with kids who have SPD and/or ADHD |
| Cerebral palsy | -sensitivity to sensory input, especially tactile, olfactory and gustatory input -difficulty interpreting vestibular and proprioceptive input -may have sensory symptoms that resemble autism. |
A 3 year old girl with cerebral palsy will only eat certain foods and requires encouragement to eat. She is afraid to sit on the swing in the therapy room.
A 3 year old boy flaps and twists his hands when he sees his favorite toy. |
An occupational therapist discusses sensory integration therapy for a child with cerebral palsy. |
| Traumatic brain injury | -Multiple sensory processing problems to varying degrees -sensory issues correspond to the damaged areas of the brain |
A 6 year old boy who sustained a traumatic brain injury 3 years ago loves to sit on the swing in the therapy room and spin or sit on the therapy balls and bounce.
A 17 year old teenager who sustained a traumatic brain injury at age two becomes upset and refuses to participate when his schedule changes without his being told ahead of time. |
An occupational therapist discusses sensory processing in patients diagnosed with traumatic brain injury. |
| Developmental Coordination Disorder, also called dyspraxia | -difficulty interpreting vestibular and auditory input -difficulty with sensory modulation -difficulty integrating sensory input to perform motor tasks |
A 10-year-old boy with Developmental Coordination Disorder is unable to judge the speed and direction that a ball is rolling in order to kick it during a game of kickball.
A 4 year old girl with Developmental Coordination Disorder wanders around her classroom and requires physical guidance from her teacher to locate and sit on her carpet square for circle time. |
A parent discusses her son’s problems with Developmental Coordination Disorder, also called dyspraxia. |
| Fragile X Syndrome | -Multiple sensory processing problems similar to autism spectrum disorder. -About 46 percent of males and 16 percent of females diagnosed with Fragile X Syndrome are also diagnosed with autism spectrum disorder. -Not every child with Fragile X displays sensory processing problems. |
A 5-year-old boy who has a diagnosis of Fragile X Syndrome flaps his hands every time he sees pictures of dinosaurs.
A 7 year old girl with a diagnosis of Fragile X syndrome requires a visual schedule to transition between classrooms during her school day. |
A child with Fragile X Syndrome and autism receives occupational and speech therapies. |
| Sensory Deprivation – children raised in deprived environments such as large orphanages, families with neglectful parents, foster homes, etc. | -difficulty with sensory modulation -difficulty with emotional regulation |
A 4-year-old boy who has been adopted by a local family from an eastern European orphanage does not like to be touched and laughs inappropriately at various situations with his peers.
A 5 year old boy seeks frequent hugs from his teacher and has frequent meltdowns when prompted to get ready to go home. |
The Impact of Isolation on the Neuroanatomy and Neurobiology of the Brain |
The following chart reviews evaluations for sensory integration and sensory processing skills.
| Test Name | Author/Year | Age Range | Method of Administration | Areas Evaluated |
| Sensory Integration and Praxis Tests (SIPT) | A. Jean Ayres, 1989 | 4-0 to 8-11 | The child is asked to complete activities defined on 17 different subtests. The tests may be administered separately or used together as a comprehensive evaluation. | -Visual, tactile, and kinesthetic perception -Motor performance. |
| Sensory Profile 2 Includes: -Infant Sensory Profile 2 -Toddler Sensory Profile 2 -Child Sensory Profile 2 -Short Sensory Profile 2 -School Companion Sensory Profile 2 -Spanish Caregiver Forms |
Winnie Dunn. Original Sensory Profile published 2002. Sensory Profile 2 published 2014. | Infant Sensory Profile 2 – birth to 6 months Toddler Sensory Profile 2 – 7 to 35 months. Child Sensory Profile 2, Short Sensory Profile 2, School Companion – 3 to 14 years. |
Questionnaires are completed by a child’s caregivers and teachers. | -Sensory System – discrimination of auditory, visual, tactile, movement, body position, and oral input -Behavior – attention, behavioral, social-emotional factors -Sensory Processing Patterns – registration, seeking, avoiding, sensitivity |
| Adolescent/Adult Sensory Profile | Winnie Dunn, 2002 | 11 years through adulthood | Questionnaire completed by the patient | Sensory Processing Patterns – registration, seeking, avoiding, sensitivity |
| Sensory Processing Measure and Sensory Processing Measure – Preschool | L. Diane Parham, et. al., 2010 | Sensory Processing Measure – 5 to 12 years. Sensory Processing Measure, Preschool – 2 to 5 years (prior to beginning school). |
Questionnaires completed by the child’s caregivers, teachers, and other adults who may observe the child in the school setting. | Sensory Systems – social participation, vision, hearing, touch, body awareness (proprioception), balance and motion (vestibular), planning and ideas (praxis). -systems evaluated in both school and home settings. |
| Test of Sensory Function in Infants (TSFI) | Georgia A. Degangi and Stanley I. Greenspan, 1989 | 4 to 18 months | Twenty four items administered through simple interaction with the infant. | Overall sensory processing as well as these subdomains: -Reactivity to tactile deep pressure -Visual tactile integration -Adaptive motor function -Ocular motor control -Reactivity to vestibular stimulation |
| -Berk Test of Sensory Integration | Georgia A. Degangi and Ronald A. Berk, 1983 | 3 to 5 years | Children are asked to perform 36 test items that are scored on a numerical scale. | Overall sensory processing as well as these three subdomains: -Postural Control -Bilateral Motor Integration -Reflex Integration |
Occupational Therapy Treatment for Sensory Processing Disorders
The goal of sensory integration intervention is to improve the processing and integration of sensory information to allow participation in childhood occupations, including activities of daily living, school work, extracurricular activities, and play.
General Principles
1. The focus of treatment is primarily on tactile, vestibular, and proprioceptive processing. These three systems form the base for other sensory processing.
2. Treatment should provide a “just right challenge” – an activity that is challenging but at the same time realistic for the child to achieve.
3. The treatment environment should be enticing, encouraging the child to actively engage in play.
4. Treatment is child directed. The child directs treatment by giving behavioral cues that the therapist observes and reads. The therapist adjusts treatment based on these cues that indicate what the child wants and will find enticing.
Treatment for Specific Sensory Processing Problems
| Sensory Processing Problem | Focus of Treatment | Examples of Activities | Photo/Video |
| Tactile Defensiveness
-does not like to be touched |
Desensitize the nerve endings near the surface of the skin to decrease the child’s sensitivity to touch. | Wilbarger® brushing protocol (see below)
Wrapping in a heavy blanket to play “hot dog” or folding a large beanbag over a child to play “taco” Rolling a soft “rolling pin” on a child’s back. “Squishes” using hands, hugs, a therapy ball on the back, or other similar techniques. Play with toys in textures graded from non threatening (i.e. sand or plush toys) to more aversive textures (shaving cream, slime, feathers). |
Occupational therapy students demonstrate sensory activities for children with tactile defensiveness that can be completed at home. |
| Difficulty Regulating Levels of Arousal
-jumping around frequently |
Provide proprioceptive input in the form of “heavy work” so a child can feel their body’s position in space and know how fast or slow they are moving at a given point in time. | Catch with a weighted ball or a large therapy ball.
Roll in or find toys in a ball pit (an area with foam or inflated boundaries filled with small plastic balls). Crawl in a stretchy lycra tunnel or play “blob” in a body sock (a stretchy bag-like object). Jump or roll on a crash mat. Wheelbarrow walks or donkey kicks. |
An occupational therapist provides treatment to a child using activities that provide proprioceptive input. |
| Craving movement
-always running |
Provide graded vestibular activities to help meet the child’s movement needs. Activities should be introduced gradually in a nonthreatening way for children who are sensitive to movement. Higher level challenges can be introduced for children who crave movement. | Swinging in or on a variety of swings, grade activity from slow movement with feet on floor for hypersensitive children to high swinging for under – responsive children.
Rolling on a scooter board to pick up toys. Swinging prone on a swing to put together a puzzle. Rolling prone on a scooter board to play “human bowling ball” and knock down plastic pins. Standing on a balance board to toss bean bags. Jumping on a small trampoline. Sitting on a therapy ball to play catch. Rock in a glider rocker. |
A therapist demonstrates balance activities with a child for vestibular input. |
| Difficulty with tactile discrimination
-does not notice when face or hands are dirty |
Provide activities that will stimulate the nerve endings just under the skin, arousing the tactile sensors. | Play with tactile media – sand, dried beans, dry rice, pom pon balls, shaving cream, play doh, etc.
Jump or roll in a pile of pillows with different textures. Play games that require feeling and identifying objects with vision occluded, i.e. Ned’s Head®. Construct art projects using a variety of tactile media. |
A child with multiple disabilities engages in tactile activities for sensory input. |
Adaptations for Sensory Sensitivity or Sensory Modulation Problems
| Problem | Purpose of Adaptation | Examples | Photo/Video |
| Auditory defensiveness | Decrease the amount of auditory input to reduce a child’s distress when around loud noises or in crowded areas. | -Noise reducing headphones -Ear plugs -Instruction or testing in a quiet room with fewer students present -Foreshadowing before loud noises are going to occur (i.e. discussing a fire drill ahead of time). – Allow child to work in a quieter place to focus on classroom tasks |
 |
| Sensitivity to light or certain light frequencies (i.e. fluorescent lights) | Block or filter light to offset frequencies, increase access to natural light. | -Sunglasses -Visors -Filter covers over fluorescent light fixtures. -Lamps for soft lighting. -Turn off lights on sunny days and use natural light. |
 |
| Tactile Defensiveness | Provide deep pressure input to desensitize the nerve endings just under the skin. | -compression garments or tight-fitting undergarments, i.e. Under Armour® -remove tags on clothing or tagless clothing -seamless socks -slip-on shoes -extra space at tables where the child must sit with other children. -defined space during carpet time or assemblies. |
 |
| Difficulty with Modulation | Provide adaptations to foreshadow activity and environment changes during the day. | -visual schedules -visual or auditory timers -written instructions -checklists or mini schedules for specific tasks. -foreshadow changes in the schedule, special events |
 |
| Difficult Regulating Level of Arousal | Provide adaptations that will allow movement outlets and/or provide input to increase arousal | -wiggle cushion – an air filled cushion that facilitates movement. -ball chair – child sits on a therapy ball with a base. -standing desk – a desk that allows a child to sit or stand and often has a moving bar for the child’s feet. -chewy gum or candy -ice chips -aromatherapy -movement breaks |
 |
Collaboration with Teachers, Paraprofessionals, Caregivers
Sensory processing disorders affect all areas of a child’s life. For this reason, sensory treatments and adaptations must be carried over both at home and in the school environment. Occupational therapists work with parents, caregivers, teachers, and paraprofessionals to educate them in why children behave the way they do when they have sensory processing difficulties and how they can make changes to help a child adapt and develop sensory processing skills. This section will discuss techniques used to help families and educators follow through with sensory integration treatments.
1. Sensory Diets
a. A sensory diet is a schedule of sensory activities and adaptations specially designed to help meet a child’s sensory processing needs.
b. Sensory diets are designed by the occupational therapist and are custom for each child.
c. The activities in a sensory diet are usually performed according to a daily schedule so the child gets the right amount of sensory input at the right times.
d. Caregivers and educators should be educated in how to provide the activities and adaptations included in a sensory diet.
e. Sensory diets used at school should be documented in a child’s IEP or 504 plan.
2. Wilbarger® Brushing Protocol
a. A specific protocol to reduce tactile defensiveness.
b. Administered using a surgical scrub brush.
c. The protocol must be administered according to the protocol developed by Patricia and Julia Wilbarger, a mother-daughter team of occupational therapists. The Wilbargers are also credited with coining the phrase “sensory diet”.
d. Therapists should be trained in administration of the protocol before using it with children or training caregivers or teachers in its use.
Equipment and toys commonly used in a SI setting
Ball Pit 

The brightly colored balls inside the ball pit create a rainbow sea of fun and are a great therapeutic tool for SI therapy.
From a therapeutic perspective the balls provide tactile stimulation and proprioceptive feedback.
• The balls provide buoyant support, deep-pressure sensation and encourage relaxation.
• Moving through the ball pit to find hidden toys stimulates the tactile, proprioceptive and visual systems and requires motor planning.
• Hanging on to a ladder or zipline and falling or crashing into the ball pit activates the vestibular and proprioceptive system.
- A safe alternative to biting on one’s hands, shirt collars/sleeves, pencils.
- Can be incorporated into a child’s “sensory diet” to regulate their systems.
- Useful and practical tool that can be used with children who experience:
- Stress and anxiety
- Difficulty concentrating
- Limited oral awareness and seek out ways to increase their oral feedback
Chewable toys have two important functions:
1. They provide direct sensory input and oral stimulation for the mouth which is perfect for those kids who put inedible objects in their mouth in order to seek oral stimulation. Chewing provides proprioceptive feedback to satisfy the the need for sensory input that children may be seeking in their mouths.
Chewing toys can be used as an oral motor tool to:
– provide tactile stimulation (textured surface) to the gums and lips
– practice biting/chewing skill
– build up jaw strength
2. They also provide calming and self-regulation
Helps children with ASD and/or a sensory processing disorder who need to chew to become calm, focused, and self-regulated.
Chewing:
– provides proprioceptive input to the jaw that is very calming and organizing
– can be a very effective way to increase focus
– activates muscles in the jaw down into the neck, which provides added stability
Therapeutic Swings


Vestibular Stimulation
Movement is essential for typical development to occur in all children.
Swinging, jumping, spinning and rocking are important to children not only for fun and exercise but also to help their bodies organize sensory information and to regulate their sensory systems.
Vestibular input is one of the core elements of sensory integration therapy.
Swinging can have a powerful impact the brain’s ability to process and use sensory information. Whether the child is linear swinging on a strap swing, cuddled up in a net swing for proprioceptive input or spinning in a rotating movement, all of these movements can act as a powerful activator on the body’s systems.
Some children crave movement, while others may be sensitive to movement. Controlled vestibular input under the direction of an OT is used with children who have sensory processing issues.
PRAXIS
The term “praxis” was originally coined by A. Jean Ayres, the founder of Ayres Sensory Integration Therapy.
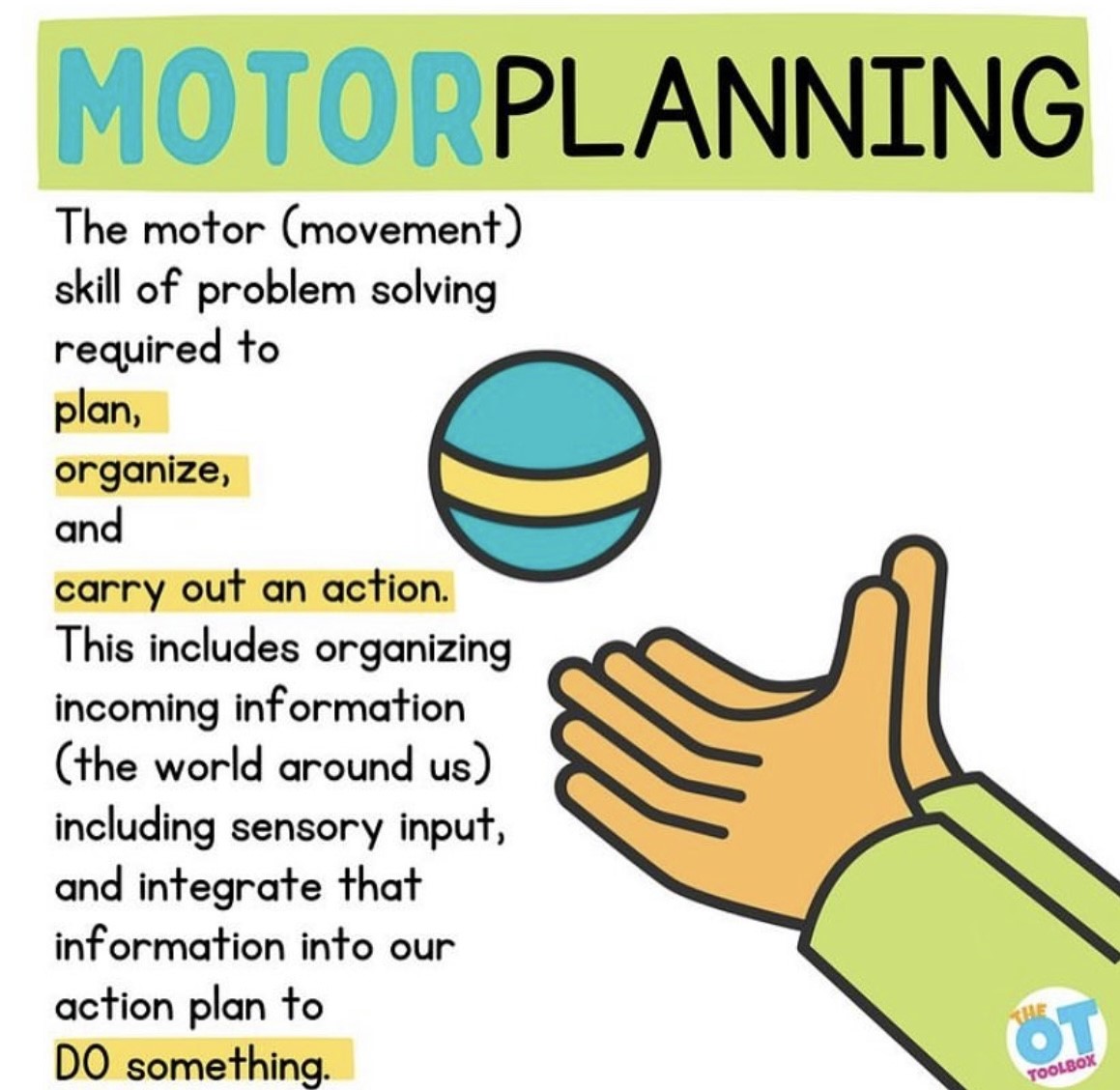
According to Ayres, “Praxis is the neurological process by which cognition directs motor action.” Praxis is the ability to conceptualize, plan, organize, and execute a new action. Praxis is an intricate process intertwining motor, sensory, and cognitive skills.
Praxis can be broken down into 4 steps:
1. Ideation – This is the ability to form an idea.
2. Motor planning – This is where the organization and plan for the idea happens. This includes understanding when and how to move the body and/or objects.
3. Execution – This is the actual performance of the idea.
4. Feedback and adaptation – This is being able to identify how the task went, identify any areas of improvement, and make those changes.
In simpler terms, praxis refers to the ability to conceive, plan, and carry out a skilled, non-habitual motor act in the correct sequence from beginning to end. It relies on sensory feedback from the body and the environment as well as on memory and other cognitive skills. It involves understanding what needs to be done (forming an idea), working out how to carry out the task (e.g., which steps need to be done first), before actually doing the task (co-ordinating the body and movements to achieve the desired result).