
Neural tube defects, such as spina bifida, are common congenital anomalies believed to result from a combination of genetic and environmental factors. These defects occur when the neural tube fails to close completely during early pregnancy.
Understanding Spina Bifida: Key Types and Characteristics
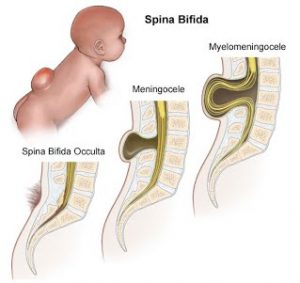
Spina bifida, literally meaning “cleft spine,” can result in the incomplete development of the brain, spinal cord, and/or meninges. The condition may affect any spinal vertebra but is prevalent in the caudal lumbar and sacral regions. It varies based on localization, coverage, and neural involvement.
Types of Spina Bifida: A Closer Look
Spina bifida is classified into several types, ranging in severity and characteristics:
- Occulta: Known as the “hidden” type; it involves a slight defect in one or more vertebrae, typically with no visible symptoms.
- Closed Neural Tube Defects: Includes conditions like lipomyelomeningocele where the spinal cord is entangled in a fatty tumor, often causing symptoms like back and leg pain.
- Meningocele: The least common type, presenting potential complications such as partial paralysis due to spinal fluid and meninges protrusion.
- Myelomeningocele (SBM): The most severe form where the spinal cord is exposed, generally leading to paralysis and significant loss of sensation.
Risk Factors: What Increases the Likelihood of Neural Tube Defects?
The precise cause of spina bifida hasn’t been definitively identified, but several factors can increase the risk:
- Genetic predisposition
- Exposure to hazardous chemicals
- Insufficient intake of essential vitamins like folic acid
- Infection, prescription drug, and alcohol use during pregnancy
- Maternal age, socioeconomic status, and birth order
Ensuring an adequate intake of folic acid, found in green leafy vegetables and fortified cereals, can significantly decrease the risk.
Open Neural Tube Defect Screening
Screening for open neural tube defects, such as spina bifida cystica, can often occur during pregnancy. Early detection is crucial in managing the disorder effectively. Regular prenatal visits and diagnostic tests can help anticipate and manage potential complications.
Clinical Features of Spinal Bifida
Understanding the clinical features of spina bifida is essential for identifying potential challenges and planning interventions:
- Motor Dysfunction: Commonly includes muscle weakness, paralysis, and loss of sensation below the malformation.
- Sensory Impairment: Difficulties in sensory processing can necessitate reliance on other senses like vision.
- Orthopedic Issues: Such as scoliosis, foot, and leg deformities resulting from muscle imbalances and neurological complications.
- Additional Concerns: Include Chiari malformations, bowel and bladder dysfunction, hydrocephalus, and tethered spinal cord which may require lifelong management.
Spina Bifida Occupational Therapy: Essential Intervention Strategies
Occupational therapy plays a crucial role in supporting individuals with spina bifida, focusing on enhancing independence and managing complications. Key interventions may involve:
- Customized exercises to improve motor function and coordination
- Adaptive techniques to facilitate daily activities and promote autonomy
- Sensory integration strategies to manage sensory processing issues
Want detailed practice tips to ace the NBCOT® exam? Join now for full access!
What is Spina Bifida and how does it affect the body?
Spina Bifida is a neural tube defect that results in the incomplete development of the spine’s vertebrae, brain, and/or meninges. It commonly affects the caudal lumbar and sacral regions, potentially resulting in motor dysfunction, paralysis, sensory impairment, and additional complications like Chiari malformations.
What are the different types of Spina Bifida?
Spina Bifida is classified into types including Occulta, Closed Neural Tube Defects, Meningocele, and Myelomeningocele (SBM). These types vary in severity; for example, Occulta is the mildest with no visible symptoms, while Myelomeningocele is the most severe and often leads to paralysis.
What are the risk factors for developing Spina Bifida?
Risk factors for Spina Bifida include genetic predisposition, exposure to hazardous chemicals, insufficient intake of vitamins like folic acid, and factors related to maternal health, such as age and socioeconomic status. Adequate folic acid intake can significantly lower the risk.
How can Spina Bifida be detected during pregnancy?
Spina Bifida can often be detected during pregnancy through screening for open neural tube defects, such as spina bifida cystica. Regular prenatal visits and diagnostic tests are essential for early detection and management of the disorder’s potential complications.
What role does occupational therapy play in the management of Spina Bifida?
Occupational therapy is vital for individuals with Spina Bifida, focusing on enhancing independence and managing complications. It involves customized exercises to improve motor function, adaptive techniques for daily activities, and sensory integration strategies to manage sensory processing issues.



