Parkinson’s disease is a progressive disorder of the nervous system.
………. … ..
PD is characterized by dysfunction in both voluntary and involuntary movements. The classic triad of symptoms includes tremor, rigidity, and voluntary movement disorders:
1. Tremor
One of the hallmark symptoms of PD is a resting tremor, often described as a pill-rolling tremor. Resting tremors occur at rest and subsides when voluntary movement is attempted. This type of tremor often typically diminishes with activity, but in some patients the tremor persists during performance of functional activities
2. Rigidity
Rigidity is the stiffness within a muscle that impedes smooth movement. Both cogwheel and lead pipe rigidity are associated with PD.
3. Voluntary movement disorders
The disturbances in voluntary movement are identified as difficulty initiating movement (akinesia) and slowness in maintaining movement (bradykinesia). The bradykinesia and akinesia are often the most disabling motor symptoms for a patient with PD. The delay in initiating movement patterns and the slowness in executing the motion compromise functional tasks such as driving, dressing, and eating. Another factor affecting ADL performance is hand dysfunction which is a common symptom in Parkinson’s disease and is characterized by poor manual dexterity, deficits in fine motor movements, and difficulty in performing movements with normal amplitude, speed, and coordination. Hand dysfunction leads to difficulties in activities of daily living (ADL), such as eating, dressing, washing, and writing.
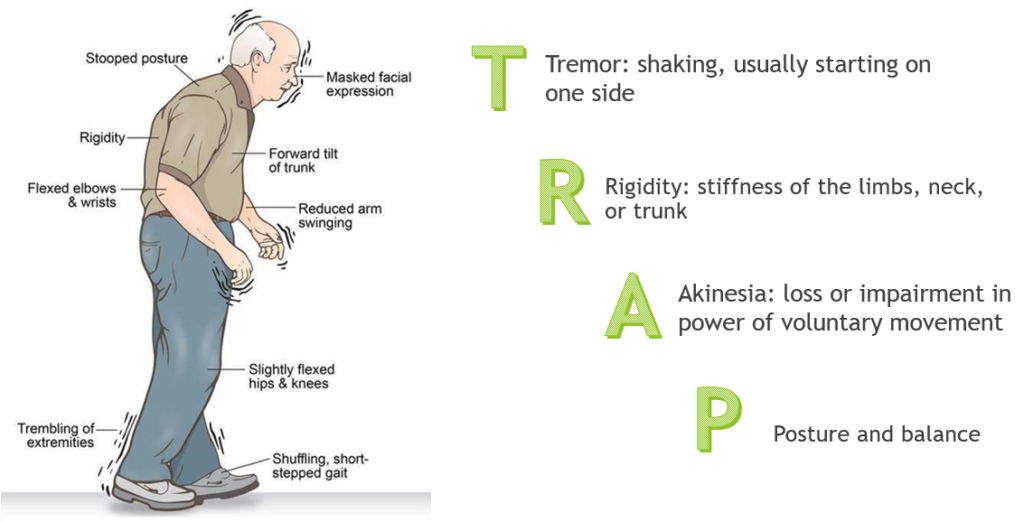
The common features of Parkinson’s Disease are easily remembered by the mnemonics TRAP and SMART.
T – Tremor, specifically resting tremor.
R – Rigidity. Difficulty moving and stiff arms and limbs.
A – Akinesia. No or slow movements.
P – Postural instability. Posture problems.
S – Shuffling-Gait
M – Mask-like Face
A – Akinesia
R – Rigidity
T – Tremor
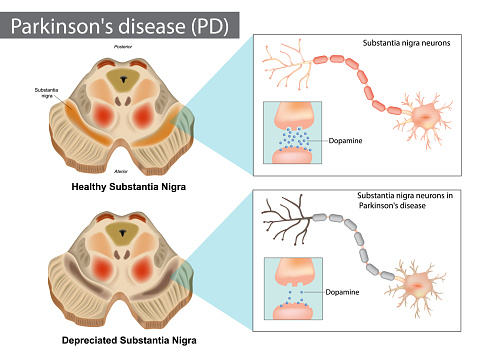
The table below outlines the cause and symptoms of this disease, as well as examples of occupational therapy evaluation, treatment, and adaptations.
| Cause | Symptoms | Evaluation | Treatment | Adaptations | Environmental Modifications |
| Neurons in the brain that produce dopamine break down and die. The decreased dopamine in the brain leads to abnormal brain activity and symptoms of Parkinson’s Disease.
Some gene markers have been found that indicate an increased risk for the disease. In rare cases specific genetic mutations lead to multiple family members developing Parkinson’s Disease. Environmental risk factors and some toxins slightly increase the risk of Parkinson’s Disease. |
Tremor – Shaking, usually in the limbs -Pill rolling tremor, the thumb and first finger rub back and forth against each other -Resting tremor, the limbs shake when a person is at rest, especially the arms and hands -Intention tremor, an increase in the severity of tremor before a person moves a limb .. Bradykinesia – Slow movement -Short steps when walking -Dragging feet when walking -Difficulty changing positions .. Muscle Rigidity – the muscles become stiff, making it difficult to move. . Stooped Posture – posture becomes flexed, or stooped, and balance may become impaired ….. Postural Instability ….. Gait disorders –shuffling gait –freezing .. Loss of automatic movements -blinking -smiling -swinging arms while walking .. Speech Problems -soft voice -slurred speech or quick speech -voice may become monotone .. Changes in writing – writing may become smaller or shaky in appearanceMask-like facial expression Cognitive symptoms Oral-motor |
• Range of motion measurements • Manual muscle test, grip and pinch strength measurement • Fine motor skills evaluation – 9 hole peg test or other fine motor evaluation • Cognitive evaluation – Allen Cognitive Levels Test, Mini-Mental State Exam or other questionnaire • Visual Perception – Motor-Free Visual Perception Test • Activities of Daily Living (ADL)and Instrumental Activities of Daily Living (IADL) Questionnaire • Observation of ADL and IADL skills |
Range of motion and strengthening exercises -grade from assisted to independent -use extra repetitions to minimize intention tremor .. Fine motor coordination activities -grade from assisted to independent -avoid timed tasks to reduce stress and intention tremor .. Focused attention activities -visualize the fine motor activity prior to completing -focus on a single aspect of the task to improve that particular movement .. Patient education -energy conservation -work simplification -use of adaptive equipment .. Caregiver education -use of rhythmic cues -use of adaptive equipment -need for environmental adaptations |
** It is important to consider the amount of energy and time needed to perform a specific task. As the disease progresses, poor endurance, and fatigue impact on the patient’s participation in their ADLs. – The use of built-up handles for eating and writing utensils should be introduced during the initial stages of PD as a lightweight utensil may facilitate smoother and higher-velocity arm movement. – When muscle weakness is not a major deficit for the individual with incoordination, the use of weighted devices can help with stabilization of objects. For example: To prevent spills during the plate-to-mouth excursion weighted utensils to offer stability. .Adaptations to reduce tremor -active assistive exercise, such as performing range of motion exercises by sliding arms on a table top -wrist or hand weights during writing or other fine motor activities -weighted eating and grooming utensils -weighted pen or pencilAdaptations for mobility -wheeled walker . Adaptations for upper extremity mobility and strength -reacher -long handled sponge for bathing -adapted clothing fasteners or pull on clothing -slip on or Velcro closure shoes -non-skid mats -jar opener -large handled cooking utensils -wheeled cart to transport items -walker basketUse of rhythmic cues -help to pattern activities to reduce hesitation and intention tremor -cues may be auditory, visual, or tactile |
• Home entrance ramps Widen entrance and interior doors -32 inch minimum width to accommodate a wheelchair -36 inch minimum width to turn a wheelchair • Remove area and throw rugs. • Raised toilet or removable raised toilet seat • Bath bench and hand held shower • Wall mounted grab bars near toilet and bathtub or shower • Organize kitchen cupboards so most frequently used items are on the lower shelves of upper cupboards, upper shelves of lower cupboards • Place a board or firm support under sagging cushions of chairs or couches • Raise low chairs or couches up on risers to assist with moving from sitting to standing • Power lift chair • Power stair lift |
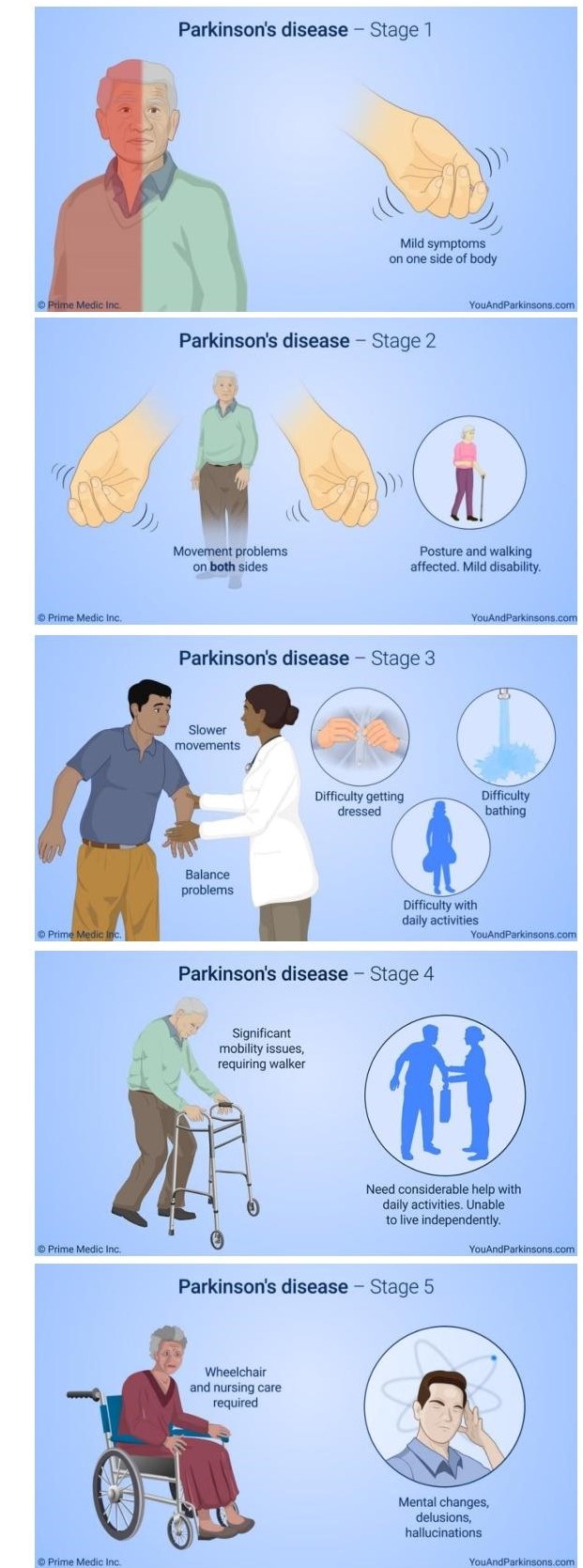
Stages of Parkinson’s Disease
Stage 1
Unilateral involvement. Mild symptoms. Minimal functional impairment. Slight changes in walking, posture, facial expressions.
Stage 2
Early stage. Bilateral involvement. Loss of facial expression, soft voice, monotone voice, fading volume after starting to speak loudly, slurring speech, tremors, stiffness/rigidity of the muscles in the trunk that may result in neck or back pain, stooped posture, and general slowness in all activities of daily living.
Stage 3
Mid-stage. Motor symptoms become worse. Loss of balance and slowness of movement. Balance compromised significantly not able to make the rapid, automatic, and involuntary adjustments necessary to prevent falls.
Stage 4
Progressed to a severely disabling disease. Symptoms severe and limiting. Movement greatly impaired. May still be able to walk and stand unassisted ,but visibly incapacitated. May seek assistance of a walker. Independent living is impossible, and assistance needed with ADLs. The necessity for help is the important feature of this stage.
Stage 5
Most advanced and debilitating stage. Characterized by an inability to rise from a chair or get out of bed without assistance. May freeze or stumble when walking.
Experience difficulty in walking and standing. Stiffness in legs may make it impossible to stand or walk. Requires wheelchair or may be bedridden. Round-the-clock care is needed at this stage to prevent falls and assist with ADLs. Hallucinations and delusions may also occur at this stage.
| STAGES | SYMPTOMS
|
OT INTERVENTION |
| 1 | Unilateral tremor, Micrographia, poor endurance for previous occupations, fatigue | Work evaluation if the patient is employed; work simplification for work and home settings; develop the habit of taking frequent rest breaks; use of utensils with enlarged handles |
| 2 | Bilateral motor disturbances, mild rigidity reported, difficulties with simultaneous tasks, difficulties with executive function | Energy conservation techniques related to ADLs; develop daily flexibility exercises focused on trunk rotation; driving assessment and alternatives for community mobility; use of task analysis to structure sequential tasks |
| 3 | Balance problems with delayed reactions, difficulties in skilled sequential tasks | Environmental modifications in the home, including raised toilet seats, chairs with armrests, removal of throw rugs; use of visual cues and supports for sequential tasks |
| 4 | Fine motor control severely compromised, oral motor deficits | Modifications to support participation in self-care tasks, changes in food textures |
| 5 | Patient severely compromised motorically, dependent with ADLs | Use of environmental controls to allow access to the environment |
Table copied from: Pedretti’s Occupational Therapy – E-Book (Occupational Therapy Skills for Physical Dysfunction)
Latest Trends in Managing PD
The Lee Silverman Voice Treatment (LSVT) – LSVT BIG®
LSVT BIG® is an exercise and self-cueing treatment derived from the LSVT LOUD®
Recent advances in neuroscience have suggested that exercise-based behavioral treatments may improve function and possibly slow progression of motor symptoms in individuals with Parkinson disease. LSVT programs are evidence-based treatment protocols designed specifically to address the motor, sensory and non-motor symptoms that many people with PD face.
The unique aspects of the LSVT Programs include the combination of:
(a) An exclusive target on increasing amplitude (loudness in the speech motor system, bigger movements in the limb motor system)
(b) A focus on sensory recalibration to help patients recognize that movements with increased amplitude are within normal limits, even if they feel “too loud” or “too big”
(c) Training self-cueing and attention to action to facilitate long-term maintenance of treatment outcomes.
In addition, the intensive mode of delivery is consistent with principles that drive activity-dependent neuroplasticity and motor learning.
There are 2 distinct LSVT therapy programs:
• LSVT LOUD® – improves communication
• LSVT BIG® – improves mobility and movement used in everyday function.
LSVT LOUD® and LSVT BIG® treatments can only be given by specially trained LSVT Certified Clinicians. With their guidance, people with PD learn to translate skills built during treatment into better everyday communication, function and movement.
Research on LSVT LOUD® has documented that people with PD show improvements in loudness and intonation of their speech, as well as clarity of speech and facial expressions. Although research on LSVT BIG® has not been as extensive, results have shown that there is improved walking, balance, and bed mobility. Since LSVT BIG® treatment is customized to each person’s specific needs and goals, it can help regardless of the stage or severity of the person’s PD. Treatment is ,however, most effective in the early or middle stages of PD.
LSVT BIG®
While people with PD perceive their movement as being normal, they often present with abnormally small amplitude movement.
LSVT BIG® is designed to decrease the impact of hypokinesia on the functional mobility of people with PD by encouraging patients to move using powerful, large amplitude movements during progressive, high intensity training. The goal of LSVT BIG® is to restore normal movement amplitude by recalibrating the patient’s perception of movement execution. One unique aspect of LSVT BIG®’s treatment protocol is its emphasis on key principles associated with motor learning, including high intensity, multiple repetitions, and progressive complexity. These principles may help to facilitate activity dependent motor learning and neuroplasticity to enhance the generalizability and automaticity of movement. This emphasis maximizes an individual’s ability to develop, consolidate, and generalize self-cueing skills to the point that they transfer into more effective real-world function
Lysergic acid diethylamide (LSD) as a complementary treatment for Parkinson’s Disease
Parkinson’s disease is a neurodegenerative disorder of unknown cause. Age is the most consistent risk factor. Classically Parkinson’s disease presents with resting tremor, rigidity, and akinesia often in an asymmetric fashion, but later usually bilateral. Clinical features are variable with some patients presenting with akinesia and rigidity only, and others with a tremor dominant type.
The aim of medical treatment is the restoration of abnormal neurotransmitter function in the basal ganglia.
L-dopa combined with a peripheral decarboxylase inhibitor remains the single most effective drug to improve parkinsonian symptoms, but the biggest problem with this is that while it produces excellent results in the early stages of Parkinson’s Disease, long-term use of the drug can result in dyskinesias, dystonias, possible toxicity, loss of effectiveness, cognitive impairment, and even psychosis.
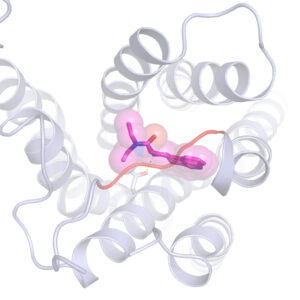
LSD is a member of a class of drugs called ergolines, which can be used to treat many conditions, including migraine headaches and Parkinson’s disease.
LSD targets the 5-HT2A serotonin receptors which can enhance the biosynthesis of dopamine. There are strong links between the serotonin and dopamine systems, both structurally and in function. Serotonin and dopamine interact with and affect each other to maintain a careful chemical balance within the body. Researchers have found that LSD binds to the 5-HT2A receptor in a way that the serotonin receptor closes a “lid” over the LSD molecule, preventing it from quickly detaching. This likely explains the drug’s long-lasting effects.
Recently there has been increased interest in microdosing LSD- using doses of LSD that are not psychoactive (typically 10 micrograms). A standard recommendation is micro-dosing every three days.
The mechanism of psychoactive drug action, including how certain drugs activate one signaling pathway inside cells, while avoiding another can help in the design of new drugs with desired signaling properties and fewer undesired side-effects.
References:
https://pmj.bmj.com/content/76/900/602
http://www.chm.bris.ac.uk/motm/serotonin/LSD.HTM
https://www.drugtimes.org/hallucinogens-culture/lsd-and-parkinsons-disease.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4813425/