A Spinal Cord Injury (SCI) is a serious event that markedly affects a person’s sensory, motor, and autonomic systems, leading to challenges such as pain, fatigue, depression, and anxiety. Achieving independence depends on the severity of the injury, personal capabilities, and the utilization of technology.
Grading SCI: Understanding the ASIA Scale
SCIs are graded using the American Spinal Injury Association (ASIA) scale:
- ASIA A: Complete injury with no sensory or motor function.
- ASIA B: Sensory incomplete with no motor function.
- ASIA C: Motor incomplete with some anti-gravity movement.
- ASIA D: Motor incomplete with more than half of muscle groups being anti-gravity.
- ASIA E: Normal function.
In our full guide, we break down each grade with real-world examples to help you understand these distinctions clearly.
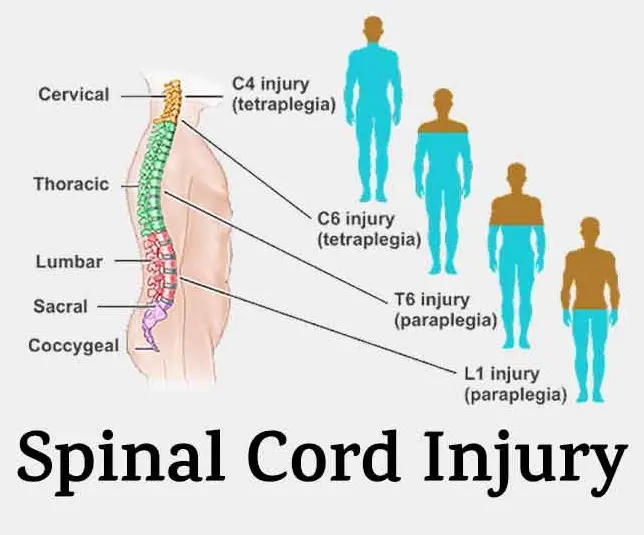
Spinal Cord Injury Levels and Functions
Understanding spinal cord injury levels is crucial for determining the function and independence potential:
Cervical Levels: SCI Mnemonic
Use this mnemonic to remember functions related to cervical levels:
- C1-C3: “I turn my head so I can see” – Head and neck movement limitation.
- C4: “Breathe more, shrug my shoulders to ignore” – Increased control over neck and shoulder movement.
- C5: “Arms up high, bend my elbows, pretend to fly” – Adds elbow flexion.
- C6: “Pick up sticks, tenodesis helps me exist” – Enhanced wrist extension.
- C7: “I’m in heaven, transfer myself, independent livin’” – Elbow extension adds independence.
- C8: “This is great – now my thumb can manipulate” – Greater hand function.
C6 Spinal Cord Injury: Functions and Independence
At C6, individuals have movement in their head, neck, shoulders, arms, and wrists. They can engage in:
- Self-feeding with adaptive equipment.
- Upper body dressing independently; require help for lower body.
- Independence in bed mobility and transfers with support.
Practice task-oriented group activities weekly to enhance skills needed at this level.
Action Steps for C6 Injury
- Implement daily pressure relief techniques.
- Enhance mobility techniques; use of adaptive devices.
T1-T12 Spinal Cord Injury Levels and Function Chart
These levels contribute to core stability and function:
- T1-T6: Advanced use of trunk muscles for stability without support.
- T7-T12: Increased core function enhances walking capabilities.
L1-L5: Lower Limb Functionality with Spinal Cord Injuries
The L1 to L5 levels support significant lower body functions, crucial for walking and hip and knee movements.
- Practice balancing techniques frequently to adjust to these new motor capabilities.
Additional Resources
For a detailed overview, including interactive quizzes and scenarios, consider our 5-day risk-free trial program for accessing the comprehensive study materials.
Want detailed practice tips to ace the NBCOT® exam? Join now for full access!
What is a Spinal Cord Injury (SCI)?
A Spinal Cord Injury (SCI) is a serious condition that affects a person’s sensory, motor, and autonomic functions, often resulting in challenges like pain, fatigue, depression, and anxiety. The impact and recovery depend on the injury’s severity and the use of assistive technology.
How are Spinal Cord Injuries graded using the ASIA scale?
The American Spinal Injury Association (ASIA) scale grades SCIs as follows: ASIA A for complete injury with no sensory or motor function, ASIA B for sensory incomplete with no motor function, ASIA C for motor incomplete with some anti-gravity movement, ASIA D for more motor function than half of muscle groups can move against gravity, and ASIA E for normal function.
What are the potential functional capabilities at the C6 level of a spinal cord injury?
Individuals with a C6 spinal cord injury can utilize their head, neck, shoulders, arms, and wrists. They can perform self-feeding and upper body dressing with adaptive equipment, are independent in bed mobility, and can complete transfers with some support.
What are the core and functional capabilities at T1-T12 spinal cord injury levels?
T1-T12 spinal cord injury levels primarily influence core stability. T1-T6 levels enable trunk muscle use for stability without extra support, while T7-T12 levels enhance core function that can improve walking capabilities.
Where can I find additional resources for learning about spinal cord injury functions?
For detailed guidance, interactive quizzes, and scenarios on spinal cord injuries, check the additional resources section provided. It offers comprehensive study materials that can aid in preparing for exams like the NBCOT®.