Huntington’s Disease
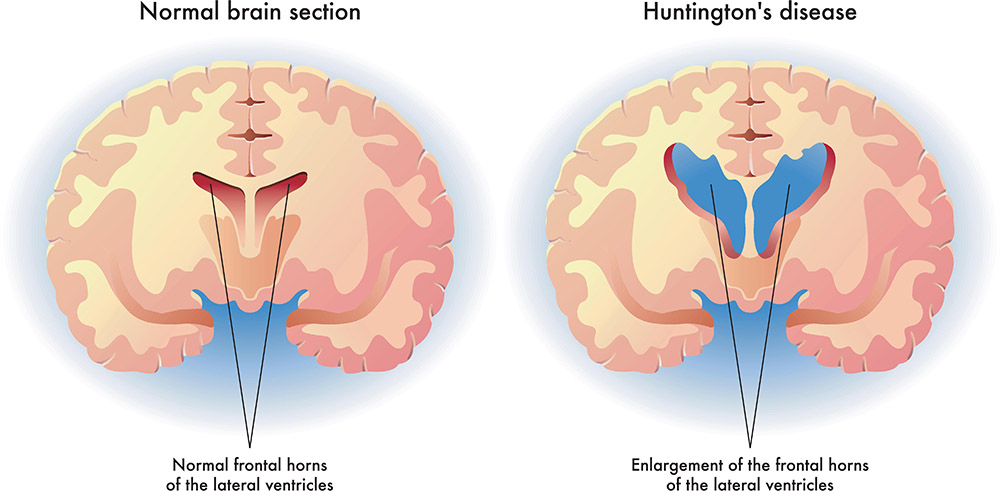
Huntington’s Disease is a progressive neurological disorder.
-The disease is genetic, has no cure, and is fatal.
-Age of onset is usually between age 30 and 50.
–Life expectancy after onset is 10 to 25 years, with death usually occurring due to a complication such as heart failure, aspiration pneumonia or suicide.
-Everyone who has a parent with Huntington’s Disease has a 50/50 chance of inheriting the genetic mutation that causes the disease and everyone who inherits the gene will develop the disease.
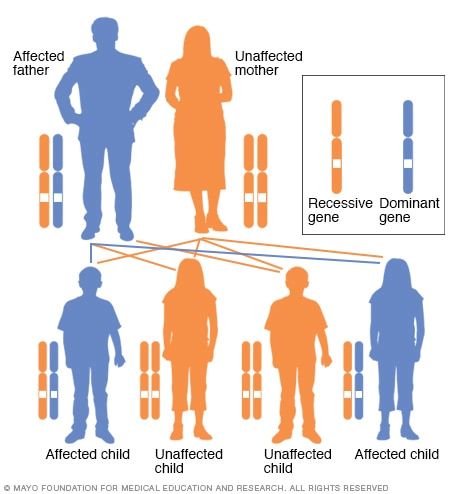
In an autosomal dominant disorder, the mutated gene is a dominant gene located on one of the non-sex chromosomes (autosomes). You need only one mutated gene to be affected by this type of disorder. A person with an autosomal dominant disorder — in this case, the father — has a 50% chance of having an affected child with one mutated gene (dominant gene) and a 50% chance of having an unaffected child with two normal genes (recessive genes).
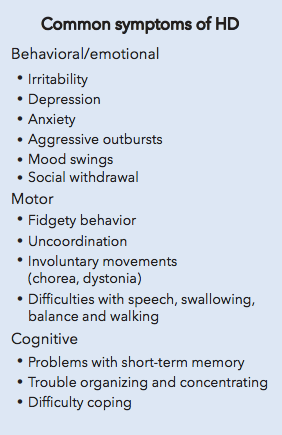
Characteristics of Huntington’s Disease
 .
.
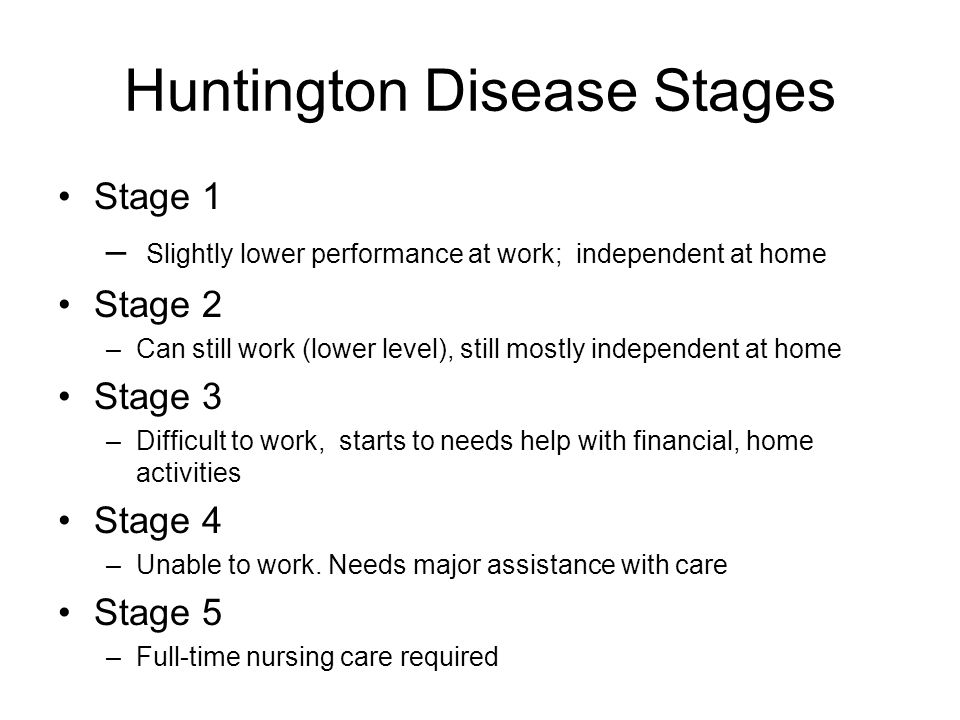
Stages of Huntington’s Disease
HUNTINGTON DISEASE IN 5 STAGES
Stage 1: Early Stage
The early stage starts when a person first begins experiencing motor symptoms, and can last up to eight years from disease onset. At this stage, motor symptoms are not debilitating. Most individuals in the early stage are fully functional at home and at work, and usually maintain typical pre-disease levels of independence when it comes to everyday activities such as finances, home responsibilities, and activities of daily living such as eating, dressing, and bathing. Mild cognitive symptoms and psychiatric changes may begin to occur among individuals at this disease stage.
Stage 2: Early Intermediate Stage
The early intermediate stage of Huntington’s can last between three and 13 years from disease onset. During this stage, patients begin to experience impairments in day-to-day living. For instance, people in the early intermediate stage may be able to do their job, but at a lower capacity. Individuals at this stage may find that some daily activities are more difficult, and may require assistance with some aspects of daily tasks. Chorea, which is irregular involuntary movement in multiple areas of the body, may become more severe at this stage.
Stage 3: Late Intermediate Stage
The late intermediate stage usually lasts between five and 16 years from disease onset. An individual at this stage is no longer able to work or manage household responsibilities. A patient’s ability to think also may become more impaired, and he or she will require substantial help for daily financial affairs, domestic responsibilities, and activities of daily living. Psychiatric and behavioral symptoms, including irritability, anxiety, and impulsiveness may become evident. In general, cognitive, psychiatric, and motor features worsen at this stage.
Stage 4: Early Advanced Stage
Typically lasting between nine and 21 years from disease onset, the early advanced stage is characterized by a need for full assistance in daily living. A person in this stage of Huntington’s cannot live independently. Some patients reside in their home with help from either family or professionals, while other individuals may decide that their needs will be better met at an extended care facility. A person in this stage of disease will be aware of daily living activities that have to be done, but will require major assistance to do them.
Stage 5: Advanced Stage
The advanced stage lasts between 11 and 26 years from disease onset. Patients with Huntington’s at this late stage will need total support in daily activities from professional nursing care. Chorea lessens at this stage, but parkinsonism — which includes slowness, stiffness, teeth grinding, and abnormal limb postures — increases. Walking/mobility, and a person’s ability to maintain an upright posture also worsen, and there is an increased risk of falls. Speech can become difficult at this stage and the patient may go through periods of confusion and screaming. The ability to swallow also can worsen, and there can be extreme fluctuations in blood pressure and temperature.
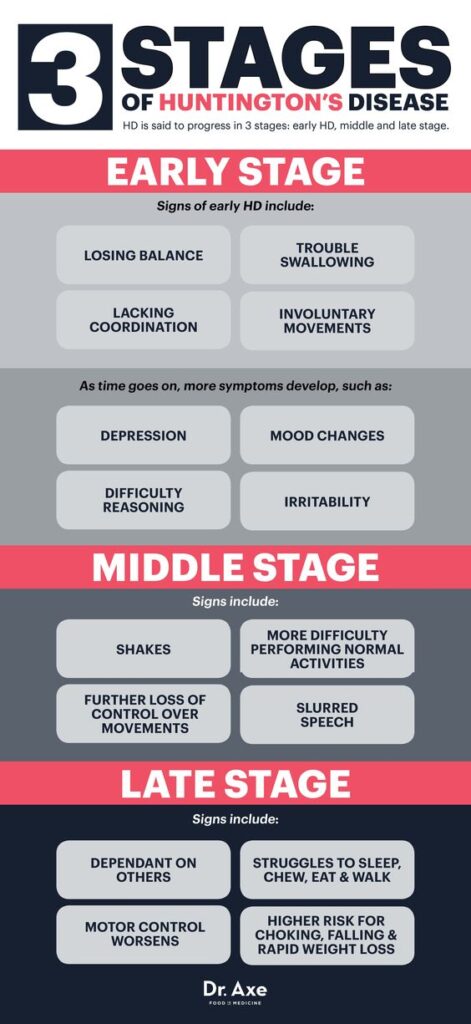
HUNTINGTON’S DISEASE IN 3 STAGES
EARLY STAGE
In early stage HD, individuals are largely functional and may continue to work, drive, handle money, and live independently. Symptoms may include minor involuntary movements, subtle loss of coordination, difficulty thinking through complex problems, and perhaps some depression, irritability, or disinhibition.
MIDDLE STAGE
In middle stage HD, individuals lose the ability to work or drive and may no longer be able to manage their own finances or perform their own household chores, but will be able to eat, dress, and attend to personal hygiene with assistance. Chorea may be prominent, and people with HD have increasing difficulty with voluntary motor tasks. There may be problems with swallowing, balance, falls, and weight loss. Problem solving becomes more difficult because individuals cannot sequence, organize, or prioritize information.
LATE STAGE
In late stage HD, individuals require assistance in all activities of daily living. Although they are often nonverbal and bedridden in the end stages, it is important to note that people with HD seem to retain some comprehension. Chorea may be severe, but more often it is replaced by rigidity, dystonia, and bradykinesia. Psychiatric symptoms may occur at any point in the course of the disease but are harder to recognize and treat late in the disease because of communication difficulties.
| EARLY STAGE | MIDDLE STAGE | LATE STAGE | |
| Stage 1 Early Stage |
|||
| Stage 2 Early Intermediate Stage |
|||
| Stage 3 Late Intermediate Stage |
|||
| Stage 4 Early Advanced Stage |
|||
| Stage 5 Advanced Stage |
According to the Huntington’s Disease Society of America, Huntington’s Disease can be described as having ALS, Parkinson’s Disease, and Alzheimer’s Disease, all at the same time. The following chart provides an overview of the primary characteristics of Huntington’s Disease.
Symptoms
| Motor Control Symptoms | • Chorea – abnormal involuntary movements • Dystonia – involuntary muscle contractions • Motor impersistence – the inability to maintain postures or positions without prompting • Dysarthria – difficulty controlling the muscles used for speech • Dysphagia – difficulty swallowing • Poor posture • Incoordination • Delayed initiation of movement • Impaired balance and gait |
| Cognitive Symptoms | • Loss of executive functioning • Difficulty with multi-tasking • Rigid, inflexible thinking • Poor concentration, easily distracted • Impaired visual-spatial abilities • Impaired impulse control • Diminished vocabulary • Poor insight • Short term memory loss |
| Psychiatric Symptoms | • Depression • Anhedonia – loss of sexual libido • Suicidal ideation • Social isolation • Disrupted sleep patterns • Delusions • Hallucinations • Paranoia • Irritability |
……………..
Implications for Occupational Therapy Treatment
People with advancing Huntington’s Disease have difficulty completing any functional activities independently. The involuntary muscle spasms make it hard for patients to do much with their hands. Patients also have difficulty maintaining healthy body weight due to unknown metabolic issues as well as difficulty chewing, swallowing, and handling utensils.
This video includes an interview between an occupational therapy student and a neurologist regarding occupational therapy intervention for people with Huntington’s Disease, as well as a simulated patient evaluation and training in the use of adaptations to compensate for impaired cognitive skills.
| Task | Interventions | Example |
| Eating | -Work with speech therapy to modify food and liquid textures to increase ease of swallowing -Provide adaptive dishes and utensils to encourage self feeding for as long as possible. -Encourage a modified eating environment with minimal distractions. |
An occupational therapist help a man with Huntington’s Disease to feed himself by training him in the use of a plate guard, a swivel spoon and a non-skid placemat. |
| Bathing and Hygiene | -Provide grab rails and adaptive seating for toileting and bathing. -Make sure that adaptive seating is of a type that will not cause injury if a patient has sudden total body extensor tone. |
An occupational therapist recommends a tilt in space shower chair for a nursing home patient with Huntington’s Disease who repeatedly slides out of a regular shower chair due to extensor tone. |
| Dressing | -Recommend loose fitting clothing with elastic waistbands and front closures, as well as supportive, low heeled shoes. -Provide zipper pulls for jackets and coats. -Recommend that clothing be laid out for patients who cannot organize and initiate dressing. |
A woman with Huntington’s Disease wants to continue to wear her favorite pair of jeans but she cannot button the waistband. The occupational therapist adapts the closure with an elastic tab to convert the waistband to pull-on style. |
| Grooming | -Recommend adaptive grooming devices, such as electric razors or beard trimmers, electric toothbrushes. -Recommend using salon services for hair styling, manicures and pedicures. |
An occupational therapist recommends an electric toothbrush to a man with Huntington’s Disease who cannot hold on to a manual toothbrush to brush his teeth. |
| Household management | -Provide adaptive equipment and assistance with kitchen reorganization to improve safety during meal preparation. -Recommend pre-packaged microwavable meals. -Clearly label cupboards and closets. -Help patients locate assistance with tasks that they can no longer complete, such as shopping, heavy cleaning, financial management, etc. |
An occupational therapist labels the cupboards and drawers in the kitchen of a woman with Huntington’s Disease so that she can remember where food, dishes and utensils are located. |
| Mobility | -Assist patients in removing safety hazards from living areas, such as throw rugs and small, unnecessary pieces of furniture. -Train patients in methods of carrying items to keep hands free while walking so that hands may be used to stabilize on grab rails or furniture. Using a shoulder bag is an example. -Recommend methods of emergency communication in the event of a fall, such as carrying a cell phone or wearing an emergency communication button. |
An occupational therapist recommends that a man with Huntington’s Disease carry his cell phone in his shirt pocket at all times so that he can call his neighbor for help if he falls. |
| Cognitive Skills | -Teach patients and their caregivers how to use planners, calendars, alerts on electronic devices, and similar memory aids. -Break down tasks into smaller steps. -Help patients to establish a daily routine and to stick to that routine. -Ask direct questions and offer specific choices rather than asking open ended questions. -Give patients time to respond to questions or instructions as response time can be delayed. |
An occupational therapist assists the caregiver of a woman with Huntington’s Disease in setting up a calendar and alert system on the woman’s computer to help her remember her daily routine. |
| Psychosocial Issues | -Educate the patient, family and caregivers in how to keep the patient’s environment calm and consistent. -Discuss stressors that can trigger frustration, irritability, or outbursts and help patients and caregivers to avoid those situations. -Avoid confrontational situations with patients. Instead, attempt to redirect patients to other topics or activities. |
An occupational therapist provides treatment to her patient with Huntington’s Disease in the later afternoon when the therapy clinic is quiet. |
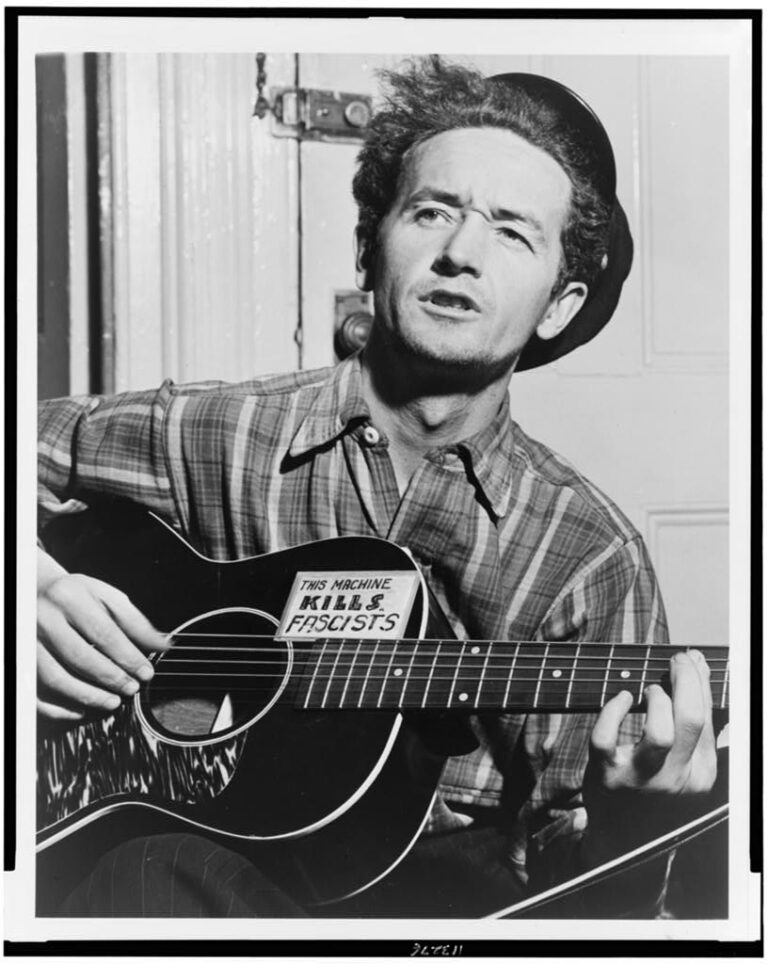
Musician Woody Guthrie passed away from complications of Huntington’s Disease in 1967. His wife Marjorie Guthrie spearheaded the movement to research for a cure for Huntington’s Disease.
References
* Pedretti, L. W., & Early, M. B. (Eds.). (2001). Occupational therapy: Practice skills for physical dysfunction (pp. 3-12). London: Mosby.
* “Huntington Disease.” Genetics Home Reference. N.p., n.d. Web. Retrieved from http://ghr.nlm.nih.gov/condition/huntington-disease on February 26, 2018
* Cook, C., et. al. (2012). Occupational Therapy for People with Huntington’s Disease: Best Practice Guidelines. European Huntington’s Disease Network. Retrieved from: file:///C:/Users/meyda/AppData/Local/Packages/Microsoft.MicrosoftEdge_8wekyb3d8bbwe/TempState/Downloads/Occupational%20Therapy%20for%20people%20with%20Huntingtons’s%20Disease%20best%20practice%20guideline%20(2).pdf on March 10, 2018.