Understanding burns and their rehabilitation is crucial for aspiring occupational therapists, especially those preparing for the NBCOT® exam. Burns vary in type and severity, and each type requires specific management and rehabilitation strategies.
Burn Stages: Levels of Burns
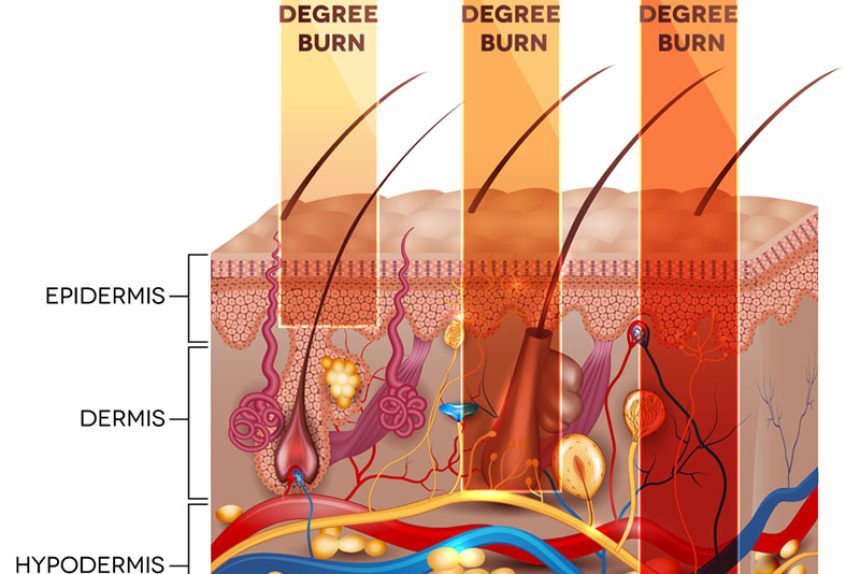
Burns are classified into stages based on their severity and impact on the skin layers:
- First Degree: Affects only the epidermis, causing red, painful skin without blistering. These superficial burns heal within 3-4 days.
- Second Degree: Extends into the dermis. Superficial partial thickness burns are pink and painful, healing in 7-21 days. Deep partial thickness burns change skin color and may require scar management, healing in 3-5 weeks.
- Third Degree: Full thickness burns that extend through all skin layers, often requiring surgery.
- Fourth Degree: Burns penetrate to fat, muscle, and bone, often needing amputation.
Stages of Burns: Phases of Wound Healing
Burns heal through distinct phases:
- Inflammatory Phase: Lasts from injury onset to 3-10 days, characterized by pain, redness, and edema.
- Proliferation Phase: From day three to wound closure, involves scar formation and tissue revascularization.
- Maturation Phase: Occurs from three weeks to over two years post-injury, with scar remodeling and increased tensile strength.
For in-depth understanding, our full guide discusses each wound healing stage alongside case examples and quizzes.
Burn Treatments and Phases
Each burn stage demands specific medical and rehabilitative care:
- Emergent Phase: Begins at injury and focuses on stabilizing vital functions and preventing infection.
- Resuscitative Phase: Manages fluid replacement and shock prevention.
- Acute Phase: Covers wound closure, infection prevention, and maintaining skin and joint mobility.
- Rehabilitative Phase: Aims to restore maximum function through scar management and muscle strengthening.
For more detailed practice tips and full access to our resources, join us today.
Medical Management: Emergent Phase of Burn
The initial response is critical for successful burn rehabilitation. Immediate actions include:
- Stopping the burning process and protecting the wound
- Preventing shock and preserving organ function
Going beyond basics, our full guide explores real-world scenarios encountered in different burn treatment phases.
Occupational Therapy Interventions
Therapy varies depending on burn severity and involves:
- Second Degree Burns Treatment: Includes wound care, edema management, range-of-motion exercises, and ADL training.
- Third Degree Burns Rehabilitation: Involves surgery, structured rehabilitation, and adaptive strategies for daily activities.
Case studies and mock evaluations are available to support your preparation for the NBCOT® exam.
Interactive Question:
Can you identify key differences in rehabilitation strategies between second and third-degree burns?
Looking to excel in the NBCOT® exam with comprehensive strategies and tools? Join now for full access!
What are the different degrees of burns, and how do they affect the skin?
Burns are classified into four degrees. First-degree burns affect only the epidermis, causing redness and pain. Second-degree burns extend into the dermis, with superficial partial thickness burns healing in 7-21 days and deep partial thickness burns taking 3-5 weeks. Third-degree burns are full-thickness, affecting all skin layers and often requiring surgery. Fourth-degree burns extend to fat, muscle, and bone, sometimes needing amputation.
How do the phases of burn wound healing progress?
Burn wound healing occurs in three phases: the inflammatory phase (3-10 days), the proliferation phase (from day three to wound closure), and the maturation phase (three weeks to over two years). These phases involve processes such as pain management, scar formation, tissue revascularization, and scar remodeling.
What are the key medical management steps during the emergent phase of burns?
During the emergent phase, immediate actions focus on stopping the burning process, protecting the wound, preventing shock, and preserving vital organ function. This phase is critical to the overall success of burn rehabilitation.
How do rehabilitation strategies differ between second and third-degree burns?
Second-degree burns rehabilitation includes wound care, edema management, and range-of-motion exercises, focusing on recovery and ADL training. Third-degree burns require more intensive treatment like surgery, structured rehabilitation, and adaptive strategies for daily activities due to the extent of injury and tissue damage.
What occupational therapy interventions are utilized for burn rehabilitation?
Occupational therapy interventions vary by burn severity. For second-degree burns, interventions include wound care and ADL training. For third-degree burns, they involve surgical recovery support, mobility enhancement, and adaptive strategies to assist with daily life activities.