This worksheet discusses the various aspects of swallowing, the definitions and causes of dysphagia, and various occupational therapy treatments for feeding disorders.
Anatomy of the Mouth and Throat
The anatomy of the mouth and throat plays a critical role in the swallowing process. Below is an overview of the key structures and their function during feeding:
| Structure | Description | Function During Eating |
| Oral Cavity | Hard and soft palate, tongue, cheeks, upper/lower jaw, teeth. | Contains food and drink and d performs initial mastication prior to swallowing. |
| Pharynx | Base of tongue, tendons, bone and muscles (buccinator, oropharynx, etc.). | Funnels food into the esophagus; shares space with the airway. |
| Larynx | Contains epiglottis, vocal cords. | Acts as a valve to close the airway during swallowing. |
| Trachea | Tube with cartilaginous rings located below the larynx. | Allows air into the lungs; closes during swallowing. |
| Esophagus | Thin muscular tube leading to the stomach. | Carries food from the pharynx to the stomach during swallowing. |
Oral Motor Skills During Eating
Eating involves using a range of oral motor skills that help prepare food and liquids for swallowing:
| Motor Skill | Description | Purpose |
| Sucking | Lips purse around a liquid source; inward suction pulls liquid into the mouth. | Used primarily by infants and for liquid intake. |
| Drinking | Controlled lip opening guides liquid from a cup into the oral cavity. | Becomes the main method of liquid intake after infancy. |
| Biting | Front teeth apply force to break food into smaller pieces. | Essential for taking manageable food pieces. |
| Chewing | Back teeth grind and soften food while saliva helps with digestion. | Prepares food for swallowing. |
Phases of Swallowing
Swallowing is a complex process that occurs in four distinct phases:
- Oral Preparatory Phase
- Food is chewed (mastication) and formed into a soft mass called a bolus.
- This is a voluntary phase and varies in duration based on food texture.
- Oral Phase
- The tongue pushes the bolus to the back of the mouth, triggering the swallowing reflex.
- This is a voluntary phase; typically lasts 1-3 seconds.
- Pharyngeal Phase
- The swallow reflex is initiated, and the larynx closes to protect the airway.
- This phase is involuntary and takes about 1-3 seconds.
- Esophageal Phase
- The esophagus contracts to move the bolus toward the stomach.
- This phase is involuntary; lasts 8-10 seconds.
What is Dysphagia?
Dysphagia refers to difficulty or discomfort in swallowing that persists over a prolonged period of time. It can impact an individual’s ability to eat safely, which may lead to malnutrition or aspiration.
2 Types of Dysphagia
| Type | Some of the common Symptoms | Causes |
| Esophageal | – pain when swallowing– the sensation of food sticking in the throat– regurgitation– frequent heartburn | – GERD, esophageal strictures, tumors |
| Oropharyngeal | – coughing or gagging when swallowing– drooling– sudden weight loss– inability to swallow | – Neurological diseases (e.g., stroke, Parkinson’s) |

Dysphagia Diet: Framework for Dysphagia Management
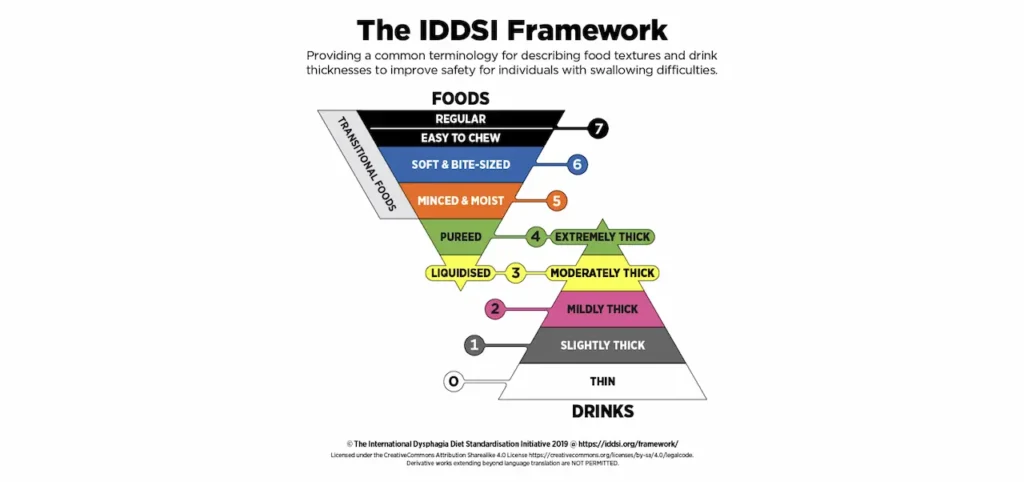
Patients with dysphagia may require modified diets to make eating and drinking safer. Liquids and foods are often thickened or altered in texture to prevent choking and aspiration.
Liquid Consistencies
| Consistency | Description | Examples | |
| Thin | Normal liquid that flows freely. | Water, tea, juice. |  |
| Nectar | Slightly thickened to slow flow. | Tomato juice, smoothies. |  |
| Honey | Moderately thick; drips slowly. | Honey, syrup. |  |
| Pudding | Extremely thick; does not drip or flow. | Pudding, ice cream |  |
Food Consistencies
| Level | Description | Examples | |
| Level 4 | Pureed; pudding-like texture. | Mashed potatoes, applesauce. |  |
| Level 5 | Mechanical soft; easy-to-mash, soft foods. | Ground meat, mashed veggies. |  |
| Level 6 | Soft solid foods, cut into small pieces. | Soft fruits, diced chicken. |  |
| Level 7 | Regular; normal food that requires chewing. | Normal diet. |  |
Occupational Therapy Treatments for Dysphagia
Occupational Therapy Practitioners (OTPs) play a key role in addressing feeding and swallowing issues by implementing interventions tailored to the patient’s individual needs.
General Feeding Guidelines:
- Ensure all dietary restrictions and food consistencies are followed.
- Check food temperature before serving.
- Seat patients in a proper seated position to encourage safe feeding.
- Make sure the patient is alert and prepared to eat.
Examples of OT Interventions:
| Problem | Examples of Intervention |
| Poor postural control | Upright positioning with supports for pelvis, head and spine. |
| Weak lip closure | Oral-motor exercises e.g.activities like blowing bubbles. |
| Tongue thrust | Facilitate tongue retraction by pressing the bowl of the spoon on the middle of the tongue before withdrawing it from the mouth. |
| Misaligned or weak bite | Use of chew tubes and handling techniques for alignment. |
| Oral sensory issues | Present new food items one at a time in a fun, non-threatening manner. |
Final Thoughts
Dysphagia can significantly impact daily life, but with a structured approach and support from OTPs, feeding and swallowing challenges can be managed effectively. Modifying food textures, positioning, and implementing specific oral-motor and swallowing exercises can greatly enhance a patient’s ability to eat safely and independently.Liquid Consistencies
For those experiencing ongoing difficulties with swallowing, it is essential to consult a physician and with a team approach, which includes OTPs and speech-language pathologists, the best course of action can be determined.
What are the key structures involved in swallowing?
Key structures involved in swallowing include the oral cavity, pharynx, larynx, trachea, and esophagus. Each plays a crucial role during the process of eating and swallowing.
What are the four phases of swallowing?
The four phases of swallowing are: the Oral Preparatory Phase, Oral Phase, Pharyngeal Phase, and Esophageal Phase. These phases ensure that food is effectively moved from the mouth to the stomach.
What is dysphagia and what types exist?
Dysphagia is a condition where individuals have difficulty swallowing, posing risks for malnutrition and aspiration. It is categorized into Esophageal Dysphagia, often due to conditions like GERD, and Oropharyngeal Dysphagia, which typically arises from neurological issues such as a stroke.
How are liquid and food consistencies categorized in dysphagia diets?
Liquid consistencies are categorized as thin, nectar, honey, and pudding-like. Food consistencies are classified from Level 4 (pureed foods) to Level 7 (regular diet). These modifications help manage dysphagia safely.
What occupational therapy treatments are available for dysphagia?
OT interventions for dysphagia include ensuring dietary restrictions are followed, maintaining the proper seating posture, and engaging oral-motor exercises. Interventions aim to improve swallowing safety and effectiveness.



