 ………..…
………..… 
Common Causes:
Types/Levels of Amputations
…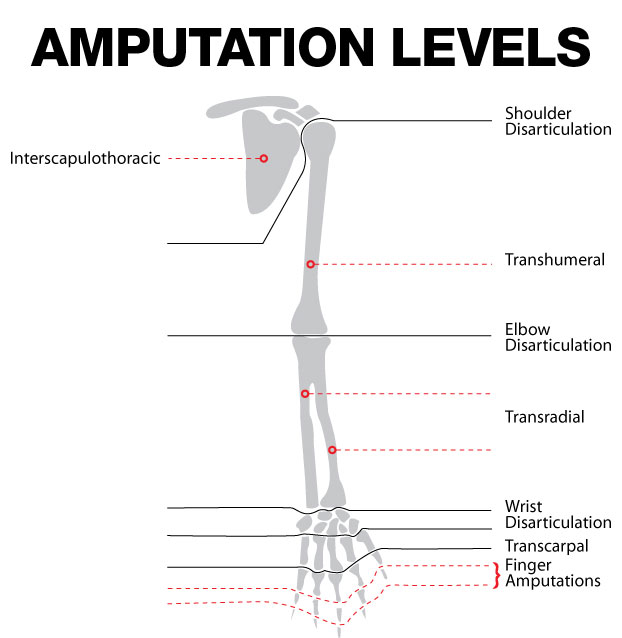
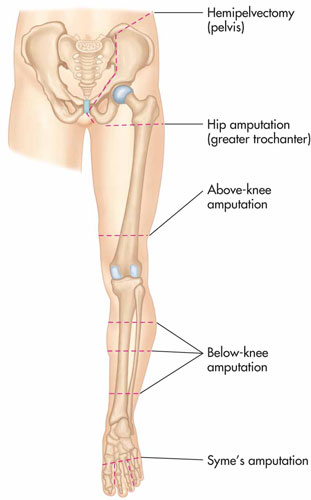
| Extremity | Type | Description |
| Upper | Forequarter | Clavicle, scapula, and entire upper extremity removed |
| Upper | Shoulder disarticulation | Entire upper extremity removed at the shoulder joint |
| Upper | Above elbow | A portion of upper extremity removed, above the elbow but below the shoulder |
| Upper | Elbow disarticulation | Forearm and hand removed at the elbow joint |
| Upper | Below elbow | A portion of the forearm plus the wrist and hand are removed below the elbow but above the wrist |
| Upper | Wrist disarticulation | The entire hand is removed at the wrist joint |
| Upper | Trans metacarpal | The fingers are removed through the metacarpal bones |
| Upper | Digital | A finger or multiple fingers are removed at any level above the metacarpophalangeal (MP) joint |
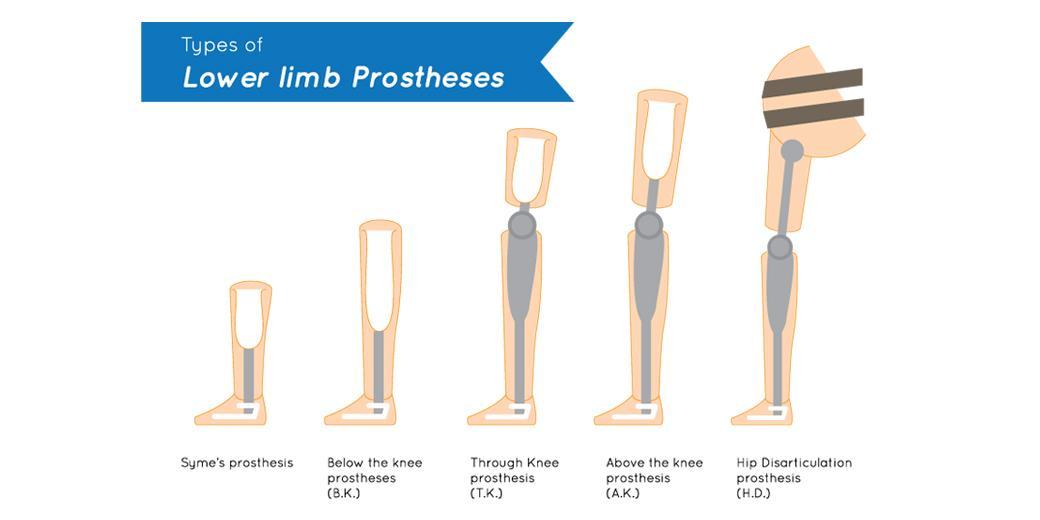
| Lower | Hemipelvectomy | Half of the pelvis and the entire lower extremity is removed |
| Lower | Hip disarticulation | The entire lower extremity is removed at the hip joint |
| Lower | Above knee (Transfemoral) | A portion of the lower extremity is removed above the knee but below the hip |
| Lower | Knee disarticulation | The lower portion of the lower extremity is removed at the knee joint |
| Lower | Below knee (Transtibial) | A portion of the lower extremity is removed below the knee but above the ankle |
| Lower | Complete tarsal | Removal of all tarsals, metatarsals, and phalanges (ankle, foot and toes) |
| Lower | Partial tarsal | Removal of metatarsals and phalanges (all or a portion of the foot and toes) |
| Lower | Complete phalanges | Removal of one or more toes |
Pain
Different pain syndromes can present after amputation. Each type of pain rarely exists in isolation and frequently contribute to one another.
1. Stump/Residual pain
2. Phantom limb pain
1. Stump Pain / Residual Pain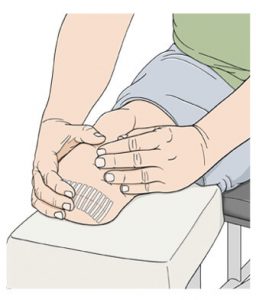
The immediate aftermath of limb amputation in the first postoperative days is dominated by surgical wound pain. This pain is readily identifiable and confined to the surgical site. Surgical stump pain is often described as sharp, aching, and severe. Acute stump pain would be expected to resolve in the first few weeks after amputation, however, ∼10% of patients will go on to experience persistent stump pain.
Causes of persistent stump pain
• Infection
• Wound breakdown
• Arterial insufficiency
• Osteomyelitis
• Bone spur
• Hematoma
• Stump neuroma
• Poorly fitting prosthesis
Stump neuroma – cause of residual pain
A neuroma is a collection, or bundle, of nerve endings that forms under the skin of your residual limb. Neuromas take time to develop and are not usually seen in the first few weeks after amputation. Features suggestive of neuroma formation include a focal point of pain at the stump, spontaneous pain, and localized sensory changes. It can become very sensitive, especially if the tangle is pressing against your prosthesis.
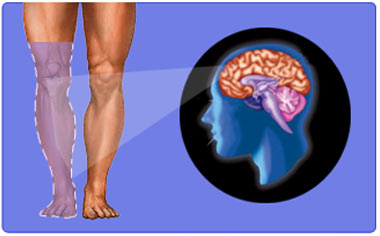
2. Phantom Limb Pain
Phantom limb pain is the most widely known post-amputation pain syndrome. Phantom limb pain is typically felt in the distal extremity of the absent limb. Pain characteristics vary but are often described as being cramping, burning, or shooting in nature. It is not uncommon to observe that if a patient experiences severe pain in a limb before operation then the same pain will be experienced after removal of that limb. Phantom pains are usually episodic occurring in short bouts ranging from a few seconds to many hours. It is the minority of patients who have severe and unremitting phantom pain.
Phantom Limb Pain vs Phantom Limb Sensation
• Phantom limb pain– pain or discomfort felt to be coming from the missing limb or body part
• Phantom limb sensation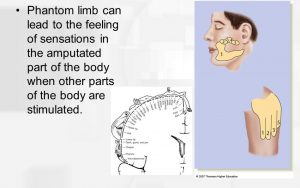 – sensation or perception of movement coming from the missing limb or body part.
– sensation or perception of movement coming from the missing limb or body part.
A phantom limb sensation is a non-painful perception of the continued presence of an amputated limb. Patients may report phenomenon from the missing limb such as tingling or itching. These non-painful phenomena are termed phantom sensations. The phantom limb may also be felt to be in a different position, shape or size to the missing limb.
This phase of treatment manages the healing process of the amputated limb, prepares the limb for prosthetic use, and helps the patient adapt to physical and emotional changes.
General considerations
1. Provide the patient with emotional support.
a. Depression due to loss of limb, decreased function, loss of work or leisure roles
b. Phantom limb sensation/ phantom limb sensation/ residual limb pain.
2. Manage hygiene and wound healing at the amputation site.
3. Desensitize limb to touch and pressure in preparation for prosthetic use.
4. Assist to shrink and shape limb in preparation for prosthetic use.
5. Special considerations apply when fitting prostheses for children with congenital deformities – please see separate chart.
| Treatment | Description | Example | Photo or Video |
| Educate patient in proper hygiene and skin care
|
Teach the patient to thoroughly wash and dry residual limb every day. Teach the patient how to inspect the skin for red areas, blisters or sores. | An occupational therapist teaches a man with a shoulder disarticulation amputation how to use a long, flexible handled mirror to check the skin integrity of the amputation site. | Hand held skin inspection mirror used to look for red areas or blisters in hard to reach spots. |
| Wound care
|
The use of debridement and modality techniques to prevent infection and promote healing of the surgical site. | For a patient with an above elbow amputation, an occupational therapist uses electrical stimulation techniques to promote circulation in the area surrounding the surgical site. | Video showing manual debridement of the surgical site two weeks after a below knee amputation. |
| Wrapping
|
Special elastic bandages are used to wrap the residual limb to reduce edema and shape the limb for the prosthetic socket. | For a woman with a below elbow amputation, an occupational therapist teaches the woman’s husband how to use an Ace bandage to wrap the stump to promote a tapered shape. | Wrapping technique for an above elbow amputation is demonstrated on a mannequin. |
| Elastic compression stump shrinker
|
An alternative to wrapping. The stump shrinker is a garment that slides on and off, made of elastic fabric that provides compression to the stump. | The same woman with the below elbow amputation opts to use an upper extremity compression stump shrinker as her husband cannot correctly wrap her stump without the occupational therapist’s help. | Compression stump shrinker for below knee or arm amputations. |
| Pain management and desensitization
|
Manual techniques to reduce pain and desensitize nerve endings at the amputation site. These techniques include the following: -tapping (also called percussion), involves tapping on sensitive areas to reset nerve endings -massage – both light and deep tissue massage using a variety of textures -vibration -fluidotherapy -weight bearing |
To reduce sensitivity, an occupational therapist applies 10 minutes of fluidotherapy to a man’s wrist disarticulation amputation site, followed with deep tissue massage. | An occupational therapist who has had a lower extremity amputation demonstrates desensitization techniques. |
| Mirror box therapy
|
A specialized technique for managing phantom limb pain. A box with a mirror down the middle is used to provide an image to the patient of the missing arm. The patient places both hands in the box and attempts to send signals to both hands. The process helps reduce phantom limb pain. | An occupational therapist has a patient with a below elbow amputation use a mirror box to attempt to pick up pennies with both hands. | Demonstration of the use of a mirror box for hand exercises. |
| Scar management
|
Treatment techniques to break up and flatten scar tissue at the surgical site, allowing a better prosthetic fit and reducing the risk of skin breakdown. Deep heat with modalities such as ultrasound, followed by scar massage, is used to treat scar tissue. | A woman has scar tissue build-up at the site of a traumatic thumb and first finger amputation. The occupational therapist uses ultrasound and scar massage techniques to soften the scar tissue. | An occupational therapist demonstrates scar massage and mobilization techniques |
| Range of motion
|
Passive and active range of motion exercises are used to prevent joint contracture and improve mobility near the amputation site. | An occupational therapist provides a home range of motion program for a man with a below elbow amputation to prevent elbow contracture. | |
| Strengthening
|
-Isometric exercises are used to strengthen the muscles that will be involved in operating a prosthesis. -Electrical stimulation to increase muscle contraction may be used to train the involved muscles prior to prosthesis use. -Isotonic and general endurance exercises are also provided to recondition the limb and the patient’s overall status after prolonged hospitalization. -Exercises may be adapted using cuff weights or an amputee cuff to compensate for a missing hand. |
An occupational therapist uses electrical stimulation to condition the shoulder girdle muscles of a man who has had a shoulder disarticulation amputation. | A man with an upper extremity amputation demonstrates the use of an amputee cuff for weight lifting. |
| Motor learning and muscle re-education | Therapeutic activities are used to teach upper extremity amputation patients how to incorporate the residual limb into bilateral activities. -If a patient has lost his dominant hand, motor learning activities are used to help the patient change hand dominance. -ADL activities are incorporated into motor learning tasks to apply new movements to functional tasks. -Biofeedback may be used to assist patients in learning to use muscle groups to operate prostheses. |
An occupational therapist teaches a man with a below elbow amputation of his dominant hand how to write with his non-dominant hand. | A woman with an above elbow upper extremity amputation uses biofeedback to train her muscles in preparation for prosthetic use. |
| Immediate post-op prosthesis (IPOP)
|
A semi-rigid plastic device that is fitted over the residual limb as soon as possible after amputation to reduce edema, prevent contractures and promote healing. | An occupational therapist has a man with a below elbow amputation reach for cones with his intact hand while bearing weight on the residual limb while wearing an IPOP. | Description of the initial rehabilitation process for upper extremity amputation patients, including a description of an IPOP. |
Body Powered – Body motion is used to apply tension on the control cable to activate the terminal device and elbow unit.
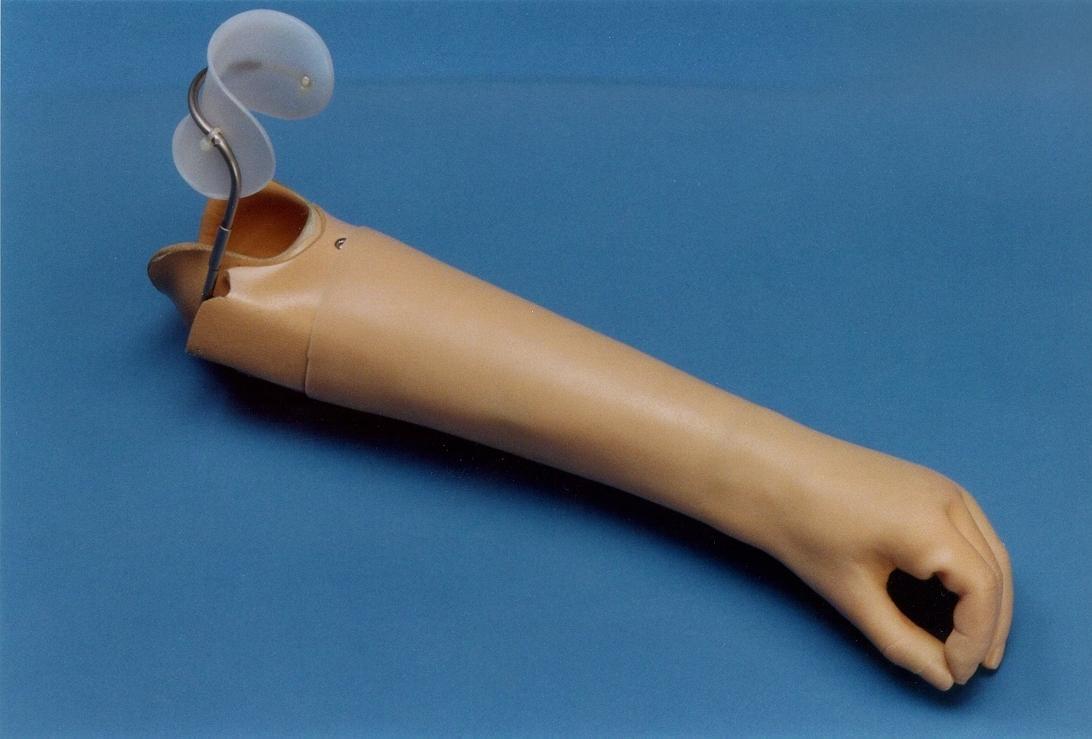
Cosmetic or Passive – has no functional parts and is made to look like the remaining limb as much as possible, including the color.

Myoelectric– uses EMG signals to activate electric components embedded inside the prosthetic socket that are in contact with the patient’s skin. The components pick up EMG signals as the muscles contract. The signals are amplified and relayed to the electrical terminal device, wrist unit, and/or elbow unit.
.
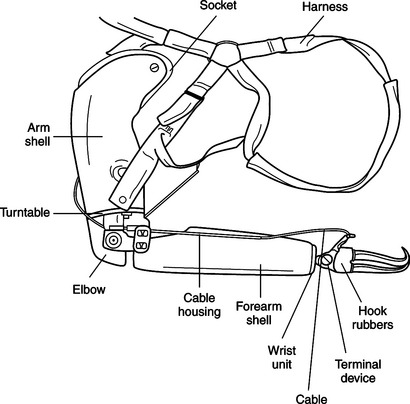
| Sockets – used to attach the prosthesis to the residual limb | Units – the body of the prosthesis | Terminal Devices – the device used to grasp and hold objects | Control Options – the way the prosthesis is operated |
| 1. Upper arm socket – encases and supports the residual limb. May have a harness or may be self supporting. 2. Forearm socket – encases and supports the residual limb. May have a harness or be self supporting. Design varies depending on the length of the residual limb...  |
1. Shoulder unit – places and positions an entire prosthetic arm. 2. Elbow unit and hinge – connects the socket to the upper arm with a triceps pad. Hinge is either flexible or rigid. May have an internal or external locking mechanism for positioning of the elbow. 3. Wrist unit – attaches the terminal device to the forearm socket. Designs vary. Can be pre-positioned...  |
1. Hook – more functional than a hand, less cosmetic. Provides better precision for small objects, better visual feedback, easier to maintain, weights less and costs less. -Voluntary opening hook – hook remains closed by a rubber band until tension on the cable causes the hook to open. Tension on the cable is created by body movement. -Voluntary closing – hook stays open until tension on the cable causes the device to close. Tension must be maintained to hold objects.2. Hand – more cosmetic, less functional than a hook. Can be voluntary opening or voluntary closing... .. ..  |
1. Body powered – operated by body motion.
2. Externally powered – activated by an external power source. 3. Hybrid – operated by a combination of body motion and external power. 4. Passive – cosmetic, for appearances only with no active movement. .. |
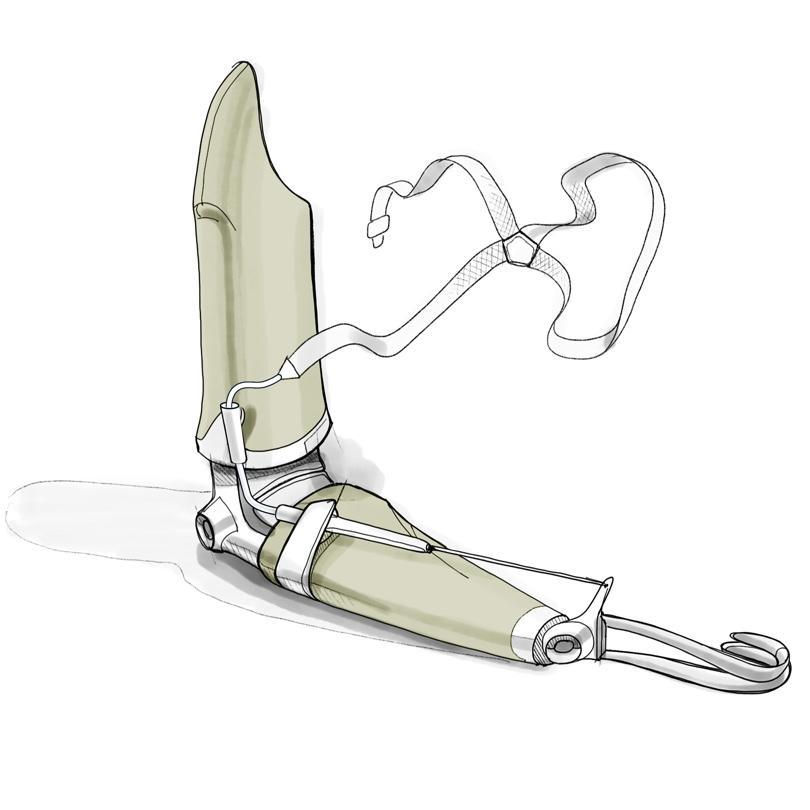
Pylon – the structure that attaches the socket to the terminal device. It may be basic, static, or dynamic.
Sock or gel liner – Device placed over the stump to fill the space in-between the stump and the socket and insure a tight fit.
Socket – the direct connection between the residual limb and the prosthesis.
Suspension system – the mechanism used to attach the socket to the residual limb. A variety of methods may be used, including belt straps, suction, and wedges.
Terminal device – the prosthetic foot, which provides a stable, weight-bearing surface and functions as a shock absorber.

Treatment Techniques – Prosthetic Phase
| Technique | Description | Example | Photo or Video |
| Patient Education | The patient is educated in the following areas: -the parts and functions of his or her prosthesis -how to don and doff the prosthesis -how to care for and maintain the prosthesis -hygiene and skin care for the residual limb |
An occupational therapist shows a woman with shoulder disarticulation amputation how to put on and fasten the shoulder unit for her prosthesis | Informative video explaining to patients how occupational therapists will help them select, use and care for a prosthesis. |
| Prosthetic Evaluation | The prosthesis is evaluated for the following: -compliance with prescription – is the prosthesis what was ordered? -comfort – observe how the prosthesis fits and check for pressure areas. -operation – make sure all components are operating correctly, including the cables and the terminal device -efficiency – check the control system efficiency, tension stability, and the ability of the terminal device to open and close with the elbow flexed in various positions. |
An occupational therapist has a man with an elbow disarticulation amputation lift a 10 pound weight with his prosthesis and checks how much displacement occurs at the socket. | Sample upper extremity prosthesis check-out form. |
| Prosthetic Training | Therapeutic activities and activities of daily living to train the patient in the operation of the prosthesis. -helps the patient develop tolerance for wearing the prosthesis. -application of prosthetic use to ADLs and IADLs is essential. |
An occupational therapist works with a child with a congenital upper extremity deformity to use his new above elbow prosthesis to pick up and place toy cars. | A four year old boy works with an occupational therapist on functional table top activities using his new myoelectric prosthesis. |
 ……
…… …….
……. 
| Age | Prosthetic Fitting | Terminal Device and Treatment | Example | Video |
| About 6 months | First fitting, when infant is able to sit independently. Fitting optional for infants with bilateral upper-limb amelia (absence of limb) or short transverse limb deficiencies (stubs). -infants without arms quickly learn to adapt using their feet. -effect of prosthetics on adapted development a consideration. |
No active controls, hook or cosmetic hand as terminal device. Training provided to parents and caregivers in application and use of prosthesis during normal play as well as care for prosthesis.
Infant should wear prosthesis at all times when awake except for bathing and swimming. Prosthesis removed when infant asleep. |
An infant wears a below elbow prosthesis while bearing weight on the affect limb to crawl. | A family talks about their experiences with upper extremity prosthetics for their daughter, including early first fitting. |
| About 2 years | Active terminal device introduced when toddler reaches certain developmental milestones:1. Able to follow simple 1-2 step directions. 2. Attention span of 10+ minutes. 3. Demonstrates awareness of terminal device. 4. Holds objects in terminal device and attempts to open it with other hand. 5. Displays interest in activities that requires use of 2 hands. 6. Able to cooperate with parent or therapist. |
Active terminal device, manual or myoelectric. -myoelectric preferred if funding is available. Active terminal device integrated into fine motor bilateral activities during play. Facilitation required by parents or therapist. Toddler may not cooperate with structured therapy. Alternate unstructured methods of terminal device use may be used instead. |
An occupational therapist teaches a 26 month old toddler to open the terminal device on her upper extremity prosthesis to pick up a plastic toy dish while playing. | A news story tells about a toddler who receives bilateral myoelectric upper extremity prostheses. |
| Preschool Age (2 1/2 to 4 years) | Adjustments for growth and terminal device settings | Treatment focused on grasp, release, and prehension using terminal device.-specific tasks used to learn grasp and release motions -learned movement incorporated into spontaneous play |
A four-year-old uses his terminal device to pick up and carry a toy hammer during pretend play. | A three year old boy demonstrates his new hand prosthesis, made from a 3-D printer. |
| 4 to 5 years | Adjustments for growth and terminal device settings. | Child trained in specific self help skills necessary for school. -opening a milk carton and snack containers or packages -holding paper -opening and closing glue and other bottles -donning and doffing prosthesis without help from an adult -managing outdoor clothing and clothing fasteners |
An occupational therapist teaches a four year old girl how to open her package of crackers using her functional hand and her terminal device. | A four year old boy works with an occupational therapist to learn school related tasks using his myoelectric prosthesis. |
| School Age – 5 years and up | Adjustments for growth, terminal device tension. Different terminal devices for different activities. | Regular therapy no longer necessary-children continue to practice skills to learn to adjust pressure on terminal device for strength of grasp
Children may need periodic training for specific activities, such as sports, arts and crafts, etc. |
A 7-year-old boy learns how to hold and swing a bat using his prosthesis during t-ball practice. | A girl demonstrates use of a myoelectric prosthesis during a variety of activities. |