Quick Reference to Common
Quick Reference to Common
Precautions/Contraindications
SAFETY FIRST
| Precaution/Contraindication | What can happen
|
What to do in this situation | ||
| JOINTS | Lower back | 1. No bending at the waist. 2. No lifting – will have lifting precautions in place. 3. No twisting at the waist. |
Possible damage to what has been done during surgery and interference with healing process. | PREVENTION
• Educate the patient in body mechanics to avoid bending at the waist, lifting and twisting. |
| Hips | Anterior Approach: 1. Avoid extension of the hip backward. Do not step backwards with surgical leg. 2. Avoid external rotation of the hip. 3. Avoid hip adduction. Do not cross legs. Use a pillow between legs when rolling. .. Posterior Approach: 1. Avoid hip flexion past 90 degrees. 2. Avoid hip adduction (no crossing legs). 3. Avoid hip internal rotation. |
Possible dislocation of hip joint | PREVENTION
• Educate the patient and patient’s caregivers in hip precautions. |
|
| Knees | 1. No squatting. 2. No kneeling on the affected knee. 3. No pivoting or twisting the affected knee. 4. Knee must be flat when lying in bed. 5. Knee may be immobilized post-surgery – specific precautions may be ordered by the surgeon. |
Stress on the knees | PREVENTION
• Educate patient and patient’s caregivers in post surgical precautions. |
|
| RA- Flare-up Acute/Exacerbation
|
1. Heat: Acutely inflamed joints may be exacerbated by heat, whereas ice may be more helpful in reducing pain and inflammation. Patients with RA often have unstable vascular reactions to heat and cold that cause greater than normal heat retention with heat agents or increased coldness and stiffness with cold exposure.
2. Active ROM can exert more stress on a joint compared to gentle passive ROM. 3. Resistance: 4. Isotonic exercises 5. Active or passive stretches 6. Inappropriate use of splints |
• Exacerbate inflammation and pain • Joint integrity can be compromised and the risk of developing and/or progressing deformities can be increased. – Active ROM can exert more stress on a joint than gentle passive ROM, so passive ROM exercises may be safer. – Inappropriate use of splints can be harmful |
PREVENTION
• Respect pain: use this as a signal to change activities. • Reduce forces on joints • PAM: Acutely inflamed joints may be exacerbated by heat, whereas ice may be more helpful in reducing pain and inflammation. In the subacute or chronic stages, heat or cold may be equally effective. Careful monitoring of patient responses to PAMs is crucial due to sensory issues. • Gentle passive ROM exercises are safer. • Functional activities as tolerated, isometric exercises and rest. • Splinting: patient’s comfort should always take precedence, and joints should never be forced into the ideal position. The splint is worn continually for the duration of the flare-up and removed at least once a day for skin hygiene and gentle ROM exercises. Splint use should continue full-time for at least 2 weeks after the flare subsides, with a gradual decrease in wearing time to allow the joints to recover. • Isometric exercises are usually the least painful for patients with RA because they eliminate joint motion and can be as effective or more effective in improving muscle strength and endurance. Isometric contractions are generally held for 6 to 12 seconds. • Exercise: General guidelines for exercise in patients with arthritis are to avoid undue joint stress, avoid pain and joint swelling, and work within the patient’s comfortable ROM. Exercises to maintain ROM should be performed at least once daily, even during a flare-up. As a good rule of thumb, pain lasting greater than 1 or 2 hours after completion of exercise signals a need to modify or decrease an exercise |
|
| PAMS | Children
Active epiphysis- (generally 16 years old or younger, although the plate may not close in some individuals until between ages 18 and 25) |
Ultrasound | Ultrasound over unfused epiphyseal growth plates may alter bone growth. | AVOID USING |
| Hypertension |
• Cryotherapy • Superficial Heat |
Cold increases, sympathetic tone and produces peripheral vasoconstriction, which increases blood pressure Generalized peripheral vasodilatation is produced by heating a large surface area of the body. Elevation in skin blood flow requires more cardiac output in order to maintain blood pressure. People with impaired heart function may not tolerate the increased cardiac demand |
AVOID USING | |
| Malignancy | • Electrical stimulation (all forms) • Superficial Heat • Ultrasound |
E-stim may stimulate growth and promote spread of cancer cells
Superficial Heat- Increasing tissue temperature stimulates metabolic activity of all types of cells. Ultrasound Sound- waves applied to tumor cells can stimulate growth and induce new blood vessel growth, which helps provide fuel for further tumor growth and potentially promotes metastases. |
AVOID USING | |
| Pacemaker | • Electrical stimulation (all forms) • Ultrasound |
Electrical stimulation (all forms) may cause malfunction
Ultrasound may affect the function of pacemakers
|
AVOID USING | |
| Pregnancy | • Superficial Heat • Electrical stimulation (all forms) • Ultrasound |
Superficial Heat – heating fetal tissues can alter fetal growth and development.
Electrical stimulation (all forms) – may lead to unwanted uterine contractions and, potentially, to miscarriage or premature labor. Ultrasound- Sound waves transmit through amniotic fluid and could cause fetal malformations |
AVOID USING | |
| Raynaud’s Phenomenon
Sudden constriction of a blood vessel that reduces blood flow |
• Cryotherapy /Cold pack | In Raynaud’s disease, the blood vessels are commonly in a state of vasospasm, which would be exacerbated by applying cold. Prolonged vasoconstriction can lead to thrombus formation, tissue ischemia, and necrosis. | AVOID USING | |
| Seizures | Electrical Stimulation (all forms)
|
May induce seizures | AVOID USING | |
| Sensory Impairment | • Electrical Stimulation (all forms) • Cryotherapy • Superficial Heat • Ultrasound • Whirlpool |
Impaired sensation that prevents patients from giving accurate and timely feedback can be harmful.
Electrical Stimulation (TENS, NMES)- unable to distinguish the prescribed and/or maximum safe level of current intensity. |
AVOID USING | |
| SPLINTS | Flexor Tendon Injury | Position of hand
|
Tendons can rupture
|
Splint in FLEXION |
| Extensor Tendon Injury | Position of hand
|
Tendons can rupture
|
Splint in EXTENSION | |
| SCI | Autonomic Dysreflexia (AD)
– Sudden onset of excessively high blood pressure.
|
Recognize the symptoms, and understand the causes. – T6 and above – More common with cervical and complete lesions. Common Causes: – Bladder distension – most common triggering factor – Bowel distension – Pressure ulcer . Symptoms: • High blood pressure • Pounding headache • Flushed face • Sweating above the level of injury • “Goose bumps” below the level of injury • Nasal stuffiness • Nausea • Slow pulse (slower than 60 beats per minute). |
MEDICAL EMERGENCY
Life-threatening condition |
“The Five B’s”
1. Bed Up BED UP: Sit the patient up or raise their head to 90 degrees. Lower their legs if possible. Loosen any tight clothing and/or constrictive devices/splints/ braces-especially around the torso and quickly check the catheter for blockages. BP: Closely monitor BP- every 5 mins or more. Search for and eliminate the trigger BLADDER: Check bladder drainage equipment for kinks or other causes of obstruction to flow BOWEL: Check if impacted BODY: Skin issues |
| Orthostatic Hypotension (OH) Also known as: Postural Hypotension– Drop in blood pressure that occurs when a person stands up from sitting or lying down. |
Recognize the symptoms, and understand the causes.
Commonly seen with cervical and high thoracic lesions Symptoms: |
Patient could faint Associated with fatigue and impacts quality of life and participation in rehabilitation. May result in deficits in cognitive performance. |
For an acute episode: The patient must be reclined quickly and, if sitting in a wheelchair, should be tipped back with legs elevated until symptoms subside.
Other management strategies include: |
|
| NEURO | – an autoimmune neurodegenerative disease characterized by demyelination of the CNS.
|
Temperature sensitivity- neurological symptoms are temporarily exacerbated by environmental or exercise-induced increases in body (core and skin) temperature.
Contraindications:
|
Heat sensitivity (Uhthoff’s phenomenon)- increases in core body temperature as little as ~ 0.5°C can trigger temporary symptoms worsening. This phenomenon is generally triggered by exposure to warm environments, hot baths, or exercise and lasts until core temperature returns to baseline values. Decreases in body temperature resulting from cold baths or exposure to cold ambient temperatures can also trigger a worsening of clinical symptoms.
|
Avoid extremes of either hot or cold.
Avoid extreme physical stress
|
| Amyotrophic Lateral Sclerosis (ALS)
– neurodegenerative disease that causes degeneration of the lower and upper motor neurons and is the most prevalent motor neuron disease. Characterized by muscle weakness, stiffness, and hyperreflexia.
|
Progressive resistive exercises | Progressive resistive exercise to strengthen muscles may cause cramping, fatigue | ||
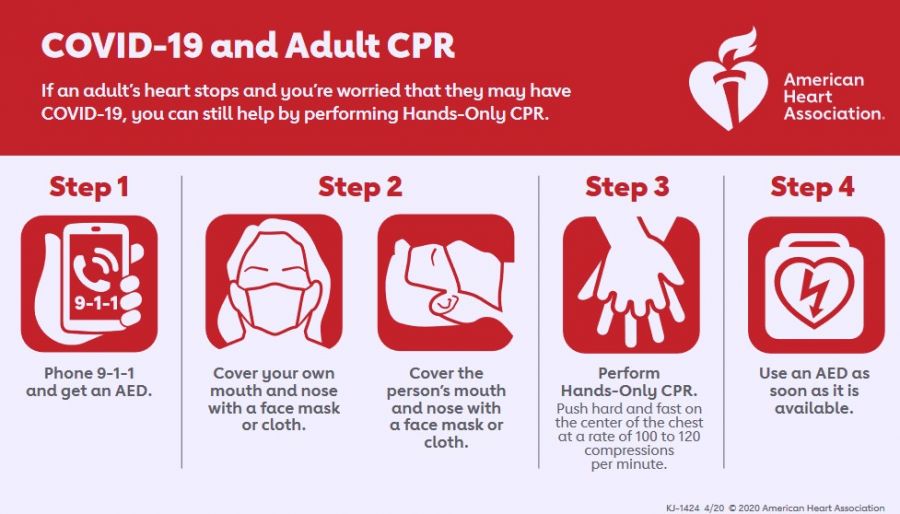
| MEDICAL | Cardiac Arrest & Heart Attack– also known as: Myocardial Infarction … A heart attack can lead to cardiac arrest. A heart attack needs immediate medical attention but doesn’t need CPR. If a heart attack leads to a cardiac arrest, then CPR is needed. … Some heart attacks strike suddenly, but many people have warning signs and symptoms hours, days or weeks in advance. The earliest warning might be recurrent chest pain or pressure (angina) that’s triggered by activity and relieved by rest. Angina is caused by a temporary decrease in blood flow to the heart. |
Do not wait to see if the symptoms go away. Do not give the patient anything by mouth unless a heart medicine (such as nitroglycerin) has been prescribed. … Symptoms: • Pressure, tightness, pain, or a squeezing or aching sensation in chest or arms that may spread to the neck, jaw or back • Nausea, indigestion, heartburn or abdominal pain • Shortness of breath • Cold sweat • Fatigue • Lightheadedness or sudden dizziness |
A heart attack is a life-threatening emergency
Time is critical in treating a heart attack, and a delay of even a few minutes can result in permanent heart damage or death. |
Act fast. Call for a medical assistance immediately. Prepare to perform CPR if necessary. CPR **Refer below for more detail |
| COPD | Anything between 92% and 88%, is still considered safe and average for someone with moderate to severe COPD. | Below 88% becomes dangerous, and when it dips to 84% or below, medical intervention is necessary. Around 80% and lower is puts vital organs in danger. | • Follow doctor’s guidelines regarding the patient’s oxygen levels during activity. • If oxygen level falls below doctor’s guidelines or below 90%, stop activity and allow rest until oxygen level returns to acceptable percentage. • If oxygen level does not return to an acceptable, end therapy session and contact the patient’s physician. • Having a pulse oximeter to test during and after exertion/Being within reach of a vitals machine. |
|
| Deep Vein Thrombosis (DVT)
Deep vein thrombosis can cause leg pain or swelling but also can occur with no symptoms.
|
Recognize the symptoms • Swelling in the affected leg. Rarely, there’s swelling in both legs. • Pain in leg. The pain often starts in the calf and can feel like cramping or soreness. • Red or discolored skin on the leg. • A feeling of warmth in the affected leg. … All PAMs are contraindicated, including: • Cold Therapy • Hot Therapy • TENS • Ultrasound |
Pulmonary Embolism (PE) is a life-threatening complication of DVT
The warning signs and symptoms of a pulmonary embolism include: |
||
| Diabetes
Wound healing Hypoglycemia Hyperglycemia |
Recognize the symptoms, and understand the causes.
Wound healing Hypoglycemia Hyperglycemia |
WOUND CARE Diabetic wounds are likely to progress into a deep infection that kills healthy tissue and delivers infection directly into your bone. This type of infection is hard to stop once it begins, making amputation the only procedure capable of halting the spread of infection and saving the patient’s life. Most common diabetic amputations occur on the toes, feet, and lower legs. Diabetes is the leading cause of non-traumatic lower extremity amputation. .. HYPOGLYCEMIA If diabetic hypoglycemia isn’t treated, signs and symptoms of severe hypoglycemia can occur and can lead to serious problems, including seizures or unconsciousness, that require emergency care. .. HYPERGLYCEMIA It’s important to treat hyperglycemia, because if left untreated, hyperglycemia can become severe and lead to serious complications requiring emergency care, such as a diabetic coma. |
WOUND CARE: PREVENTION Teach proper diabetic wound care- protect wound from infection and help the healing process. .. HYPOGLYCEMIA HYPOglycemic episode- offer carbohydrates (candy, fruit, juice, honey) .. HYPERGLYCEMIA HYPERglycemia episode- may need insulin & IV intervention |
|
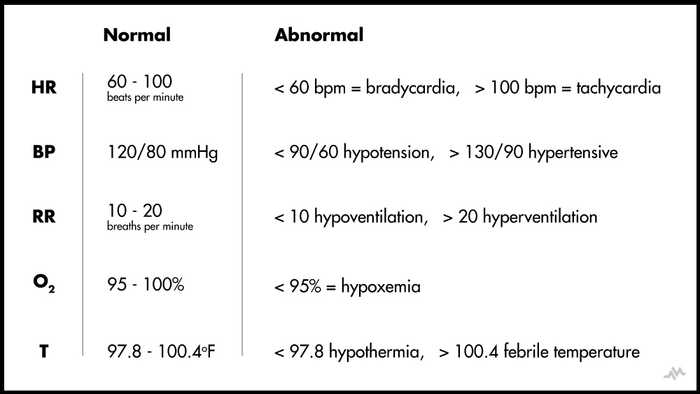
| Vital Signs | Know the values and symptoms
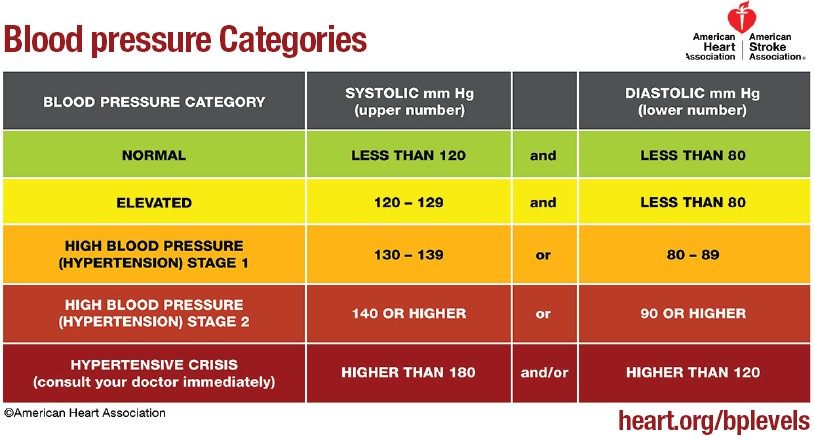
In healthy adults at rest, normal values are as follows: BP HYPERTENSION Respiratory Distress Lower than 92% is considered hypoxic. Signs of hypoxia: Since vital signs are an indication of the changes in physiological processes, they tend to change with age. With age, core body temperature tends to be lower, and the ability of the body to change with different kinds of stressors becomes minimized. Even subtle variation in core body temperature can be a significant finding as fever in an older patient often indicates a more severe infection and is associated with increased rates of life-threatening consequences **Refer to diagrams below for more information |
HYPOTENSION: Extreme hypotension can result in this life-threatening condition
HYPERTENSION HYPOXIA |
PREVENTION:
Knowing how to read vital signs and noticing a patient’s non-verbal behavior will guide the OT practitioner as to how the patient is coping and whether the session needs to be terminated. It is importance to monitor patients’ vitals. Take baseline measurements and monitor the impact of physical interventions on the patients’ vitals. If baseline vitals are not within normal or recommended range, do not provide OT intervention. |
|
| PEDIATRICS | Down’s Syndrome | Atlantoaxial instability (AAI) – a misalignment of the first two cervical vertebrae of the neck
|
Neurologic symptoms can occur when the spinal cord or adjacent nerve roots become affected.
Neurologic symptoms of symptomatic AAI include: |
PREVENTION
Avoid activities that place the neck in excessive flexion or extension, such as gymnastics. |
| Shunt malfunction
|
Recognize the symptoms
Infants Toddlers Children and Adults |
When an abrupt malfunction occurs, symptoms can develop very rapidly potentially leading to coma and possibly death. In infants and toddlers, it’s important to be aware that medication with a side effect of drowsiness can mimic or mask signs of shunt malfunction |
..CPR
The American Heart Association recommends starting CPR with hard and fast chest compressions.
• Untrained
If you’re not trained in CPR or worried about giving rescue breaths, then provide hands-only CPR.
That means uninterrupted chest compressions of 100 to 120 a minute until paramedics arrive (described in more detail below). You don’t need to try rescue breathing.
• Trained but rusty
If you’ve previously received CPR training but you’re not confident in your abilities, then just do chest compressions at a rate of 100 to 120 a minute.
• Trained and ready to go
If you’re well-trained and confident in your ability, check to see if there is a pulse and breathing. If there is no pulse or breathing within 10 seconds, begin chest compressions. Start CPR with 30 chest compressions before giving two rescue breaths.
Remember C-A-B
• C: compressions (Stayin’ Alive’s tempo is 103 beats per minute)
• A: airway (Current recommendations suggest performing rescue breathing using a bag-mask device with a high-efficiency particulate air (HEPA) filter.)
• B: breathing
VITAL SIGNS