| Term | Definition | Key Element to Therapeutic Approach/Environment | Role of the Therapist | Example | Photo/Video |
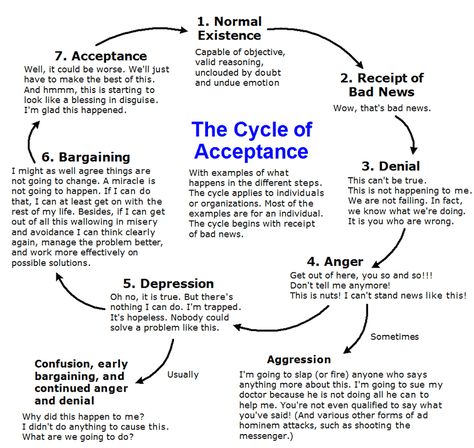
| Acceptance | When someone begins to comprehend that their situation is reality. They are no longer in denial. | An attitude of acceptance is important when dealing with a difficult situation. This does not mean that the patient gives up hope, or stops striving for a positive outcome, it simply means they accept the reality of their circumstances and chose to adjust their expectations to that new reality. | Part of the role of a therapist is to help a client move from a place of denial to a place of acceptance. Therapeutic work will be ineffective if a client remains in denial instead of moving forward in full acceptance. | A young man who recently lost his leg to a motorcycle accident, refuses to accept his new circumstances. He is fixated on getting a prosthetic leg and “getting back to normal”. His therapist works to help him understand the full reality of the loss of his leg and to give him practical skills to move forward with hope.
Acceptance is the last stage of the Kubler-Ross Model which is also known as the 5 stages of grief (denial, anger, bargaining, depression, and acceptance).
|
|
| Apraxia | Apraxia is caused by disease or brain injury. Apraxia can affect speech and or motor skills. The patient has the physical ability and desire to speak or walk, but the brain is not able to communicate the words or movements to the body. Acquired Apraxia is more common in patients who are 40 and over. Developmental Apraxia is seen in children and affects the ability to form words. | Physical and speech therapies are used to help the patient overcome symptoms. It is important to develop short and long treatment goals for treatment. Some patients with speech apraxia may benefit from sign language training. | Occupational therapy is key for patients struggling with apraxia. The OT provides skill training to help the patient improve their quality of life. This is especially true for young patients and their families – these families will need encouragement and support to work toward long-term improvement. | A patient has been diagnosed with Apraxia after suffering a stroke. The patient can understand words and has the physical ability to speak but is unable to form words. She has a strong desire to speak but can only communicate with hand motions, noises and gestures. The OT will work with this patient to provide and support non-verbal forms of communication while facilitating therapies with the long term goal of allowing the patient to speak again. | 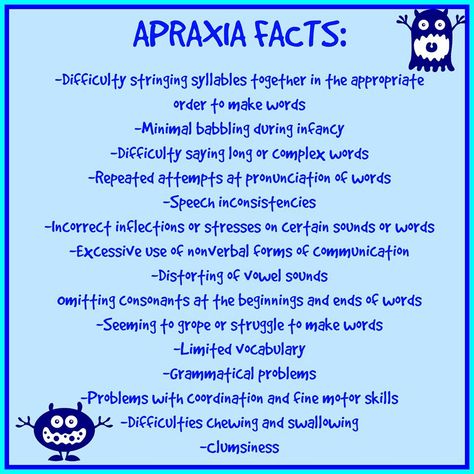 |
| Clubhouse | The clubhouse is a specific model of Psychological Rehabilitation for people with mental illness or disabilities. | A key to this type of environment is understanding that the people involved in the program are not patients or clients. They are willing participants, usually known as members. These members work alongside the staff to create a uplifting, supportive, engaging environment. | In the clubhouse setting, there are no therapists or psychologists. The focus is on the member’s strengths and abilities rather then their mental illness. | A woman with a history of substance abuse joined a clubhouse in her community with the goal of finding a job. The club and it’s members help to develop her confidence, her skills, and allows her to participate in work programs and education programs. She feels empowered and supported because of the friendly, non-threatening environment. | Clubhouse International |
| Community-Based Mental Health Services | Community based mental health care is an alternative to in-patient treatment. It grew out of the deinstitutionalization movement of the 1960’s. It is more cost effective and offers a simple, less invasive form of mental health care while allowing the patient to continue to function and flourish in their own community. | Community based care promotes a well-rounded model of treatment. It helps minimize the stigma associated with mental illness while providing well-organized services and support for a wide range of concerns. Patients generally report a higher level of satisfaction with community health services than with a standard in-patient setting. | The OT maintains aspects of self care, lifestyle, medications, and education. | A 45 year old man with a history of serious mental illness is referred to a psychiatric rehabilitation program. He attends the program on a daily basis. He receives training in selfcare, social skills, and job readiness. He may also participate in individual and group therapy sessions. | 
|
| Community residential setting | This is the step between an inpatient and an outpatient setting. It maintains some structure and supervision while allowing the patient to regain some freedom. It is the first step to practicing new skills in the outside world. | This type of setting is all about balance. The OT will need to help the patient balance their new freedom while avoiding the old bad habits or relationships. | The OT can help the patient maintain the skills they learned in a more structured program while encouraging them to become self sufficient. Each patient may need a different level of supervision and it may become clear that some patients are not ready for life on their own yet. | A young woman was recently released from rehab and is recovering from a heroin addiction. As part of her court ordered treatment she needs to be supervised, but also needs to get a job. The best solution for her is a halfway house where she can continue her therapy in the mornings and evenings but is free to work at her job during the day. This program also provides her a safe place to live and supports her recovery by requiring her to keep a strict schedule. | |
| Delusions | Delusions are beliefs that are not based on reality. They are irrational, but the client believes them to be true, even when shown clear evidence that they are false. | When working with a patient who experiences delusional thinking, it is important to avoid focusing on the delusion – this can reinforce the delusion to the patient. Instead, focus on thought-provoking activities. | The OT should try to maintain a calm demeanor. It can be frustrating to confront irrational thinking on a daily basis but it is important to remain focused on the well-being of the patient and avoid becoming angry. It is the role of the OT to gently refocus the patient until he is able to reject his false beliefs. | After experiencing a traumatic event, a client believes that his mind has been implanted with a device that reads his thoughts. This belief leads to irrational behavior like harming himself to try and remove or turn off the device. | Examples of Delusions |
| Denial | Believing something to be untrue or unreal. Refusal to face facts. Part of the process of grieving. | We all experience denial as some point in our lives. It is a way for our minds to cope with difficult situations. However, if a patient remains in denial for too long it can keep them from being able to fully engage in treatment or therapy. Almost any diagnosis can be followed by denial a OT needs to be ready to address it on a regular basis. Denial of a problem can force a patient to avoid treatment for a long time. | Denial can be overcome by continually pointing the patient back to the reality of the situation, while encouraging the patient to be hopeful. Sometimes it simply takes time to overcome denial. Often is it helpful to educate the patient on other, more effective coping mechanisms like a new activity or talk therapy. | A client refuses to accept the fact that she is an alcoholic. She doesn’t believe that the problem is serious enough to require treatment and refuses to recognize the affects the drinking has on her life, her body and her relationships. | Denial Defense Mechanism in Mental Health |
| Hallucination | Experiencing something as reality that is not. Any of the senses can be affected, but the most common type of hallucination is auditory. | Hallucinations are a sign of serious mental illness or brain damage. They can be short-term or long term. When treating a patient with hallucinations it is important to reduce the stimulation in their environment. Let them be in a quiet place, without noises, bright lights or other people. | When a patient is experiencing a hallucination, the OT should remain calm and provide a peaceful space for the patient. The OT should speak in a quiet but firm voice. Clearly communicate what is happening and encourage them to share more about the sensations they are having. | A young mother has had several sleepless nights with her newborn baby. She begins hearing the baby crying, but when she checks she finds the baby is sleeping. Her exhaustion has lead her to hallucinate the noise of a crying baby. | What hallucination reveals about our minds |
| In-patient psychiatric unit | Short-term hospitalization for patients experiencing symptoms of mental illness. This is sometimes referred to as Emergency Care. | Patients are usually admitted to inpatient care while they work through a specific set of challenges or symptoms. The majority of patients being treated for mental illness will not need any type of long-term hospitalization. It is important to address the fears that the patient may have about an inpatient setting. | The goal of the OT in this setting should be to stabilize the patient as quickly as possible and help them move to a less restrictive setting. The OT needs to assess the roles the client had before they were admitted and see how many of those roles they can return to when they are discharged. Teaching self-care is also important. | Out of fear for her safety, a mother has asked that her bi-polar son be admitted into a psychiatric unit. He has been showing increased aggression, explosive anger and has threatened self harm. It is decided that the young man and his mother will both be safer if he is treated in an in-patient setting. | Differences between inpatient and outpatient treatment for mental illness |
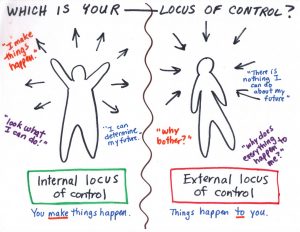
| Locus of Control
|
Locus of control refers to the extent to which people feel that they have control over the events that influence their lives.
If you believe that you have control over what happens, then you have what psychologists refer to as an internal locus of control. If you believe that you have no control over what happens and that external variables are to blame, then you have what is known as an external locus of control. This individual typically believes that external factors are what contribute to their personal failures or success. It is important to note that locus of control is a continuum. No one has a 100 percent external or internal locus of control. Instead, most people lie somewhere on the continuum between the two extremes. |
A patient’s locus of control can have a major impact on their life, from how they cope with stress to their motivation to take charge of their life. Having more of an internal locus of control is a positive attribute. It means that they believe that their own actions have an impact. If they tend to have more of an external locus of control, they tend to view themselves as simply being a passive bystander who is caught up in the flow of life. | The goal of the OT is to help the patient move away from an extreme external locus of control. With a patient who has more of an external locus of control, they might find it helpful to start actively trying to change how they view situations and events. Rather than viewing themselves as a passive bystander, they should be encouraged to think about the actions they can take to have an impact on an outcome. They should be encouraged them to take responsibility for their actions. | Internal locus of control – A student who passed their exam would say “I totally aced that test because the teacher had the class participate in a really good review session”. External locus of control – A student who failed their exam would say “I failed that test because the teacher didn’t provide me with a good enough study guide” |
 |
| Long term hospitalization | When a patient exhibits extreme symptoms, does not respond to treatment, or is seen to be a risk to themselves or others, long-term hospitalization may be required. | Recognize patterns in behavior that may have gone unnoticed when the patient was not receiving 24/7 care. For patients admitted due to injury or illness, the treatment plan may need to change they improve or decline. | As with short term care, the OT should focus on the stabilization of symptoms. In long-term care it is sometimes necessary to conduct further evaluations of the patient’s behavior in order to have a more specific diagnosis. Once a full diagnosis is available, a more tailored plan can be created for the treatment and support of the patient. | After several weeks in the in-patient unit, the patient from the previous example has not improved. His moods have not stabilized and he has continually showed aggression towards the hospital staff. It is decided that it would be better for this young man if he were moved to a long-term care unit for further evaluation and treatment. | Inpatient care- duration |
| PTSD | Symptoms include anxiety, loneliness, inability to sleep, inability to feel joy, anger, aggression, nightmares (night terrors), feeling guilty, risky behaviors, self-harm, suicidal thoughts. | Since PTSD is often accompanied by anxiety and depression, medication to treat those two conditions are often prescribed for those with PTSD. Therapy is essential for PTSD patients and should focus on helping the patient understand and overcome that initial trauma. Support groups can also be helpful. | The first goal of an OT should be to determine how much the PTSD has impacted the patient’s performance and work to discover the specific triggers for the patient. Triggers should be understood and addressed while providing training to the patient and their caregivers to avoid triggers and create healthy routines. | A soldier has returned home from tour, where he witnessed the death of several of his friends. The soldier now feels guilty that he was the one to survive. He drinks and smokes often and he feels anxious in social settings. He is unable to sleep, eat, or work. He shares that he doesn’t think he has a future and has contemplated ending his life. | American Occupational Therapy Association PTSD Fact Sheet |
| Stigma | Stigma occurs when society labels someone as tainted or less desirable. Stigma involves three elements; a lack of knowledge (ignorance), negative attitudes (prejudice) and discrimination.
Two main types of stigma occur with mental health problems, social stigma and self-stigma. |
Stigma causes people to feel ashamed for something that is out of their control. Worst of all, stigma prevents people from seeking the help they need.
Cognitive Behavioral Therapy (CBT) can help patients cope with the negative effects of being stigmatized. This therapeutic approach helps the patient learn to identify, question and change their thoughts, attitudes, and beliefs so that they can modify their emotional and behavioral reactions. It is a “problem-focused” and “action-oriented” method of dealing with discrimination. |
As occupational therapists, we have an obligation to combat mental health stigma and reduce barriers to accessing mental health services for our patients across all settings. E.g. Talk openly about mental health. Advocate for equality between physical and mental illness. Educate people – they need to understand that mental illness is a disease. Show compassion for those with mental illness – model compassion for others. |
Many people with mental illness are doubly challenged. On one hand, they struggle with the symptoms and disabilities that result from the disease. On the other, they are challenged by the stereotypes and prejudice that result from misconceptions about mental illness. As a result, people with mental illness are robbed of the opportunities that define a quality life: good jobs, safe housing, satisfactory health care, and affiliation with a diverse group of people.
|
A Social Experiment on Mental Health Stigma
Breaking the Stigma and Shame of Mental Illness
|
| Supported employment/vocational rehabilitation | A collaboration between the patient, the OT, and an employer to help the patient improve their skills in the workplace. | Vocational rehabilitation and Supported Employment can be extremely helpful to a wide-range of patients. For a person with an intellectual disability, entering the workforce for the first time can be overwhelming and returning to work after an injury or illness can be very difficult. Having specific and tailored support during this transition is valuable to both the patient and the employer.
|
In this setting, the OT works to provide the patient with all the tools they need to thrive in the workplace. This includes skills training, interpersonal communication, interview and resume support. The OT may need to serve as an advocate for the patient to their employer. In some settings, the OT may also communicate with perspective employers to set up interviews for the client. | A woman with Down’s Syndrome works with her OT to find and interview for a job. The OT prepares her for the interview, goes with her on the interview, and goes to work with her for the first couple weeks to make sure everything is going smoothly. The OT will regularly check in with the employer to see if how the client is doing and if any changes need to be made. | Living Unlimited – Vocational Rehabilitation |
Intervention Models used in Mental Health Care
Assertive Community Treatment (ACT) 
Assertive community treatment (ACT) programs also known as Programs for Assertive Community Treatment (PACT), are comprehensive community-based intervention models for patients with severe mental illness.
These programs provide intensive treatment, rehabilitation, and support services to patients in their homes, at their jobs, and in social settings. In this approach, a multidisciplinary mental health team is organized as a type of mobile mental health agency. The purpose of the ACT team is to take an interdisciplinary/interprofessional team approach to treating these individuals, with each member fulfilling their unique role.
Individual Placement and Support (IPS) ………
IPS is a model of supported employment for people with serious mental illness. IPS supported employment helps people living with behavioral health conditions work at regular jobs of their choosing.
IPS is based on 8 principles:
1. Competitive employment
Jobs anyone can apply for, pay at least minimum wage/same pay as coworkers with similar duties, and have no artificial time limits imposed by the social service agency.
2. Systematic job development
Employment specialists systematically visit employers, who are selected based on the job seeker’s preferences, to learn about their business needs and hiring preferences.
3. Rapid job search
IPS programs use a rapid job search approach to help job seekers obtain jobs rather than assessments, training, & counseling. The first face to face contact with the employer occurs within 30 days.
4. Integrated services
IPS programs are integrated with mental health treatment teams.
5. Benefits planning
Employment specialists help people obtain personalized, understandable, and accurate information about their Social Security, Medicaid, and other government entitlements.
6. Zero exclusion
People are not excluded on the basis of readiness, diagnoses, symptoms, substance use history, psychiatric hospitalizations, homelessness, level of disability, or legal system involvement.
7. Time-unlimited supports
Job supports are individualized and continue for as long as each worker wants and needs the support.
8. Worker preferences
IPS program services are based on each job seeker’s preferences and choices rather than the employment specialist’s and supervisor’s judgments.