SPINA BIFIDA

Neural tube defects are one of the most common birth defects and are thought to have multifactorial etiology, including multi-genetic and environmental influences. The neural tube closes 28 to 32 days after conception at a time before many women are aware, they are pregnant.
Risk Factors
Normal development of the brain and spinal cord may be affected during these first 3 to 8 weeks of pregnancy by the following:
• Genetic factors
• Exposure to hazardous chemicals and other substances
• Lack of proper vitamins (folic acid) and nutrients in the diet
• Infection
• Prescription drug and alcohol consumption
• Maternal age. Spina bifida is more commonly seen in teenage mothers
• History of miscarriage
• Birth order. First-born infants are at higher risk
• Socioeconomic status. Children born into lower socioeconomic families are at higher risk for developing spina bifida. It is thought that a poor diet, lacking essential vitamins and minerals, may be a contributing factor
** Folic acid (vitamin B-9), a nutrient found in some green, leafy vegetables, nuts, beans, citrus fruits, and fortified breakfast cereals, can help reduce the risk of neural tube defects.
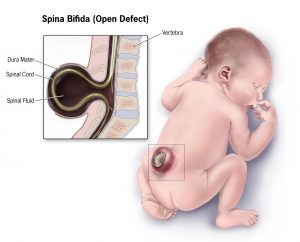
Spina Bifida (SB), which literally means “cleft spine,” is characterized by the incomplete development of the brain, spinal cord, and/or meninges, and is classified as a defect of the neural tube.
In babies with SB, a portion of the neural tube doesn’t close or develop properly, causing defects in the spinal cord and in the vertebrae. SB may affect any vertebra but is most common in the caudal lumbar and sacral areas. SB’s impact is determined by the size and location of the malformation, whether it is covered, and which spinal nerves are involved. All nerves located below the malformation are affected to some degree. Therefore, the higher the malformation occurs on the spine, the greater the amount of nerve damage and loss of muscle function and sensation.
Although the spinal opening can be surgically repaired shortly after birth, the nerve damage is permanent, resulting in varying degrees of paralysis of the lower limbs. Even when there is no lesion present there may be improperly formed or missing vertebrae and accompanying nerve damage.
2 Types of Neural Tube Defects
1. Closed
2. Open / Spina Bifida Cystica
Closed Neural Tube Defects
• Localized and confined to the spine; brain rarely affected
• Development of the spinal cord is affected by malformations of the fat, bone, or meninges.
• Neural tissue not exposed; spinal defect fully covered by skin. The skin covering the defect may be dysplastic (i.e., tuft of hair, dimple, birthmark, or other superficial abnormality).
• May remain undetected for years, especially in absence of cutaneous markers.
Sub-types: SB Occulta, Lipomyelomeningocele, Lipomeningocele
Open Neural Tube Defects
• Involves the entire CNS
• Neural tissue exposed with associated CSF leakage
• Skin covering not intact
• Visible at birth; majority discovered during pregnancy
Sub-types: Meningocele, Myelomeningocele
| TYPE | DESCRIPTION | SYMPTOMS | PICTURE |
| Occulta | Mildest form– “occulta” means “hidden”. One or more vertebrae has a slight defect which is covered by skin and there is no protrusion of the spinal cord. | Most people with spina bifida occulta are almost always completely asymptomatic. Most people are not even aware that they have spina bifida occulta, unless it is discovered on an x-ray performed for an unrelated reason Occasionally, spina bifida occulta does cause symptoms. This usually occurs when the defect is more extensive, for example, if it involves more than one vertebra. This can lead to neurological deficits such as bowel or bladder dysfunction, back pain, leg weakness. |
|
| Closed Neural Tube Defects
Example: Lipomyelomeningocele |
Lipomyelomeningocele is a closed spinal lesion in which part of the spinal cord and nerves are tangled in a benign fatty tumor. | Problems associated with lipomyelomeningocele are caused by the spinal cord and nerves being trapped within the fatty lump, and the lump putting pressure on the spinal nerves. Initially may have no symptoms but symptoms then start to develop, usually as a result of a tethered spinal cord, and may include problems with bowel and bladder function, frequent urinary tract infections, spasticity, back and leg pain, weakness, and sensory loss. |
|
| Meningocele | Rarest type of spina bifida. Spinal fluid and meninges protrude through an abnormal vertebral opening; the malformation contains no neural elements and may or may not be covered by a layer of skin. |
Usually no resultant paralysis. Some babies have few or no symptoms, while others experience complications, such as partial paralysis and urinary and bowel dysfunction. |  |
| Myelomeningocele
(SBM) |
Most severe form. Occurs when abnormally developed spinal cord tissue is exposed through the opening in the spine.In most cases, there is no layer of skin covering the sac. |
The exposed spinal cord is damaged by the fluid in the womb during pregnancy and may also not develop properly. As a result, there is nearly always some resulting paralysis and loss of sensation. The extent of deficits can be patchy and difficult to predict.
Can expect: Muscle weakness or paralysis below the level of the defect. Loss of sensation and an inability to control bladder or bowel function. Additionally, CSF may build up in the brain, leading to hydrocephalus, which is common in children with myelomeningocele. If left untreated, hydrocephalus can cause brain damage, blindness or seizures. |
|
As outlined in the table above, symptoms can range from minor physical problems with little functional impairment to severe physical and intellectual disabilities.
Clinical manifestations associated with Spina Bifida Myelomeningocele (SBM)
The most obvious clinical manifestation of myelomeningocele is the loss of sensory and motor functions in the lower limbs.
• Sensory impairment
Impaired sensation below the level of the lesion. Sensory loss includes kinesthetic, proprioceptive, and somatosensory information. As a result, children will often have to rely heavily on vision and other sensory systems to compensate.
• Weakness and paralysis
Upper limb function, as well as lower limb function, is impaired in two thirds of children with SBM.
Upper limb motor deficits in SBM include strength, hand and finger dexterity, speed, motor planning, and bimanual coordination. Poor hand function and the inability to coordinate eye and hand movements may interfere with ADLs, such as buttoning a shirt or opening a lunchbox.
At birth, two main types of motor dysfunction in the lower extremities have been identified.
I. The first type involves a complete loss of function below the level of the lesion, resulting in a flaccid paralysis, loss of sensation, and absent reflexes. Orthopedic deformities may result from the unopposed action of muscles above the level of the lesion. This unopposed pull commonly leads to hip flexion, knee extension, and ankle dorsiflexion contractures.
II. When the spinal cord remains intact below the level of the lesion, the effect is an area of flaccid paralysis immediately below the lesion and possible hyperactive spinal reflexes distal to that area. Neurological involvement again results in orthopedic deformities, depending on the level of the lesion, the spasticity present, and the muscle groups involved.
• Orthopedic deformities
The orthopedic problems that occur with myelomeningocele may be the result of the imbalance between muscle groups; the effects of posture, and gravity; and associated congenital malformations. Decreased sensation and neurological complications also may lead to orthopedic abnormalities. Scoliosis, hip, foot, and leg deformities are common.
• Type 2 Chiari malformation
Most babies with SBM are born with a Chiari malformation (Type II), in which brain tissue extends into the spinal canal. This condition can lead to compression of the spinal cord and cause a variety of symptoms including difficulties with feeding, swallowing, and breathing. Other symptoms may include weakness in the upper limbs.
• Bowel and bladder dysfunction.
The most common bladder and bowel problems are inability to voluntarily relax the sphincters. Besides various forms of incontinence, incomplete emptying of the bladder remains a constant concern because infection of the urinary tract and possible kidney damage may result.
• Hydrocephalus is another common residual problem, affecting most children with SBM. Without treatment, this can cause neurological problems or intellectual disabilities. Hydrocephalus often recurs gradually after treatment.
• Tethered Spinal Cord
Tethered spinal cord is defined as a pathological fixation of the spinal cord in an abnormal caudal location. This fixation produces mechanical stretch, distortion, and ischemia with daily activities, growth, and development. This can cause foot or leg deformities, hip dislocation, or scoliosis. As the spine lengthens, the spinal cord stretches out, damaging spinal cord tissue and restricting blood supply to the nerves. The problems can worsen as the child grows and the tethered cord is stretched. Over time, usually months or years, a tethered spinal cord can reduce sensitivity in the legs, bladder, or bowel.
• Pathologic bone fractures
This occur in a significant percentage of children with SBM. A pathologic fracture is a break that occurs because of weakness or disease in the bones, not solely because of injury. Because the paralyzed limbs of the child with spina bifida have increased amounts of unmineralized osteoid tissue, they are prone to fractures,
• Growth and nutrition
Growth hormone deficiency results in short stature. Early on, infants may have feeding issues as a result of an impaired gag reflex, swallowing difficulties, and a high incidence of aspiration. Altered oral-motor function has been attributed to the Chiari II malformation. These impairments may lead to nutritional issues and delayed growth and weight gain. Conversely, obesity can be a significant issue. Mobility limitations and decreased energy expenditure result in lower physical activity levels.
• Cognitive impairment and learning issues
Although children with SBM without hydrocephalus may have normal intellectual potential, children with hydrocephalus, are likely to have below-average intelligence. These children often demonstrate learning disabilities and poor academic achievement. Even those with a normal IQ show moderate to severe visual-motor perceptual deficits. The impairment of intellectual and perceptual abilities has been linked to damage to the white matter caused by ventricular enlargement. This damage could account for the often severe perceptual-cognitive deficits that is evident. Tasks and skills affected include memory, reasoning, math, handwriting, organization, problem solving, attention, sensory integration, auditory processing, visual perception, and sequencing.
• Latex Allergy or Sensitivity
Allergy to latex is very common. This is thought to be a result of intense exposure to latex in the early years of life because of frequent surgeries and other medical procedures. An allergic reaction to latex can be life threatening.
• Risk for pressure sores
The presence of paralysis and lack of sensation on the skin places the child with spina bifida at major risk for pressure sores and decreased skin integrity.
• Psychological, social, and sexual problems occur more often in people with SBM than in the general population.
Resources:
https://www.ninds.nih.gov/disorders/patient-caregiver-education/fact-sheets/spina-bifida-fact-sheet
https://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Spina-Bifida
https://www.columbiaspine.org/condition/spina-bifida-occulta/
https://emedicine.medscape.com/article/1825866-treatment
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3075008/
https://clinicalgate.com/spina-bifida-a-congenital-spinal-cord-injury/
https://www.ucsfbenioffchildrens.org/conditions/spina_bifida/signs_and_symptoms.html
https://www.orthobullets.com/pediatrics/4085/myelodysplasia-myelomeningocele-spinal-bifida