
The following chart will review the definition, symptoms, and interventions for Multiple Sclerosis, Amyotrophic Lateral Sclerosis, Parkinson’s disease, Guillain-Barre Syndrome, and Myasthenia Gravis.
..
| Disease | Definition | Cause/Who is affected/Prognosis | Progression | Primary Symptoms |
| Multiple Sclerosis (MS)
|
An autoimmune disease in which the body’s immune system attacks the myelin sheaths surrounding the neurons of the brain and spinal cord, causing demyelination and a subsequent slowing or stopping of nerve transmission. | Cause: unknown
Who is affected: Prognosis: |
Four types of MS:
1. Relapsing/remitting – “flare-ups” occur when new lesions or symptoms appear, alternating with periods of remission when no new symptoms occur. |
1. Fatigue – the most common symptom of MS. Primary fatigue – due to cortical damage, -leads to overwhelming feelings of fatigue -Secondary fatigue- due to deconditioning, respiratory muscle weakness, pain. 2. Paresthesias – pins and needles sensations. 3. Sensitivity to extreme heat. 4. Pain 5. Vertigo 6. Emotional reactions -lability -euphoria -reactive depression 7. Visual symptoms -diplopia -scotoma -loss of visual acuity -optic neuritis (loss of vision and pain behind the eye, temporary) 8. Motor symptoms -muscle weakness -impaired coordination -impaired balance; ataxia -partial or complete paralysis -spasticity -intention tremors with movement -impaired bowel and bladder functions; incontinence -impaired sexual functions 9. Cognitive symptoms -impaired short term memory -word finding problems -difficulty attending -slow processing speed -executive function problems |
| Amyotrophic Lateral Sclerosis (ALS) – also called Lou Gehrig’s Disease) 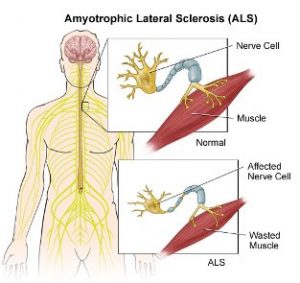 |
Progressive motor neuron disease in which the nerve cells deteriorate and die. | Cause: Three classifications
1. Sporadic – cause is unknown, can happen to anyone, anywhere, 90 to 95% of all cases. Who is affected: Prognosis: Poor. ALS usually leads to death within 5 years after diagnosis. (Stephen Hawking is very much the exception and has lived with ALS for many years.) |
Nerve loss occurs distal to proximal and asymmetrically.
Six stages of function: |
1. Progressive weakness in hands and feet, moves proximally toward trunk. 2. Loss of fine motor control. 3. Difficulty walking with tripping and falling. 4. Slurred speech, difficulty swallowing. 5. Muscle cramps and twitching in arms, shoulders tongue. 6. Difficulty maintaining upright posture or holding head up. 7. Cognitive decline characterized by personality change, irritability, obsessions, poor insight, and pervasive deficits in frontal executive tests. Presentation consistent with the changes to character, social conduct, and executive function in frontotemporal dementia. 8. Does not affect eye function, bowel and bladder function, sensory or sexual functions. |
| Parkinson’s Disease
|
A progressive neurodegenerative disorder in which the brain stops producing the neurotransmitter dopamine, resulting in a decreased ability to regulate the body’s movements and emotions. | Cause: Unknown, possibly caused by a combination of genetic and environmental factors.
Who is affected: Prognosis: |
Five stages of Parkinson’s Disease:
Stage 1. Unilateral – no or very limited loss of function. |
1. Tremors -resting tremors: occur when the extremity is at rest. -intention tremors: tremors that increase in severity when the person thinks about moving the limb. 2. Muscle rigidity and stiffness. 3. Cogwheeling of joints – joint ratchets when moving. 4. Akinesia or Bradykinesia – slow movements or inability to initiate movement. 5. Gait disorders -shuffling gait -falling forward -retropulsion – walking backwards. 6. Postural Instability 7. Mask-like facial expression 8. Micrographia – tendency to write small. 9. Cognitive symptoms -impaired memory, executive function -dementia -depression 10. Communication and oral motor symptoms -hypophonia (soft voice) -lack of expression -swallowing problems -drooling |
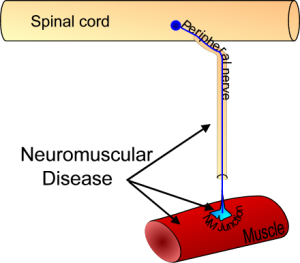
| Guillain-Barre Syndrome
|
An autoimmune disorder in which the immune system attacks the myelin sheaths and axons of the peripheral nervous system. -Does not attack the central nervous system like MS. |
Cause: Unknown. Sometimes preceded by a bacterial infection or virus.
Who is affected: Most common onset between the ages of 30 and 50. Youngest age of onset 20. Prognosis: |
Three stages of Guillain-Barre:
1. Onset and acute inflammatory phase |
1. Tingling sensations in the legs that spread to the arms and upper body. 2. Muscle weakness beginning in the legs and spreading to the arms and upper body. 3. Mild, distal sensory loss. 4. Muscle belly tenderness as diagnostic sign. 5. Fatigue 6. Edema in legs 7. Deep tendon reflexes are absent. 8. Possible facial palsy. 9. Possible autonomic symptoms such as hypotension, diaphoresis, urinary retention. 10. Anxiety |
| Myasthenia Gravis (MG)
|
An autoimmune disorder in which the immune system blocks the neuromuscular junctions between the nerves and the voluntary muscle fibers, causing the signals from the nerves to the voluntary muscles to be lost. | Cause: Unknown:
Who is affected: Anyone at any age. Prognosis: Good with treatment. |
Progressive muscle weakness.
-progression varies between individuals. |
1. Increasing muscle weakness with activity, weakness improves with rest. 2. Drooping eyelid on one side. 3. Impaired facial muscles with slurred speech. 4. Difficulty chewing and swallowing. 5. May experience difficulty breathing. 6. End stage – may experience quadriparesis, respiratory failure. |
.Occupational Therapy Treatment
| Disease | Symptom/Treatment | Precautions | Examples | Video |
| Multiple Sclerosis (MS) | Muscle weakness: -gentle therapeutic exercise -ergonomic positioning -education in joint protection techniques Visual impairment: -clear walkways in the home -provide contrast at the edges of steps or carpeting (bright or dark electrical tape) -adaptations for low vision (large print, large buttons, etc.) Sensory impairments: -sensory re-education -adaptations for safety to prevent burns Cognitive impairments: -adaptations for short term memory, executive functioning. -educate family members in how to allow extra time for processing, word finding. Spasticity: -resting splints, AFOs Dysphagia: -thickened liquids -allow extra time to chew and swallow Fatigue: -educate patient and family in energy conservation and work simplification techniques |
1. Avoid extreme physical stress -strengthening should be gradual -allow for rest breaks -plan activities over several sessions. 2. Avoid thermal physical agent modalities. 3. Educate patient and family about exacerbations and remissions. -disease prognosis -exacerbations happen, patient is not faking illness. |
-Low load strengthening for endurance. -Use of a utility cart to transport heavy pots and pans in the kitchen. -Use of a magnifier with a light to read. -Prioritize activities, alternate heavy and light tasks. -Training in visual checks of skin for burns, injuries, pressure areas. -Use of a universal cuff to hold eating utensils or grooming items if hand weakness is extreme. -Use of a planner to write down appointments, schedules, birthdays, etc. |
|
| Amyotrophic Lateral Sclerosis (ALS) | Muscle spasticity: -AAROM and PROM to prevent contractures -positioning to reduce spasticity -diaphragmatic positioning to reduce the work of breathing Limited upper extremity movement: -adaptations for functional activities, such as built-up handles on eating and grooming utensils or a universal cuff. Limited mobility: -Cane -AFO for foot drop -Walker -Power wheelchair in late stage Dysphagia: -adapt food consistencies -allow extra time to eat -reduce distractions during eating Fatigue: -education in energy conservation and work simplification techniques Limited Communication: -augmentative communication -single switch or eye gaze control Caregiver education: -management of dysphagia -environmental modifications -prevention of skin breakdown |
1. Progressive resistive exercise to strengthen muscles may cause cramping, fatigue and is contraindicated 2. Monitor for aspiration and choking – may need suction. 3. Monitor for decreased respiratory function 4. Monitor for pressure sores. 5. Avoid overwhelming the patient with adaptive equipment, as the person may not receive adaptations well. |
-Bilateral resting splints to prevent hand and finger contractures -Use of a plate guard and built-up handle utensils to eat meals -Assist the patient in rearranging the kitchen to position frequently used items at wheelchair height -Training family in visual checks of skin for pressure areas. -Use of a universal cuff to hold toothbrush while brushing teeth -Use of a mobile arm support to move upper extremity while feeding self. |
|
| Parkinson’s Disease | Impaired functional mobility: -adapt home to clear pathways -recommend flat shoes, not rubber soled shoes (can stick, cause falls) -avoid tight spaces -encourage group exercise to manage bradykinesia, elevate mood Muscle rigidity and pain: -moist heat -gentle ROM -closely monitor pain during exercise Deficits in self care and feeding skills: -distal wrist weights to manage tremors -weighted utensils -thickened liquids -soft food consistencies and small portions Problems with communication: -use a mirror for facial awareness -felt tip pen for writing -address vocal responses – volume Employment: -sedentary job with limited need for communication and gross motor movement Family and caregiver training: -use of timed auditory cues to assist patient with initiating and speeding up movements -medication management |
1. High risk for falls due to postural instability -keep pathways clear -remove throw rugs 2. Prone to aspiration due to dysphagia. 3. Mask-like face may make it difficult to determine emotions. Closely monitor pain and signs of depression. 4. Medication side effects may cause orthostatic hypotension, stomach problems, dystonia. |
– Metronome training for repeated, rhythmic movements. -Use of wrist weights during cooking and cleaning tasks to reduce tremors. -Wheelchair positioning to compensate for poor postural control. -Use of a hand based weight and a fine tip marker to write a grocery list. |
|
| Guillain-Barre Syndrome | Acute Phase: Occupational Therapy evaluation and treatment may not be ordered during this phase. If it is, focus should be on positioning and splinting to prevent muscle tightness and contracture. PROM may be provided as tolerated but should not be overdone.
Plateau Phase: |
-Watch for signs of fatigue during treatment, discontinue activity if needed to prevent overexertion. -Watch for muscle substitution patterns during movement ; provide adaptations to compensate for weak or fatigued UE muscles to prevent long term pain or contracture from substitution. |
-Upright positioning in a high backed reclining wheelchair for meals and activities. -Use of a mobile arm support and universal cuff for self feeding and grooming tasks. -Active-assistive range of motion using a towel to slide the arms along a table top. -Use of an intercom system in the home to improve contact with caregiver and reduce anxiety. -Home exercise program that includes low resistance and reps in short sets to conserve energy. -Functional capacity evaluation and/or ergonomic assessment prior to return to work. -Adaptations for residual upper extremity weakness, including built-up handle utensils, a jar opener, ergonomic keyboard on the computer, lever style door handles, etc. |
|
| Myasthenia Gravis | Upper extremity weakness: -exercise and activity to regain muscle power and endurance -adaptations for extreme weakness, including overhead slings, mobile arm supports, electronic devices Facial and oral-motor weakness: -educate in adaptations to food consistencies, including thickened liquids, small bites, food consistencies -train in self-check of facial muscle status in mirror Fatigue: -educate patient in disease process, fact that muscles fatigue with activity, recover with rest -educate in energy conservation techniques -educate in work simplification and adaptations to lifestyle -assist patient and family in modifying home to compensate for low endurance and weakness |
1. Attend to and respect the patient’s activity tolerance. 2. Watch for changes in respiration and emotional distress during therapy. 3. Use the Borg Scale of Perceived Exertion to monitor the patient’s perceived exertion levels. |
-UE exercises that utilize low resistance and reps in short sets to conserve energy. -Gradually increasing the amount of time engaged in activity to increase endurance. -Education in how to alternate heavy and light housekeeping tasks and home to conserve energy. -Adapting the kitchen to place frequently used dishes and cooking utensils between chest and waist height. -Educating patient in how to monitor fatigue levels by checking for eyelid or facial droop in a small pocket mirror. |
All of the neurological conditions discussed here result in muscle weakness and decreased endurance levels. Patients should be educated in energy conservation and work simplification techniques to help them compensate for weakness and endurance.
Here are a few ways patients can conserve energy and simplify work tasks:
*Write a daily to-do list and prioritize activities. Do the tasks with the highest priority first. If energy runs out, reschedule lower priority activities for another day.
*Alternate heavier activities with light activities during the day. For example, vacuum the floor, then sit down and pay bills.
*Schedule rest breaks during the day and take them.
*Rearrange furniture to make walkways clear and straight.
*Rearrange cupboards and closets to place the most frequently used items between chest and waist height.
*Use a wheeled cart to transport heavy items, rather than carrying.
*Slide heavy pots and pans along the countertop, rather than carrying.
*Bathe sitting down, using a bath bench or shower chair and a hand held shower.
*Do not be afraid to ask for help!
References:
-The Benefits of Group Occupational Therapy for Patients with Parkinson’s Disease. American Journal of Occupational Therapy, June 1987, Vol. 41, 360-365. doi:10.5014/ajot.41.6.360
-Cooper, C. (2007) Fundamentals of Hand Therapy: Clinical Reasoning and Treatment Guidelines for Common Diagnoses of the Upper -Extremity. St. Louis, MO: Mosby/Elsevier.
-Physical Dysfunction Practice Skills for the Occupational Therapy Assistant, 3rd Edition – Mary Beth Early
-Quick Reference to Occupational Therapy, 2nd Edition – Kathlyn L. Reed
-Myasthenia Gravis
-Parkinsonism
-Guillain-Barre Syndrome
-Dysphagia and multiple sclerosis
-Ventilatory control in ALS
-Exercise is effective for delaying respiratory insufficiency in ALS patients (Aboussouan 2009, de Almeida et al. 2012)