The following charts review some of the more common pediatric diagnoses, including causes, common problems, and occupational therapy intervention.
| Diagnosis | Cause(s) | Problems | Occupational Therapy Intervention | Video |
| Acquired Brain Injury – a loss of consciousness that lasts from 0 minutes to over 6 hours with posttraumatic amnesia that can last from less than an hour to over 24 hours. | Accidental and non-accidental trauma, motor vehicle accident, falls, anoxia to the brain, infections such as meningitis. | -Unable to complete basic self-care tasks -Unable to write -Delayed processing of information -Expressive, receptive or global aphasia -Decreased postural control -Ataxic motor movements -Visual impairments -Sensory damage |
–ADL retraining with hand over hand assist/sequence pictures as needed. -Adaptive toys -Non-slip mats -Low stimulated and group learning environments -Increased time to complete home and school activities -Positioning equipment for seating and for extremities -Address concentration/sustained attention with grading time for tasks -External supports for memory -Activities to improve direction following -Natural weight bearing to decrease ataxic motor movements |
A teenager and her family describe her experience with an acquired brain injury |
| Attention Deficit Hyperactivity Disorder | Unknown. Can occur as a primary condition or along with other developmental or psychiatric conditions | Inattention, Impulsivity, Hyperactivity | –Encourage consistent routines -Limit background noises -Provide concise and clear directions -Write notes and use checklists -Encourage verbal responses vs written responses in the classroom as able -Limit distractions in the environment by providing quiet areas with only essential items and facing work surfaces toward walls -Eye-tracking activities -Gross motor games that develop body awareness and coordination -Calming strategies |
Cute video of a little girl explaining her life with ADHD. |
| Autism Spectrum Disorder | Unknown | -Impaired communication and social interaction skills
-repetitive patterns of behavior -excessive routines, inflexible -lack of reciprocal interactions -decreased awareness of environment |
-Examine sensory processing and modulation and provide appropriate sensory input or decrease input as necessary (visual; tactile; vestibular; auditory; proprioceptive; olfactory; oral)
-feeding/eating therapy to increase repertoire of food preferences for improved nutritional intake -develop body awareness to improve motor planning through massage, swings, weighted materials, hanging activities -educate caregivers on – peer mediated approach is designed to teach typically developing children ways to help children with ASD. This intervention trains peers to form a social “network” to provide support for children with ASD in their classroom. Peer-mediated instruction and intervention is based on principles of behaviorism and social learning theory. In this approach, typically developing peers are taught ways to interact with and help children with ASD acquire new social skills by increasing social opportunities in natural environments. Students with autism are then able to model the behavior of their peers, while their peers learn how to interact with and advocate for the students with autism.
|
A father explains how occupational therapy helps his daughter who has autism.
An example of the peer mediated approach in an elementary school. |
| Child Abuse, Child Neglect and Shaken Baby Syndrome | Child is a victim of physical, emotional, or sexual abuse or neglect of proper care and nutrition resulting in physical harm. | -delayed growth, delayed development and/or cognitive deficits -injuries inside the brain resulting in nerve cell damage, brain swelling and bleeding -injuries outside the brain resulting in retinal bleeding-rib fractures -bruises -abdominal damage |
-ADL training in self- care tasks -address academic success by providing school-based OT as necessary -gross motor and strengthening activities to increase postural control -visual-perceptual and visual-motor activities to address visual inattention, visual scanning deficits and visual motor integration -symbolic play, social stories and art activities to promote expression of feelings -sensory processing examination and providing appropriate sensory input to regulate/modulate sensory systems for calming -bilateral integration activities -coping strategies For calming babies: -swaddling -swinging -deep pressure and warmth -massage/gentle touch -soft, soothing music and sounds |
An occupational therapy graduate student shows how OT helps abandoned children (in Armenian and English). |
| Cystic Fibrosis | A genetic disorder caused by mutations in the gene for the cystic fibrosis transmembrane conductance regulator. | Accumulating thick, sticky mucus that causes coughing, shortness of breath, and frequent chest infections. Other symptoms include: -poor growth -poor weight gain -salty sweat -fatty bowel movements -trouble digesting food -enlarged heart |
-Training in daily routine management, including medications and respiratory treatments. -Education in energy conservation techniques during ADLS and IADLs. -For adolescents, training in self- management of disease, transitioning away from parents to independence. |
A teenage boy demonstrates self-management of his breathing treatments. |
| Developmental Delay | Usually caused by other conditions or disorders | Excessive functional limitation in one or more of the following areas: self-care, communication, motor development, sensory processing, social skills, cognition. |
-determine underlying diagnosis to facilitate OT intervention -self-care training -sensory strategies as appropriate -smaller step learning for developing complex skills and concepts -visual supports -gross-motor activities -construction tasks -fine motor activities -postural activities -UB strengthening and coordination -backward chaining -coping skills training -social skills and turn- taking |
Pediatric occupational therapists and parents of children explain how occupational therapy helps to address developmental delays. |
| Developmental Coordination Disorder (Dyspraxia) | Unknown | Clumsiness. Excessively delayed motor development that negatively influences daily functional tasks such as ADL or school activities and is not related to any other diagnoses. | -Clothing such as pullover garments and elastic pants until child develops ability to manage fasteners (zip, button, snap)
-provide alternatives to fork and knife use until able to manage cutting meats etc. -adaptive scissors for cutting -sensory-based tasks to develop motor planning -activities to develop postural control and stability -teach how to plan and check for progress -provided environmental modifications as necessary (computer, handwriting modifications, line guides, arm rests on chairs) -break occupations and |
A mother explains how dyspraxia affects her son. |
| Down Syndrome | Trisomy 21 – an extra copy of chromosome 21 due to an error in cell division. | Slanted eyes, protruding tongue, flat nose, epicanthal fold over the eyes, shortened fingers and limbs, hypotonia and hyperextension of joints, delayed development of reflexes, delayed or impaired sensory development, cognitive impairment, may have heart defect, creases in the hands. |
-place food to sides of mouth to encourage lip closure while eating -repetitive activities to promote mastery of skills -compensatory strategies for ADLs -early intervention and school based OT to promote intellectual development, incorporating problem solving, organization skills, life skills, vocational skills and social skills training so that child is prepared for transition from school to work |
An explanation and demonstration of occupational therapy for a child with Down Syndrome. |
| Failure to Thrive | Medical or environmental factors. Home environment may influence condition. | -body weight is well-below normal weight of peers of the same age range
-feeding difficulties -delays in age-appropriate self-care skills, play skills and/ or cognitive |
-Oral motor skills, eating/feeding schedule based on child’s expression of hunger
-food additives for increasing calories -small portions with frequent mealtimes -nutrition monitored for proper balance -food play -establish daily routine with regular eating times -compensatory strategies -remediation |
A mother describes her son’s battle with failure to thrive. |
| Fetal Alcohol Syndrome | Excessive alcohol intake of the mother during pregnancy, resulting in various birth defects. | -neural abnormalities
-facial abnormalities -cranial abnormalities -cardiac abnormalities -delays in cognitive and physical development -fussy -poor coordination -deficits in sensory processing -visual impairments |
-monitor vital signs as necessary
-organizational, proprioceptive activities such as wheelbarrow walking, climbing, pushing loaded carts -motor planning tasks such as obstacle courses and mazes -appropriate sensory diet -calming tasks including deep pressure, “cuddling” activities -use schedules and timers to prepare for transitions -break tasks into smaller segments -gross motor activities to develop body awareness, coordination, and alerting behaviors and cognition, i.e. tug of war, running races, hanging on a bar -visual motor activities such as stringing beads, dot to dot, block construction -visual perceptual activities such as hidden pictures and letter/number recognition |
An occupational therapist discusses fetal alcohol syndrome. |
| Intellectual Disability | Various causes | –intellectual functioning that is significantly below average
-delays in two or more areas of occupation such as play skills, ADLs, homemaking skills -deficits in intellectual functioning (academics, abstract thinking) and adaptive behaviors |
-varies depending on level of disability
-develop behavior modification plans -develop alternatives for communication in collaboration with SLP -reciprocal play tasks -ADL skills -handwriting skills and modifications -development of performance patterns that include rituals, habits and roles to enhance engagement in meaningful activities with emphasis on occupations |
An au pair who is an occupational therapist works with a family with an 11-year-old boy with intellectual disability. |
| Learning Disability | Various causes, often secondary to other conditions | -difficulties in learning
-may result in language deficits -difficulties in attention and impulse control -visual-spatial organization deficits -memory deficits or difficulties with motor function |
School based OT services that include sensory integration strategies, cognitive-behavioral therapy techniques, handwriting, organization training, motor planning tasks | A specialty elementary school in Atlanta provides services to children with learning disabilities. |
| Rett Syndrome
Neurodevelopmental disorder that affects girls almost exclusively |
Caused by mutation in the MECP2 gene which is needed for brain development | 4 stages to Rett Syndrome.
– Slowed growth. – Loss of normal movement and coordination. May lose ability to perform motor skills previously learned e.g. walking Eventually muscles become weak or may become rigid or spastic with abnormal movement and positioning -Loss of communication abilities. Become disinterested in other people, toys and their surroundings, loss of speech – Abnormal hand movements. repetitive, purposeless hand movements include hand-wringing, squeezing, clapping, tapping or rubbing – Unusual eye movements. eye movements, such as intense staring, blinking, crossed eyes or closing one eye at a time – Breathing problems. breath-holding, hyperventilation, forceful exhalation of air or saliva, and swallowing air. – Irritability and crying – Abnormal behaviors. E.g. sudden, odd facial expressions and long bouts of laughter, hand licking, and grasping of hair or clothing – Cognitive disabilities. Loss of skills can be accompanied by a loss of intellectual functioning – Seizures – Scoliosis — Sleep disturbances |
– Look for potential. E.g. use of eye gaze, or initiation of movement towards a desired object
– Keep in mind the effect of dyspraxia. May be a marked delay between a prompt and reaction – Progress is often very slow. Improvements in functional self-care and hand skills can be achieved throughout the lifespan. – Identify and encourage use of body parts which she may have better control. E.g. head, elbows – Maximize hand use for functional activities |
|
| Spina Bifida | Malformed development of the spinal cord, meninges and brain resulting from abnormal closure of the vertebrae. Non-curable. | -poor prognosis for those with high level spinal cord involvement and congenital anomalies
-visual deficits -four levels of involvement from mild to severe |
-increase basic self-care skills and IADLs with adaptive equipment, assistive devices and wheelchair seating and positioning if required
-bladder and bowel training including self-catheterization -skin integrity education -range of motion, strengthening, gross and fine motor activities within the patient’s level of ability -home accessibility and safety training as applicable -consultation with educators to assist with academic success and school based OT services as indicated |
Professionals at a specialty clinic explain spina bifida and interventions for the condition. |
| Traumatic Brain Injury | Caused by traumatic injury to the skull that impacts the tissues of the brain. | Acute: -loss of consciousness-slow slurred speech -vomiting -irritability -lethargy -confusion -severe headache Long Term: -changes in personality -abnormal muscle tone, may have hemiplegia -changes in affect -memory loss -cognitive deficits -impulsiveness, quick tempered -visual deficits | -schedules to prepare child for the environment
-use textures to improve sensory awareness and muscle tone -develop skills for ADLs and play (visual attention, memory, UE strength) -weight shifting and weight bearing tasks -engage in daily ADL skills and simple IADLs, such as meal prep and clean up |
A 17-year-old boy who has sustained a traumatic brain injury participates in an occupational therapy session. |
| Visual Impairments | Various causes, including abnormal eye development, strabismus, amblyopia (lazy eye), decreased binocular function (eyes not working together), optic nerve hypoplasia, Retinopathy of Prematurity, ocular albinism, central nervous system disorders resulting in cortical vision damage and visual field deficits | -difficulty focusing on faces or toys
-holds objects very close -tilts head to look at objects -crossed eyes -jerky eye movements -decreased school performance -poor gross and fine motor skills |
-varies depending on the severity of eye impairment
-use of contrast -clear and descriptive explanations of environment -sensory integration strategies to address gravitational insecurity, tactile defensiveness, and movement aversions -encourage hand exploration and association of sounds and smells |
A toddler with a visual impairment participates in an occupational therapy session. |
Treatment Approach
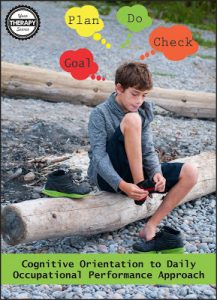
Cognitive Orientation to Occupational Performance (CO-OP)
Cognitive Orientation to Occupational Performance (CO-OP) is a performance-based treatment approach for children and adults who experience difficulties performing the skills they want to, need to or are expected to perform. Focused on enabling success, the CO-OP Approach employs collaborative goal setting, dynamic performance analysis, cognitive strategy use, guided discovery, and enabling principles. It is defined as a “client-centered, performance based, problem solving approach that enables skill acquisition through a process of strategy use and guided discovery”. CO-OP is an evidence-based approach that has been successful for children with developmental coordination disorder (DCD) and autism spectrum disorder (ASD)
The main objectives of CO-OP are:
A. Skill acquisition in child-chosen tasks
B. Development of cognitive strategies
C. Generalization and transfer of learned skills and strategies.
The steps to the CO-OP approach include client chosen goals, dynamic performance analysis, cognitive strategy use, guided discovery, enabling principles, parent/significant other involvement and intervention format.
Generally, the CO-OP approach is GOAL – PLAN – DO – CHECK.
Step 1: The child along with the parents determine a goal or task that needs to be accomplished. The therapist performs evaluations and assessments to determine if the goal is feasible.
Step 2: Create a plan together to reach the goal. To begin, the therapist performs a task analysis of the child performing the skill. The child can explore different strategies such as body position, attention to the current task, modifications, self-talk, self-monitoring, etc.
Step 3: Carry out the plan with the child using the planned strategies to accomplish the task.
Step 4: Check the plan. How well did it all work? What was successful? What can I change? What needs improvement? This can be done through self-interrogation, self-monitoring, self-observation and self-evaluation.