OT Process and Intervention
………….. .. ….
Occupational Therapy Process

The provision of occupational therapy services follows a specific sequence of
steps.
| Step in the Process | Description | Who is Involved | Points to Consider |
| Altruism | Patients are referred to occupational therapy by a variety of sources, including family members, caregivers, physicians, health care centers, employers, etc. –Occupational therapists cannot work with any patient because the patient may have a therapeutic need; patients must be referred. –The rules and regulations regarding occupational therapy referrals vary from state to state. |
Anyone can refer a patient to occupational therapy, including the patient. Occupational therapy services cannot be provided, however, without an evaluation. A prescription, also called an order, for an evaluation must be issued by the patient’s physician (including medical doctor, doctor of osteopathy, psychiatrist, or other holding a medical degree), nurse practitioner (subject to state law), chiropractor, or dentist.
–Physician’s orders for occupational therapy are required in most states and by most insurance providers. |
Therapists can also refer to other therapeutic practitioners. -Visual acuity issues=refer to the optometrist -Eye disorders= refer to the ophthalmologist -Not following dietary recommendations=refer to the dietician -Speech delay=refer to the speech language pathologist -Gait disorders=refer to the physical therapist.A referral can be very specific such as asking for a neoprene splint or general by asking to test for a developmental delay. |
| Screening | After the referral, the occupational therapist needs to screen the patient in order to determine if an evaluation is needed. A screening is used to obtain preliminary information of the patient’s situation. | The occupational therapist oroccupational therapy assistant may complete observation of the patient, checklists, and medical record review. –The occupational therapist may also use a quick screening tool such as the ACL. |
Occupational therapists should discuss the patient’s status with other health care providers and with the patient’s family before pursuing an evaluation.
Screening usually occurs before a physician’s order is issued. |
| Evaluation | An occupational therapist can use a standardized assessment such as the Peabody Developmental Motor Scales, Functional Independence Measure (FIM), or the Sensory Profile. If a standardized assessment is used, then the therapist needs to follow the assessment word for word and step by step. -Criterion referenced assessment: the patient’s scores on the assessment are compared to predetermined criteria or standards. The Functional Independence Measure (FIM) is an example of a criterion referenced assessment. -Norm referenced assessment: the patient’s scores on the assessment are compared to a set of normative data that compares the patient to the population from which the data was gathered. This population is usually comparable in age and gender to the patient. The Peabody Developmental Motor Scales is an example of a norm referenced assessment. |
The occupational therapist completes the evaluation, including administering evaluation tools, scoring the results, and writing the evaluation report. –The occupational therapy assistant may assist with the evaluation by completing those portions of the assessments that he or she has been trained to administer under the supervision of the occupational therapist. |
Therapists should consider any language or cultural barriers prior to or while conducting an evaluation. For example, if the therapist has an accent that is different from the patient’s and the patient cannot understand verbal directions due to the therapist’s accent, the therapist should arrange for an alternate means of communication, such as written instructions or asking another staff member to act as an interpreter. |
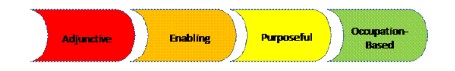
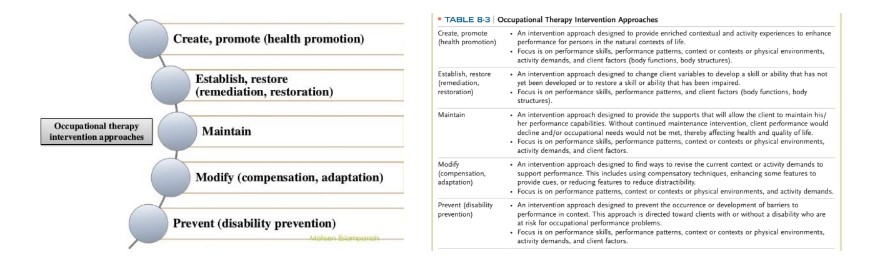
| Intervention | Intervention is provided based on 4 levels. These levels will be discussed in a separate chart. See below. | The occupational therapist or occupational therapy assistant may provide intervention. The occupational therapy assistant is supervised by the occupational therapist based on the occupational therapy assistant’s experience, complications that may arise during intervention, and any pertinent rules, regulations and insurance requirements. | An occupational therapy aide may not provide occupational therapy intervention. An occupational therapy aide may assist the occupational therapist or occupational therapy assistant in providing portions of the intervention under close supervision. Occupational therapy aides should be trained in providing portions of intervention before assisting therapists with patients. When designing a program, the OT needs to research relevant literature to support the process of evidence-based decision-making. |
| Discharge | The patient is discharged from occupational therapy services when goals are met, when progress has plateaued, or when the patient’s medical condition changes and the patient is unable to tolerate occupational therapy services. –Planning for discontinuation of services begins at the evaluation. |
The occupational therapist recommends discharge from occupational therapy services to the referring physician, who approves the dismissal. –In the public schools, the occupational therapist recommends dismissal to the IEP team, who must agree with the recommendation. |
Discharge from occupational therapy services may be dictated by the patient’s insurance company and the limits on the amount of occupational therapy that is allowed by the patient’s policy. Occupational therapy assistants may give the occupational therapist input regarding the discharge of patients but may not recommend discharge themselves. |