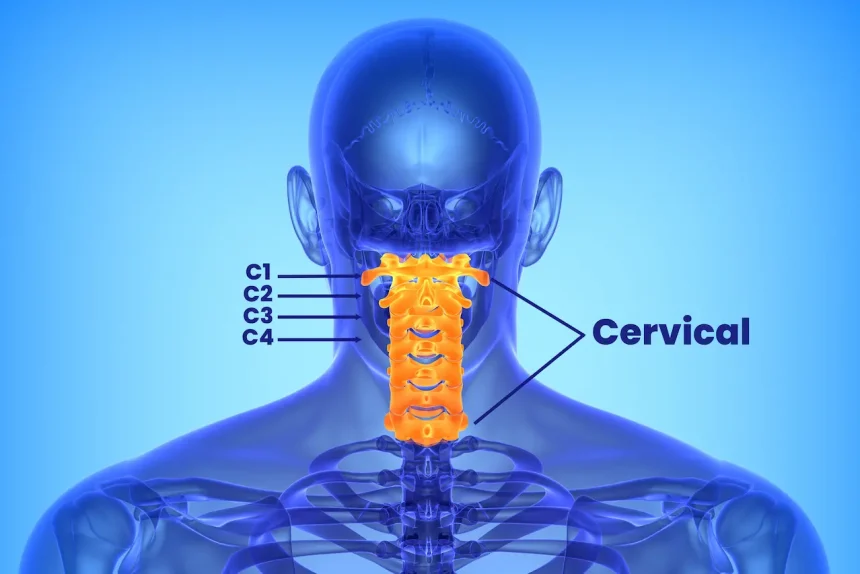
Discover the intricacies of managing a complete C1–3 spinal cord injury (SCI), and how it affects speech, swallowing, breathing, and mobility.
Sip and Puff Ventilation
Understanding High Level Tetraplegic injuries can be life-changing, especially when it includes ventilation support through methods such as sip and puff systems.
- Patients with C1-C3 injuries often rely on long-term mechanical ventilation due to diaphragm innervation loss.
- Functional electrical stimulation (FES) might reduce ventilatory needs if there’s intact motor innervation.
Practice Tip: Can you explain how the sip and puff ventilator works with tracheostomy?
What is Tetraplegic?
Tetraplegia refers to a condition where there is a partial or complete paralysis affecting the four limbs and torso, generally caused by a neck injury.
High level tetraplegics retain certain muscle functions:
- Sternocleidomastoid: Neck rotation and flexion
- Cervical paraspinal muscles: Neck extension
- Neck accessory muscles: Assist with speech and swallowing
Sip N Puff Wheelchair Control
Alternative mobility solutions like the sip n puff wheelchair offer tetraplegics a way to navigate their environment safely and independently.
- Control wheelchairs by inhaling or exhaling into a pneumatic tube.
- Head, chin, speech, and tongue-operated controls are alternatives based on individual capabilities.
Study Method: Consider setting up weekly practice sessions with sip and puff devices to test your knowledge and skills.
Diaphragm Spinal Cord Level
Understanding the spinal cord levels for diaphragm innervation is crucial for assessing ventilator support needs.
When compromised, as in high-level SCI, it necessitates ventilatory assistance, potentially through innovative approaches like FES or sip and puff ventilators.
Spell Trach Correctly – Tips and Tricks
For medical students and professionals, spelling and understanding terms like “tracheostomy” (often abbreviated to “trach”) is essential.
Sip and Puff Power Wheelchair for Improved Mobility
Sip and puff systems can empower tetraplegics, enhancing their independence by facilitating easy wheelchair control.
Utilize our quizzes to test your knowledge on modern assistive technologies in the full instructional guide.
Want detailed practice tips to ace the NBCOT® exam? Join now for full access!
What are the key challenges of managing high level tetraplegia?
Managing high level tetraplegia, especially with C1-C3 spinal cord injuries, involves addressing issues such as speech, swallowing, breathing, and mobility, often requiring mechanical ventilation and assistive devices like sip and puff systems.
How does a sip and puff ventilator work with a tracheostomy?
A sip and puff ventilator is operated by inhaling or exhaling into a tube, which can control the ventilator that is connected via a tracheostomy. This allows individuals with diaphragm paralysis to manage their breathing effectively.
What are some alternative mobility solutions for tetraplegics?
Besides the sip and puff systems, tetraplegics can use head, chin, speech, or tongue-operated controls for wheelchairs to navigate their environment independently. Each system is chosen based on the individual’s specific capabilities.
How does high level tetraplegia affect diaphragm functionality?
High level tetraplegia, such as complete C1-C3 injuries, often disrupts diaphragm innervation, necessitating ventilatory support. Innovations like functional electrical stimulation (FES) or sip and puff ventilators can assist in compensating for this loss.
What muscle functions are retained with high level tetraplegia?
Individuals with high level tetraplegia typically retain some muscle functions, such as neck rotation and flexion via the sternocleidomastoid, neck extension with cervical paraspinal muscles, and speech and swallowing assistance from neck accessory muscles.