Neurological Treatment Approaches
The charts below review the traditional neurological treatment approaches of:
1. Neurodevelopmental Treatment (NDT)
2. Proprioceptive Neuromuscular Facilitation (PNF)
3. Brunnstrom approach
4. Rood approach
5. Constraint-Induced Movement Therapy (CIMT) which is a new treatment technique is also reviewed.
Neurodevelopmental Treatment Approach (NDT)
– developed by Berta Bobath PT, and Karel Bobath, M.D.
Basis – The sensations of movement are learned, rather than the actual movements. Abnormal movement patterns must be stopped so that the person can gain control over movement in a developmental sequence. Basic patterns of posture and movement, righting reactions, and equilibrium responses can be facilitated by providing appropriate stimuli while abnormal movement patterns are inhibited.
-Early intervention is necessary to avoid abnormal patterns and/or contractures.
-Once the person has gained control of basic movement patterns, he will automatically be able to expand upon these patterns to learn more skilled movements.
.. … 
| Treatment Technique | Treatment Technique | Example | Picture/Video |
| Reflex-Inhibiting Patterns | Patterns of movement that inhibit abnormal muscle tone or reflexes. -initiated at key points on the body to inhibit the abnormal muscle pattern of the more distal body part. -controls muscle tone distribution -pattern is applied to the proximal end of the body part to allow voluntary movement in the distal part. |
An occupational therapist working with a child with spastic quadriplegic cerebral palsy lifts the child’s head into slight hyperextension of the neck to inhibit the flexor tone in the child’s shoulders and trunk so that the child can reach up. | |
| Handling | The technique used to move a patient through reflex-inhibiting patterns and facilitation of righting and equilibrium reactions. -used to influence postural tone and inhibit abnormal patterns. -regulates coordination of agonists, antagonists, and synergists. -facilitates normal automatic responses -completed passively at first and then gradually withdrawn as the patient gains the ability to move in normal patterns. -constantly changes to inhibit undesired responses and facilitate desired responses during activity. |
While working with a woman with right upper extremity flexor tone following a stroke, an occupational therapist repeatedly positions the woman’s shoulder girdle in retraction so that the woman can pull her arm away from her body and straighten her elbow. | |
| Righting Reactions | Reactions that are evoked through a sequence of postures to help the patient change position. -Neck righting and body righting reactions are used to move the patient from supine, to prone, to on-elbows, to quadruped, to tall kneeling, to standing. -Labyrinthine righting reactions are used to help the patient regain normal position in space after being displaced. -The head is used as a key handling point for neck and body righting reactions. The shoulders are used as key class=”blur” handling points for labyrinthine righting reactions. |
An occupational therapist positions a child with cerebral palsy in side lying on one elbow to facilitate labyrinthine righting reaction of the head so that the child can look at and reach for a toy. | |
| Equilibrium Reactions | Reactions are evoked by displacing the patient’s center of gravity while that patient is in a developmental pattern. -does not begin until the patient can maintain the pattern against gravity. -can be elicited by either moving the patient or moving the surface that the patient is on. -the patient is moved in all directions within each developmental pattern – back and forth, side to side, and obliquely. -as the patient improves moving surfaces can be used to elicit reactions. -handling is completed by the therapist at the shoulders or hips, leaving the head and extremities free to react to the position. |
While working with a child with hemiplegia resulting from a seizure disorder, an occupational therapist holds the child on a therapy ball and handles his hip and pelvic region to facilitate upper body equilibrium responses as she moves the child through all the planes of movement on the ball. | |
| Sensory Stimulation | Sensory stimulation techniques are used to facilitate muscle activity when hypotonic muscles are observed. -always done when the patient is in a reflex-inhibiting pattern. -stopped if the response is abnormal or results in hyperactive tone. -three types of sensory stimulation 1. Weight bearing – pressure and resistance are used to increase muscle tone and decrease involuntary movements. 2. Placing and Holding – the patient’s limb is moved to various positions with assistance from the therapist, and then the patient is instructed to hold each position. 3. Tapping – manual muscle facilitation through one of four techniques: a. joint compression to increase tone and maintain posture b. inhibitory tapping by releasing the body part and catching it after a very short fall to stimulate stretch reflexes c. alternate tapping by very lightly pushing the patient to and from mid position d. sweep tapping where the therapist sweeps a hand over the desired muscles in the desired direction of movement to activate synergic patterns |
While working with a man who has flexor muscle tone in his left arm following a stroke, an occupational therapist positions the man’s arm, performs joint compressions to his shoulder and elbow, then has him place his hand on the mat and lean on it with his elbow straight. |
Proprioceptive Neuromuscular Facilitation (PNF)
– developed by Herman Kabat, Ph.D., M.D.
Basis – Neuromuscular movement is facilitated by stimulating the proprioceptors using assorted techniques superimposed on patterns of movement and posture. There are 11 developmental principles associated with PNF.
.. 
Principles of PNF
1. All human beings have potentials that are not fully developed.
-abilities become the means for reducing inabilities
2. Normal motor development proceeds in a cervico-caudal to proximodistal direction.
-head to foot
-trunk to extremities
3. Early motor behavior is dominated by reflex activity. Mature motor behavior is reinforced or supported by postural reflex mechanisms.
-reflexes do not disappear, but instead become integrated into the nervous system
4. The growth of motor behavior has cyclic trends as evidenced by shifts between flexor and extensor dominance.
-interaction between the movements of flexion and extension is necessary to develop function
5. Goal-directed activity is made up of reversing movements.
-movement is rhythmic and reversing throughout life
-if a person cannot reverse direction, function will be limited
6. Normal movement and posture are dependent upon “synergism” and a balanced interaction of antagonists.
-the goal of the PNF approach is to achieve a balance of antagonists
-without balance, quality of movement decreases
7. Developing motor behavior is expressed in an orderly sequence of total patterns of movement and posture.
-functional activity is based on total movement patterns
-direction of movement also develops in an orderly sequence
8. Normal motor development has an orderly sequence but lacks a step by step quality. Overlapping occurs.
-the order of the developmental sequence helps the therapist to find a place to begin treatment.
9. Improvement of motor ability is dependent upon motor learning.
-proprioceptive feedback plays a role in conditioned responses
-sensory cues enhance motor learning
10. Frequency of stimulation and repetition of activity are used to promote and for retention of motor learning and for the development of strength and endurance.
-repetition occurs naturally during activity
11. Goal-directed activities, coupled with techniques of facilitation, are used to hasten learning of total patterns of walking and of self care skills.
-facilitation techniques and activity together enhance neurological integration. One or the other is not enough.
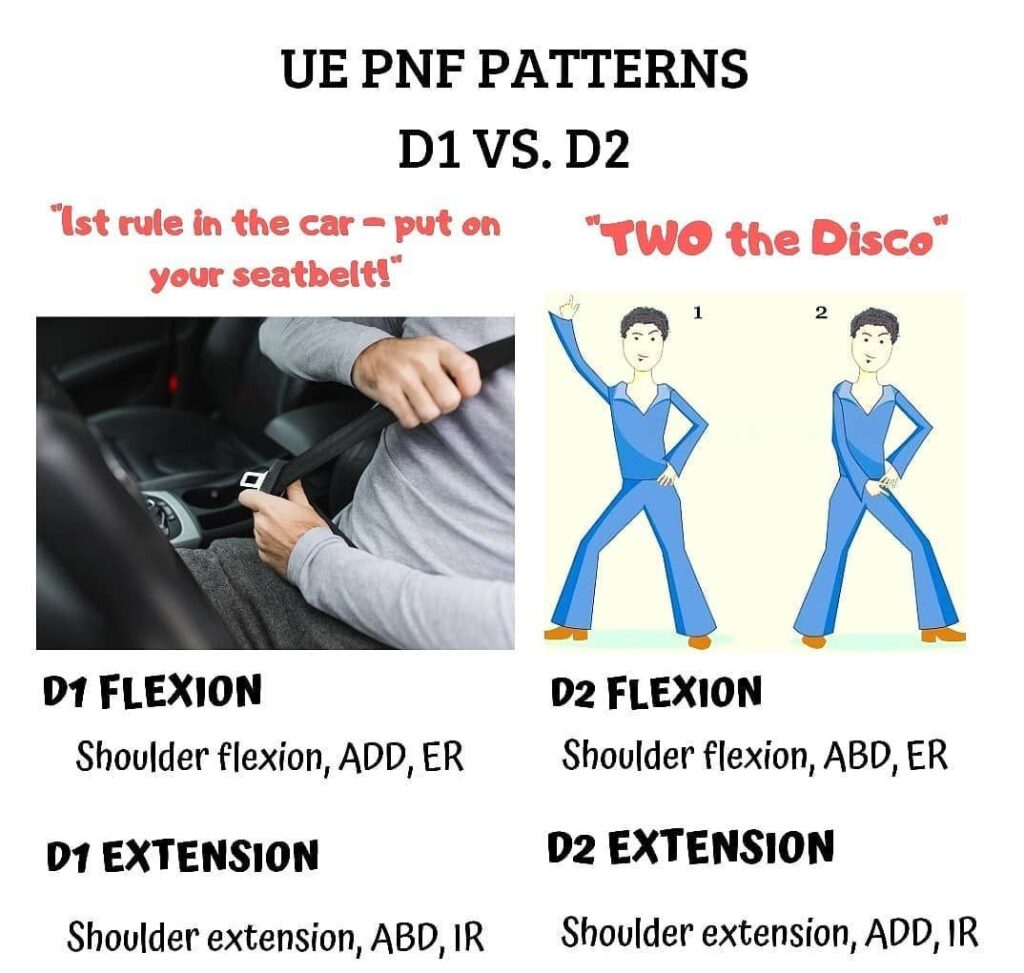
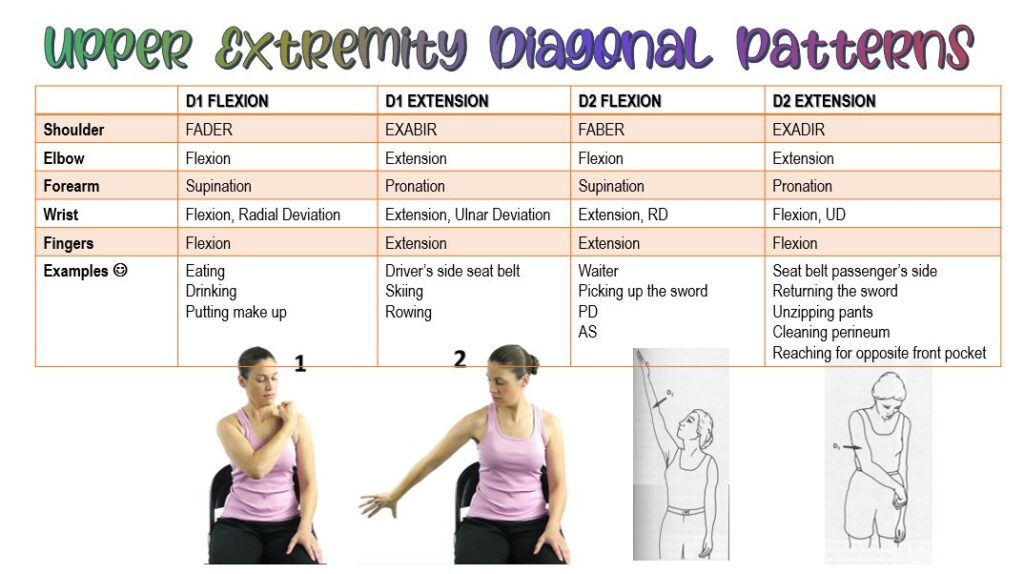
PNF Diagonal Patterns
Two pairs of diagonal patterns exist for every major part of the body. Each pattern consists of three movement components, which include flexion or extension, internal or external rotation, and abduction or adduction.
| Pattern | Description | Description | Photo or Video |
| D1 Flexion | -shoulder flexes, adducts and externally rotates -elbow flexes/extends -forearm supinates -wrist flexes toward radial side -fingers flex and adduct -thumb flexes and adducts |
An occupational therapist facilitates D1 flexion while assisting a man recovering from a stroke to wash the opposite side of his face with his affected hand. | |
| D1 Extension | -shoulder extends, abducts and internally rotates -elbow extends -forearm pronates -wrist extends toward ulnar side -fingers extend and abduct -thumb extends and abducts |
An occupational therapist facilitates D1 extension while working with a woman who has multiple sclerosis to pick up a napkin and throw it in the garbage can. | |
| D2 Flexion | -shoulder flexes, abducts and externally rotates -elbow extends -forearm supinates -wrist extends -fingers extend and abduct -thumb extends and adducts |
An occupational therapist facilitates D2 flexion while working with a man who has muscular dystrophy to reach up and grasp a pulley on a weight machine. | |
| D2 Extension | -shoulder extends, adducts and internally rotates -elbow flexes -forearm pronates -wrist flexes toward ulnar side -fingers flex and adduct -thumb opposes |
An occupational therapist facilitates D2 extension while working with a woman who has had a stroke to grasp and fasten her seat belt in the car. |
Variations of Movement Patterns
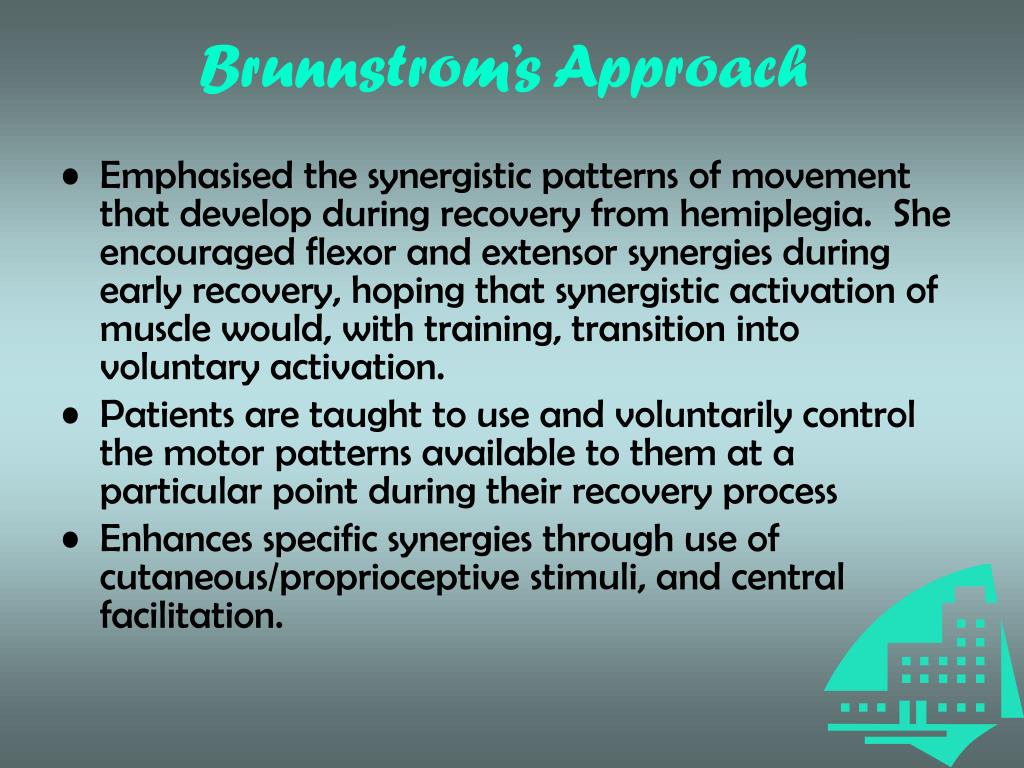
Brunnstrom Movement Therapy Approach
– developed by Signe Brunnstrom, PT
Basis – <style=”background-color: yellow; color: #000000;”>Synergies and reflexes that are a normal part of early development should be included as a part of the sequence of return of motor function in hemiplegia.
.. 
Reflexes and Reactions
Stages of Recovery, Upper Extremity
| Stage | Stage | Example | Photo or Video |
| 1 | Flaccidity – no voluntary movement. | An occupational therapist provides passive range of motion to the hemiplegic upper extremity of a man who suffered a stroke. | |
| 2 | Synergies developing -flexion usually develops before extension -weak associated reactions may appear -spasticity may develop |
An occupational therapist asks the same man to hold his unaffected arm at 90 degrees of flexion. She then tells the man to hold the position while she pushes down on the arm. She is able to observe increased muscle tone and slight shoulder flexion in the affected arm. | Slide presentation by a physical therapist about the Brunnstrom Movement Therapy approach. Slides 33 and 34 discuss the stages of recovery. |
| 3 | Synergies performed voluntarily -spasticity may become severe |
An occupational therapist has the man lean forward from his chair and push on a bolster with his unaffected arm. The therapist helps the man position his affected arm and taps on the triceps of the affected arm to facilitate elbow extension. | Slide presentation on Brunnstrom’s Stages of Recovery as applied to the hand. |
| 4 | Some movements observed that deviate from synergy -hand behind body -arm forward in horizontal position -pronation/supination with elbow flexed to 90 degrees -spasticity begins to decrease |
An occupational therapist has the man perform active assistive shoulder flexion on a table top with both hands on a towel to facilitate movement. | |
| 5 | Independence from basic synergies -arm to side in horizontal position -arm forward and overhead -pronation/supination with elbow fully extended -spasticity almost gone |
An occupational therapist has the man reach for cones with his affected arm to strengthen shoulder flexion. | |
| 6 | Isolated joint movements are performed/ voluntarily with close to normal coordination -no spasticity present |
An occupational therapist has the man use his affected arm to take his jacket off of a hook. | |
| 7 | Normal movement restored | The man is discharged from occupational therapy because he has regained normal movement. |
Rood Approach
– developed by Margaret Rood, MA, OT
Basis – Motor patterns develop from basic reflex patterns present at birth which are gradually modified through sensory stimuli until mature control is achieved on a conscious, cortical level.
……. 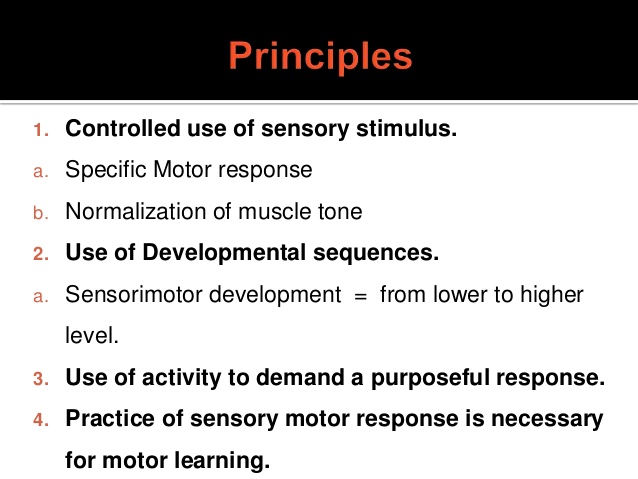
Four components of the Rood Approach
1. Normalization of tone and facilitation of desired muscle responses is acquired through the use of appropriate sensory stimuli.
2. Sensorimotor control is developmentally based and must occur sequentially.
3. Movement is purposeful. Activities are used to create a purposeful response in the patient and elicit the correct movement pattern.
4. Repetition is necessary to establish sensorimotor responses.
Sensory Stimulation and Inhibition Techniques
| Technique | Description | Example | Photo or Video |
| Stretch | Stretching of the muscle, applied in three ways: 1. Quick stretch – results in a short lived muscle response with contraction of the agonist muscle and inhibition of the antagonist muscle 2. Prolonged stretch – inhibits muscle responses to reduce tone 3. Maintained stretch – uses resistance to facilitate muscle contraction |
An occupational therapist working with a woman with hemiplegia resulting from a stroke applies a quick stretch technique to the woman’s biceps and forearm muscles to facilitate elbow flexion. | An occupational therapy instructor demonstrates quick stretch with a student. |
| Vibration | Applied to the muscle in two ways -high frequency at 100-200 Hz to facilitate muscle contraction -low frequency at 5-50 Hz to inhibit muscle contraction |
While working with a man with hemiplegia resulting from a traumatic brain injury, an occupational therapist applies vibration at a fast speed to the man’s middle trapezius to facilitate shoulder retraction. | |
| Joint Approximation and Joint Compression | The joint to be moved is compressed either by quick, jerking motions or by slow, sustained compression. -quick compression facilitates movement -sustained compression inhibits movement |
An occupational therapist applies quick joint compression techniques to the elbow of a woman with hemiplegia following a stroke, then asks the woman to straighten her arm and bear weight on the arm while reaching for cones with the unaffected arm. | Occupational therapy students demonstrate joint compression techniques in the first part of this video. |
| Touch | Facilitates muscle activity by eliciting protective responses -brief light touch -brief swiping motion with ice -noxious stimuli -light pinching |
While working with a child with hypotonic cerebral palsy, an occupational therapist lightly “tickles” the child’s forearm to facilitate wrist extension prior to a prone over a ball activity. | A demonstration of three faciliatory and three inhibitory techniques. |
| Brushing | Application of light stimuli using a manual or battery operated brush to elicit muscle reaction. | An occupational therapist uses an electric brush to stimulate the triceps of a man with hemiplegia following a stroke to facilitate elbow extension prior to putting on a shirt. | Occupational therapy students demonstrate fast brushing. |
| Prolonged Icing | Ice applied using chips, wraps, packs or an ice bath to inhibit muscle activity. | An occupational therapist applies a cold pack to the forearm of a woman with muscle spasticity resulting from multiple sclerosis to reduce finger flexor tone. | |
| Neutral Warmth | Prolonged application of lukewarm heat to inhibit muscle activity. -wrapping in towel or blanket -hot pack -tepid water bath -air splint |
An occupational therapist applies air splints to the forearm and hand of a woman with hemiplegia resulting from a stroke prior to completing range of motion exercises. | |
| Maintained Touch | Firm manual contact at the midline abdomen and back to provide a general calming response. | An occupational therapist working with a child with hemiplegia resulting from a seizure disorder applies firm pressure to the child’s abdomen and back to calm the child’s muscle activity prior to a sitting balance activity. | |
| Slow Stroking | Stroking using a flat hand over the paravertebral muscles from cervical region to sacral region to elicit a general calming response. | An occupational therapist provides slow stroking to a child with spastic quadriplegic cerebral palsy while the child is prone on a therapy ball to calm the child’s muscle tone prior to a reaching activity. | Students demonstrate several facilitation and inhibition techniques, including neutral warmth and slow stroking. |
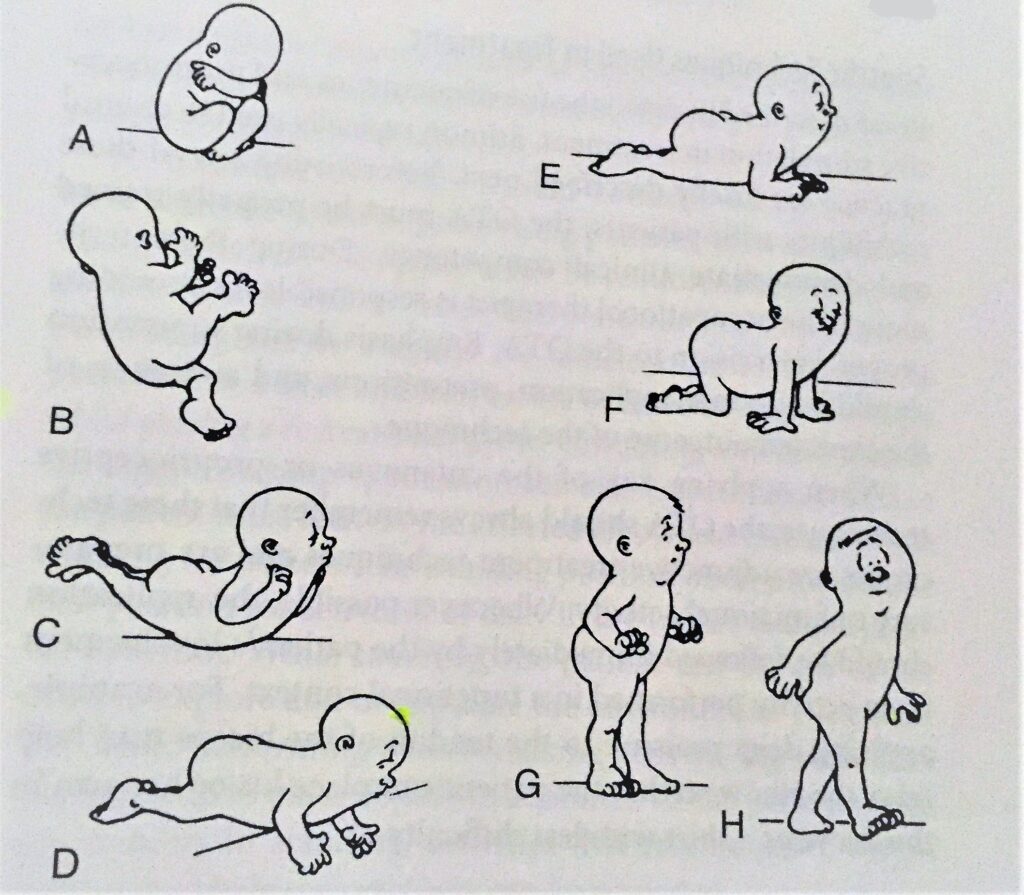
Ontogenic Motor Patterns
| Pattern | Description | Method to Elicit | Treatment Examples | Photo or Video |
| 1. Supine withdrawal | The body is in total flexion while in supine (curled in a ball). Upper extremities cross the chest, dorsum of extended hands touch the face, lower extremities flex and abduct. | Fast brushing of the lower back and dermatomes of C1-4 posterior primary rami distribution. Small wedges may also be placed under the head and the pelvis to stretch the short extensors of the back to facilitate flexors. | An occupational therapist has a child with cerebral palsy push his hands together to squeeze theraputty with shoulders adducted. | A slide presentation by a physical therapist on the Rood Approach. Slide 19 shows the ontogenic motor patterns. |
| 2. Rolling over | The arm and leg on the same side flex as the patient rolls. | Give the patient something interesting to look at, causing the patient to turn his head. The body will follow the head. | An occupational therapist shows a child with hemiplegia resulting from a seizure disorder a toy car, then moves the car to the side of the child’s head. The child turns his head and then rolls his body. | A cute picture study video of the ontogenic motor patterns. |
| 3. Pivot prone (prone extension) | In prone, the neck, trunk, shoulders, hips and knees are extended, the shoulders are abducted and externally rotated, and the elbows are flexed. -the first postural stability pattern. -all other postural patterns are based on this one. |
With the patient in prone, the area over the deep back extensors is fast brushed (C-brushed); the skin over the posterior deltoid, latissimus dorsi, trapezius, proximal hamstrings, and gluteus are fast brushed (C-brushed) and iced. An activity may be used to demand and resist the response. | An occupational therapist has a child with cerebral palsy lay prone on a scooter board. She applies brushing to the appropriate muscles, and then has the child push himself on the scooter board. | An infant displays rolling, pivot prone, and prone on elbows while maneuvering to retrieve a book. |
| 4. Neck co-contraction | In prone, the patient lifts his head against gravity. -this pattern is used to develop head control. |
The short neck flexors are activated by fast brushing (C-brushing) the flexor distribution of C2; the sternocleidomastoid muscles are activated; the patient is placed in prone and asked to raise his head. -to activate, the muscles are fast brushed (C-brushed) about 20 minutes prior to activity, then the muscles are squeezed while the patient is performing the motor pattern. |
An occupational therapist working with a child with low muscle tone applies fast brushing to the child’s neck flexor muscles, has the child perform an unrelated activity, then has the child lay in prone and pick up and place pom- pom balls by sucking through a straw. | Occupational therapy students demonstrate the ontogenic motor patterns. |
| 5. Prone on elbows | From pivot prone, the shoulders are brought into forward flexion so that the patient can bear weight on his elbows. -position inhibits STNR |
The back and neck extensors are fast brushed (C-brushed); the glenohumeral extensors and abductors are fast brushed (C-brushed) and iced. | An occupational therapist working with a woman who has hemiplegia resulting from a stroke has the woman lay in pivot prone, applies brushing and icing, then helps the woman move to prone on elbows to complete a painting task. | A man moves from a modified pivot prone to prone on elbows. |
| 6. All-fours (quadruped) | The patient supports himself on hands and knees. -does not happen until the neck and upper extremities have developed stability -static at first, then one or two points of support may be lifted, then weight shifting. |
The back and neck extensors are fast brushed (C-brushed); the glenohumeral and hip extensors and abductors are fast brushed (C-brushed) and iced. The patient is placed in pivot prone position and then resistance is added as the patient moves to all fours position. | An occupational therapist working with a man who has hemiplegia due to a seizure disorder completes fast brushing and icing to the appropriate muscle groups, then puts downward pressure on the man’s mid back and pelvis as he moves to all fours to play a bean bag toss game. | A child with cerebral palsy works with therapists to maintain all fours position. |
| 7. Standing | The patient stands upright, first in static position, then unilateral posture, then weight shifting. | NA | An occupational therapist has a woman who has muscle weakness resulting from multiple sclerosis stand to put dishes away in a cupboard. | Occupational therapy students demonstrate ontogenic movement patterns. Functional activity in standing is demonstrated at the end. |
| 8. Walking | The patient begins in standing, then with the foot pushes off, swings through and strikes the heel. -the skill level of standing. |
NA | An occupational therapist has a man who has hemiplegia resulting from a traumatic brain injury walk to retrieve cones placed at waist level around the therapy room. |
Constraint-Induced Movement Therapy (CIMT)
– developed by Edward Taub, Ph.D.
Constraint induced movement therapy (CIMT), or forced use, is a therapeutic strategy designed to promote functional use of a hemiparetic upper extremity. It is a behavioral and task-oriented approach to neurorehabilitation to improve functional use and control of an affected upper extremity.
.. 
Hypothesis: Patients who present with an insult to their CNS, develop “learned non-use” of their affected upper extremity basically because it’s easier to use their unaffected, more functional upper-limb. To prevent this pattern from developing, CIMT aims to use the brain’s neuroplasticity and ability to reorganize itself, to promote habitual use of the affected upper limb. This is achieved by engaging the patient in intense and repetitive functional activities.
CIMT is typically performed with individuals following a CVA as the majority of CVA survivors will experience some functional loss in their impaired limb. It can also be used with individuals who have CP (hemiplegia), TBI and MS.
Minimum inclusion criteria for CIMT:x
• 20º wrist extension
• Up to 10º thumb abduction
• Up to 10º finger extension in any two digits
Also, in order for CIMT to be more beneficial, it is suggested that the patient has:
• Limited spasticity
• Ability to move the affected arm 45º of shoulder flexion and abduction, and 90º of elbow flexion and extension
• Adequate balance
• Minimal cognitive dysfunction
Models of CIMT
1. Unmodified CIMT: The original CIMT involves the restraint of the individual’s unaffected upper extremity with the use of a safety mitt. The mitt is left on for 90% of the day, over a 2-week intervention period in conjunction with 6 hours a day, 5 days of the week of task-specific training. Only activities involving toileting, hygiene and bathing are permitted.
2. Modified CIMT (mCIT):This is a more pragmatic model that was developed to promote better compliance. mCIMT protocols include less clinical treatment time with OT practitioners, providing the patient with an increased amount of time to be spent on home-based practice using the affected upper extremity functionally and during activities of daily living. The program typically consists of 3 hours per day for 5 days/week, for a minimum of 4 successive weeks. In total there will be 20 treatment sessions totaling to 60 hours. The individual is expected to use their affected extremity for a minimum of five hours at home during each week day. There are many different formats of the mCIMT, differing in practice and constraint time, however, all protocols share the same components which stem from the original CMIT.
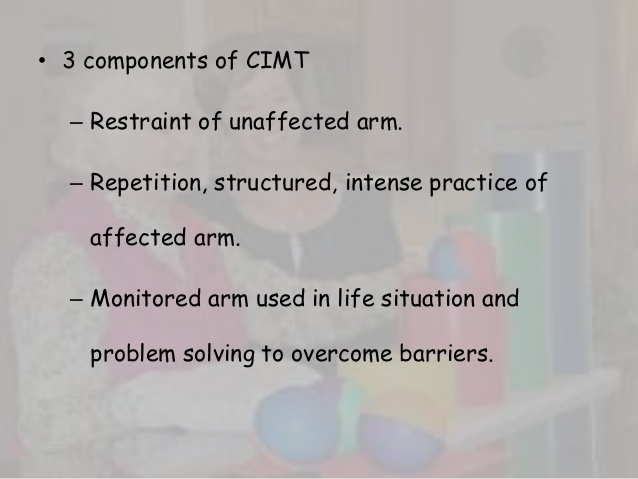
The three fundamental components of treatment intervention, which stem from the original CIMT.
I. Restraint of the unaffected upper limb.
II. Repetitive Functional Task Practice– Structured, intense practice using the affected upper limb.
III. Application of behavioral techniques– To ensure carry over from sessions, the clinician monitors functional use of the affected upper limb in daily life and problem solves to overcome any barriers. It includes a behavioral contract that identifies tasks that the participant will attempt to perform.
The restraints commonly used for CIMT includes:
• Sling
• Plaster cast
• Triangular bandage
• Splint
• Sling combined with a resting hand splint
• Half glove
• Mitt

Key Strategies used during CIMT
Feedback:
An important component of interventions designed to enhance motor learning is the feedback the person receives while attempting a movement strategy and from the results of the movement action. Feedback refers to the sensory experiences intrinsic to the person and the external information provided by the environment, which includes verbal comments from the OT practitioner- feedback during the performance of the motor tasks and on completion of the motor tasks. These strategies are combined with shaping to foster a higher frequency of successful motor practice for functional tasks.
Shaping is considered the most important technique used in CIMT:
Shaping is a training method in which a motor task is gradually graded. Shaping programs are individualized, consisting of 10-15 tasks selected primarily from a basic battery of tasks. Shaping involves providing encouraging feedback immediately after any gain in function. The feedback is explicit to identify small improvements in motor or functional performance.
Shaping tasks are determined by OT practitioners based on: individual movement deficits at specific joints, joint movements that have the most potential for improvement, and patient preferences of specific tasks that would produce the desired movements.
With shaping, progression of movement tasks is made in a systematic, quantified, and parametric manner which makes the intervention time-specific. By using tasks that are individualized and meaningful for the patient, the experience is positive, especially when combined with feedback which promotes encouragement.
CIMT for the Adult vs Pediatric Patient
CIMT was developed for adults but it is a useful strategy to use with the pediatric population as well. As it is an intensive intervention in its original form, it is not child-friendly and therefore using the modified model is more appropriate. A key distinction between adult vs child, is that the underlying focus of the adult CIMT is on overcoming learned non-use, whereas children may have developmental disuse which requires them to focus on their impairments.
Reference:
Trombly, C.A. (1983). Occupational Therapy for Physical Dysfunction, Second Edition. Baltimore, MD: Williams & Wilkins.
Pedretti’s Occupational Therapy – E-Book (Occupational Therapy Skills for Physical Dysfunction (Pedretti)
https://www.sciencedirect.com/topics/medicine-and-dentistry/constraint-induced-movement-therapy
https://physio-pedia.com/Constraint-Induced_Movement_Therapy_(CIMT)