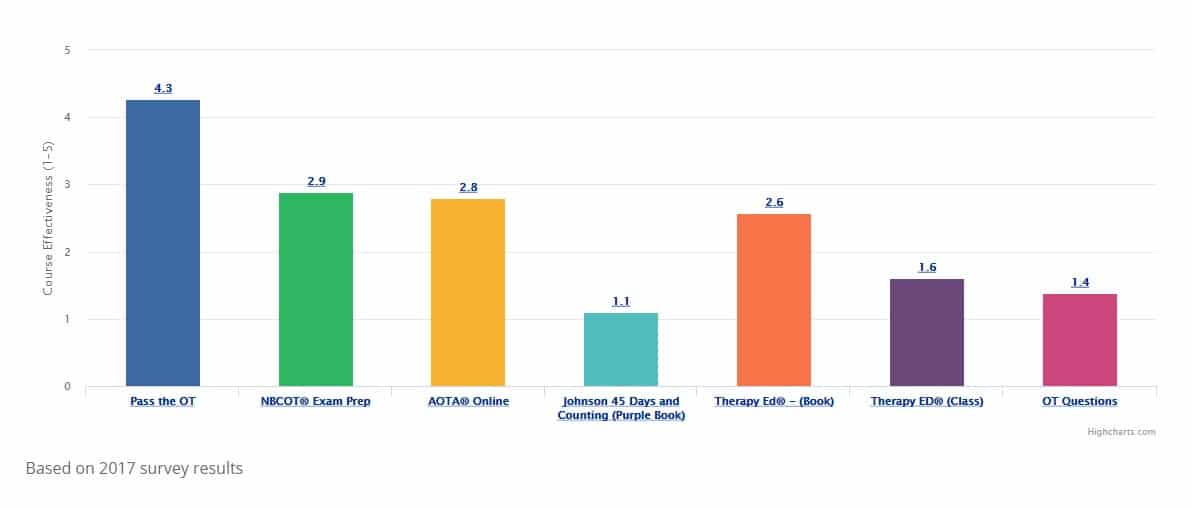
Symptoms and Challenges associated with
Mental Health Diagnoses (PART -2)
| Description, Symptoms, and Challenges | Associated Diagnoses | Support and Treatment | Key Elements to the Therapeutic Approach and Environment | Sample Activities | Video Example | Photo/Aids |
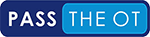
| Sensory experience that does NOT correspond to external reality
-Appear as visual, auditory, tactile, olfactory, or gustatory sensations that do not really exist.
|
Wide range of psychiatric disorders -Schizophrenia -Manic and depressive psychoses -Organic mental disorder -Substance abuse Also occur with certain neurological conditions -Parkinson’s Disease -Alzheimer’s Disease -migraine headaches -brain tumors -Epilepsy |
Move the patient to a less overwhelming area -Remove external stimuli -Temporarily isolate the patient |
Karaoke – sing songs that people should know Make a pizza- premade dough and put toppings on that they want Stimulate sensations other than the one causing the hallucination Play Wii Age involvement with other trusted people Use bright colors |
A short film depicts a girl with schizophrenia confronting her hallucination.
|
 |
|
| Disturbance in mood.
Thinking, talking, and making decisions very quickly. No sense of risk or danger. Recklessness or a feeling of invincibility. Sleeping very little or not at all. Easily distractible. A feeling of being “high” or “on top of the world” without any rational reason. The person experiencing a manic episode may say that they feel great, but they need to be watched very closely for the quick turn from manic to depressed. |
-Bipolar disorder -Schizoaffective disorder -Associated with some medical conditions such as multiple sclerosis -Associated with some medications such as prednisone |
The specific causes of manic depressive and bipolar disorder are still being studied, but some therapies and medications do exist to help patients with these diagnoses. Treatments include mood-stabilizing drugs, antidepressants, antipsychotics, psychotherapy, and in many cases, hospitalization. As well organized routine is usually very helpful for bipolar patients. | An OT may encounter bipolar symptoms in a wide variety of patients. Symptoms of mania may be harder to spot since they can appear positive, like an increase in energy, or a more optimistic outlook. OTs need to be alert for risky behaviors and restlessness that can signal a manic episode. Be cautious of giving criticism Be firm, consistent Reinforce limits Be aware that behaviors are caused by diagnosis and/or medications Be aware that patients may try to manipulate the situation by using flattery Have patients work alone Reduce stimuli in the therapy clinic Provide activities that burn extra energy |
Exercise bike or treadmill Gross motor activities Sports that require a high-energy level, such as soccer Structured activities Simple food preparation |
An entertaining lecture on bipolar disorder. |  |
| A distinct difficulty in reasoning, thinking, processing and understanding.
Risky behaviors, being impulsive, poor social skills. Difficulty living alone or practicing good self-care. Also known as intellectual disabilities. |
Congenital disorders -chromosomal abnormalities and syndromes. Cerebral palsy. Birth trauma. Brain damage due to infantile illness. Epilepsy- May be comorbid with mental illness. |
Special education, life skills training and developmental and behavioral therapies are all helpful for this diagnosis. Routine and physical exercise are also encouraged. Animal-assisted therapies and sensory based therapies have also proved very effective. | An OT’s main goal should be to improve the quality of life. This includes teaching job skills, cooking, cleaning, self-care, and social skills. | -ADL training -IADLs, including cooking and simple meal prep, housekeeping, community mobility, money management -Vocational training -Adaptations for deficits in literacy and math skills |
A video and description of an occupational therapy session with a child with Down syndrome. | 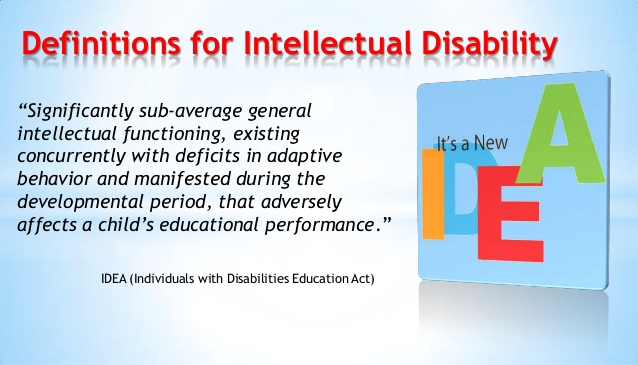 |
| There are two main categories within mood disorders: Dysthymic and Cyclothymic.
In general, a mood disorder is less severe than the full diagnosis of depression or bipolar. Dysthymic mood disorders can be a “low-grade” version of depression. A patient may display some signs of depression, but can cope on a daily basis. A Cyclothymic disorder is a “low- grade” version of bipolar. It has ups and downs but the episodes may be shorter and less severe than the full bipolar diagnosis. Both dysthymic and cyclothymic disorders can be “warning signs” pointing to the onset of more severe disorders. |
-Dysthymic Disorder -Major Depressive Disorder -Pervasive Depressive Disorder -Cyclothymic Disorder -Seasonal Affective Disorder |
Treatments may include medications (antidepressants, mood stabilizers and antipsychotics) and psychotherapy. An active and healthy lifestyle can also help to manage the symptoms of mood disorders. | Some sources say that as many as 10% of the US population suffers from some type of mood disorder. An OT should be prepared to handle these symptoms and challenges on a daily basis with a wide range of patients. | -Relaxation and stress management techniques
-Education in coping techniques |
An educational video about mood disorders. | 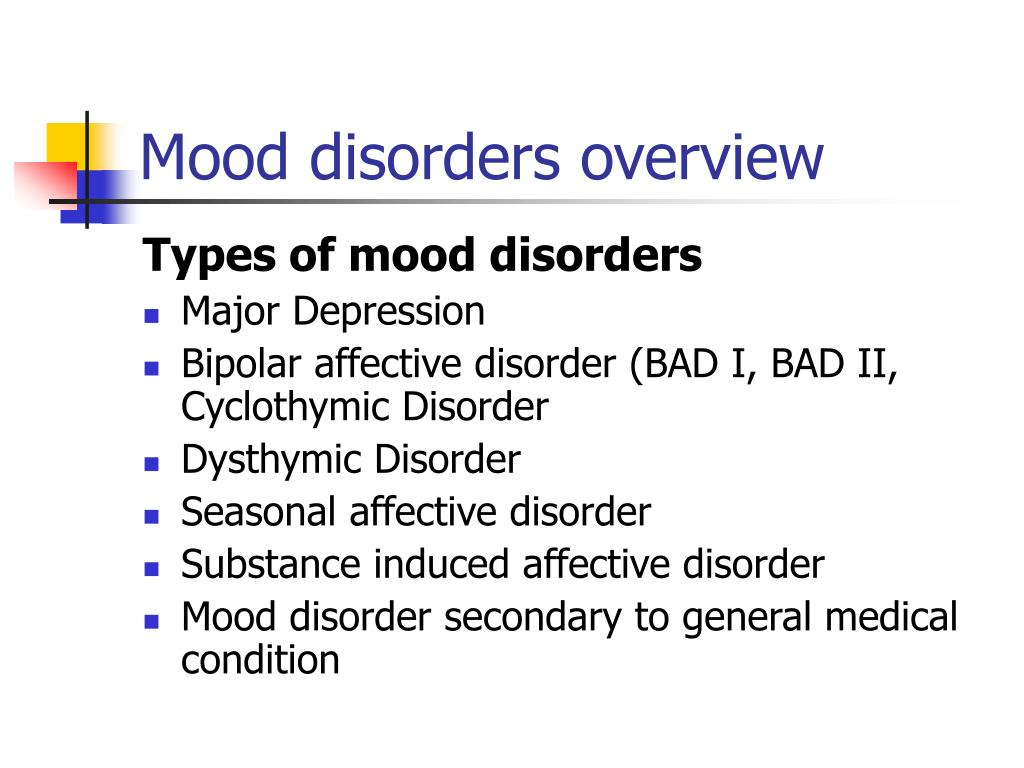 |
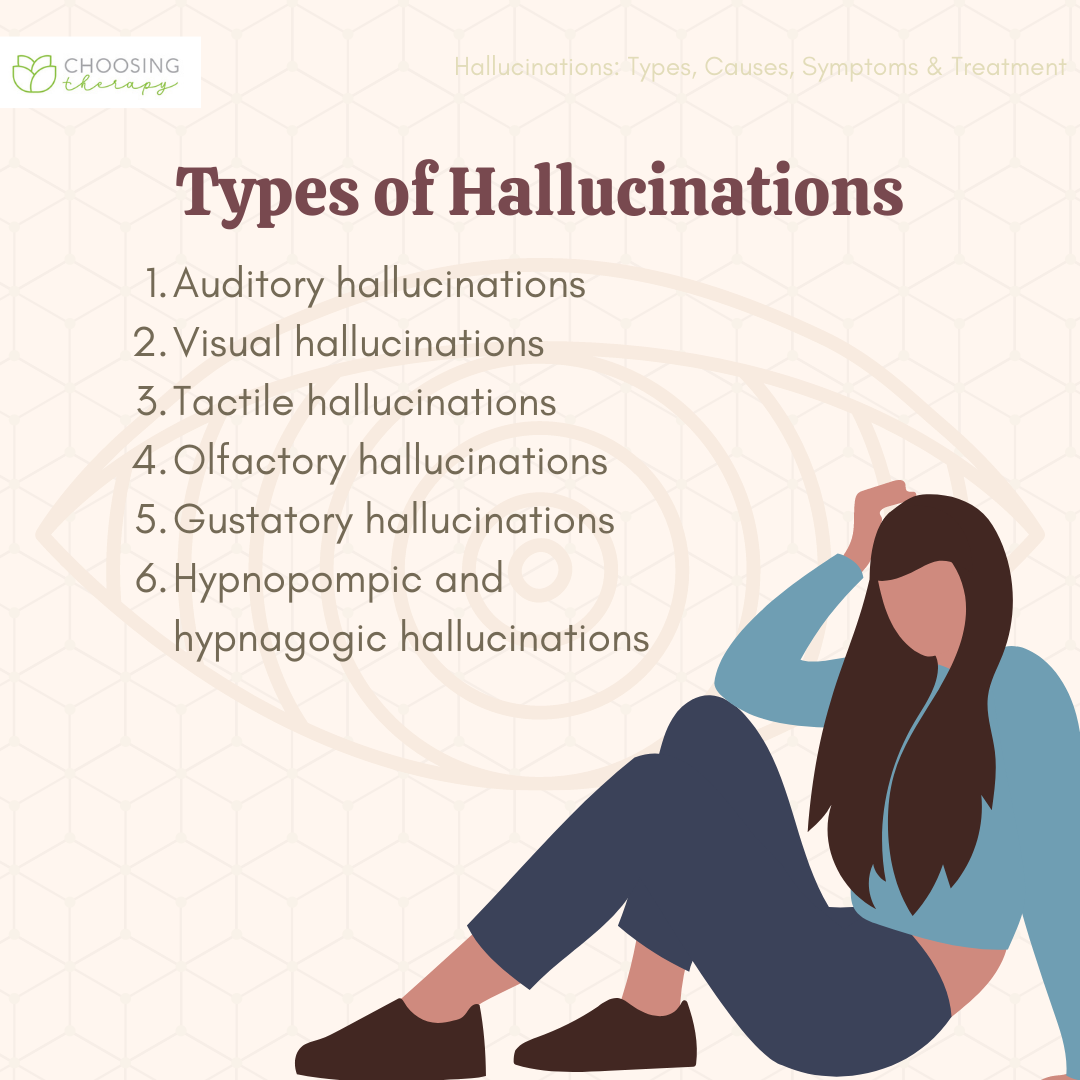
| Unbalanced thoughts that lead to unbalanced behaviors.
Fear, irrational worry, extreme need to do or avoid doing something. Feeling anxious or panicking if something is done out of order or in the wrong way. Hoarding, cleaning, organizing, and picky eating can all be signs of OCD. OCD is often misunderstood because of the way it is portrayed in TV and movies. OCD is not simply about funny behaviors. Patients with true OCD live in a world where every action they take has deep meaning and they can be extremely fearful, angry, and depressed |
-Anxiety disorders -Eating disorders -Depression -Bipolar disorder -Panic attacks |
Cognitive behavioral therapy and exposure/aversion therapy are commonly used to treat OCD. Support groups are also helpful. Some prescriptions are also available to help manage anxiety and obsessive thoughts. | OCD behaviors often begin slowly and with something minor, like needing to have food cooked a certain way, or having to clean the kitchen in a certain way every night. But if this develops unchecked it can consume the patient very quickly and have huge consequences for their mental health. | -Crafts and hobbies
-IADLs, incorporate realistic habits and expectations, focus on reducing rituals |
A TED Ed video about OCD. | 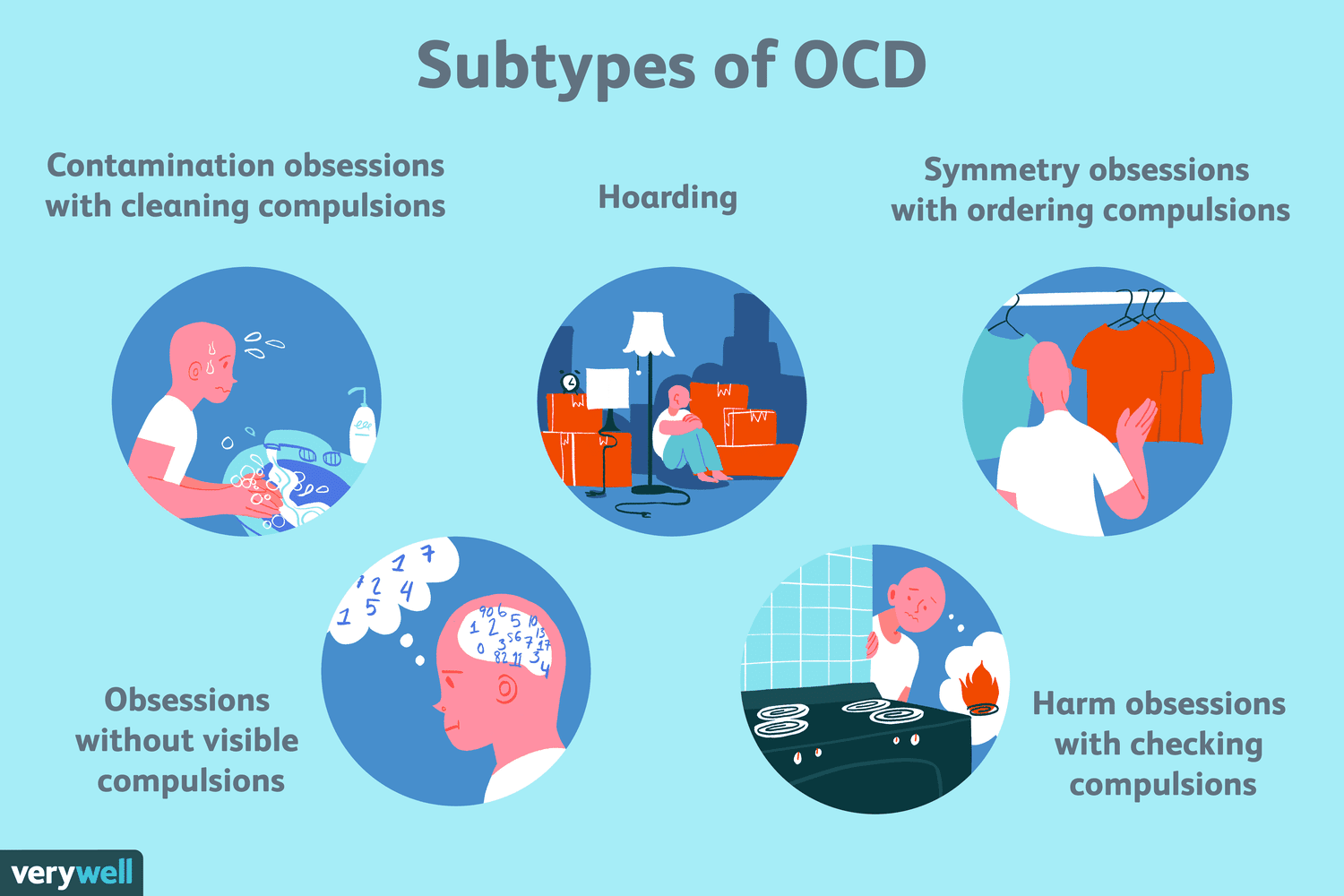 |
| An episode of extreme anxiety.
Fast breathing, not being able to catch your breath, pain in chest or stomach, shaking, sweating, irregular heartbeat, nausea or gastrointestinal issues. |
Treatment for panic attacks include therapy to address the underlying issues and lifestyle changes to help prevent panic attacks. A patient can stop their own panic attacks by avoiding stimulants like nicotine and caffeine, by learning breathing and relaxation techniques and by recognizing and managing stressful situations. | An OT should educate a patient on deep-breathing, relaxation, meditation and other calming activities. This way, a patient can learn to avoid or manage a panic attack even when they are alone. | -Education in healthy lifestyle techniques – diet, exercise -Relaxation and stress management techniques -Therapeutic activities and groups to address habits related to panic attacks – alcohol and drug use, smoking, caffeine intake, etc. |
A brief video on how to help someone having a panic attack. | 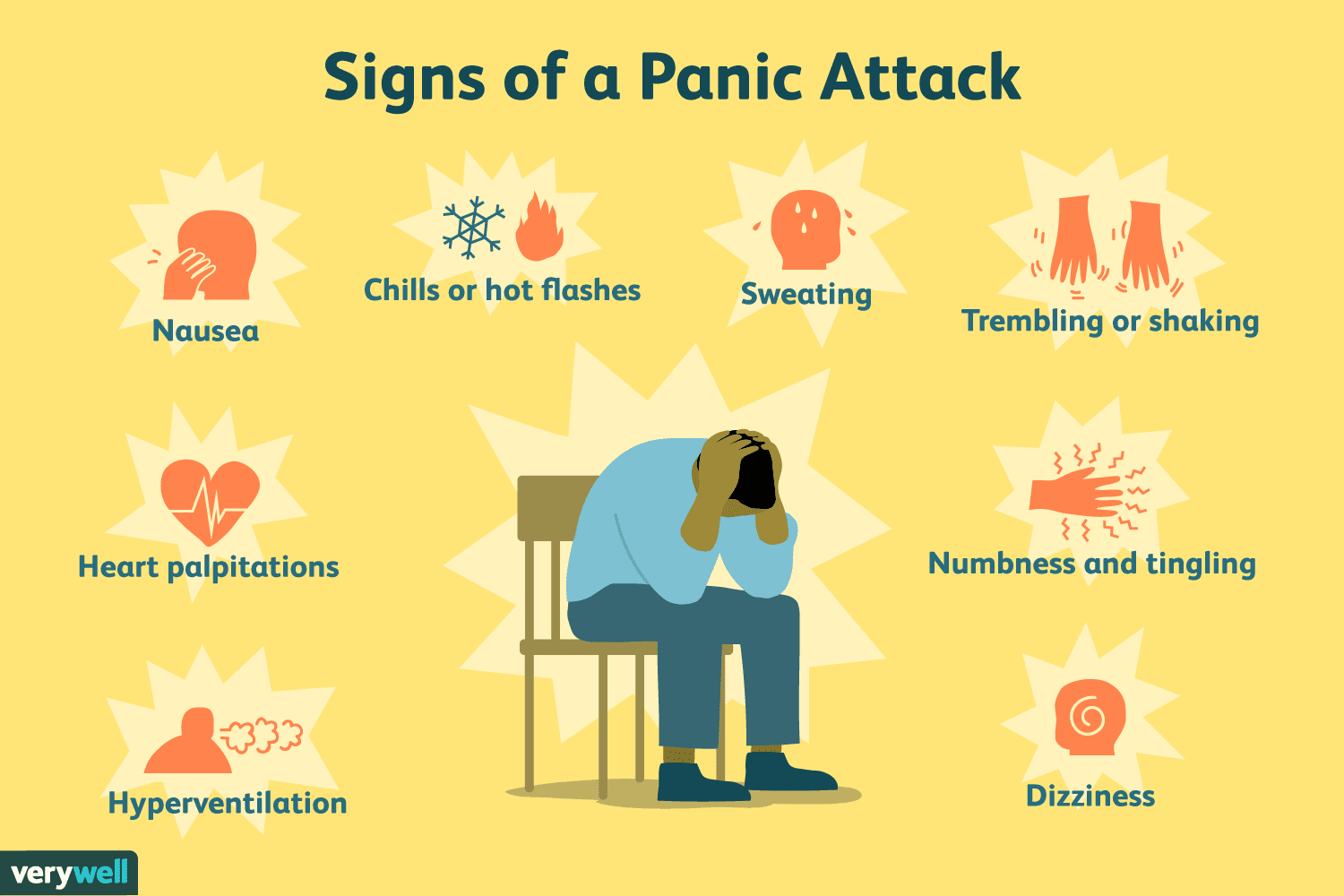 |
|
| Description: type of thinking in which persecutory and grandiose ideas predominate.
-General suspiciousness and very extreme and unbelievable ideas (paranoid ideation), |
– Paranoid schizophrenia – Psychotic depression – Borderline and narcissistic personality |
Look at the world from their point of view Avoid approaching from behind or suddenly Do not whisper- the patient will think you are talking about him or her Be clear, concise, directive Avoid arguing Be truthful and do not make empty promises – The patient may try to form a special relationship with staff |
During group sessions, let the patient. sit at a separate table but with whomever they wish – Maintain the same people in a group so they gradually build trust – Don’t force socialization Keep the environment as stable as possible – Prepare the pt. for any changes in their environment well in advance |
Provide activities that the patient can control, meet at the patient’s intellectual level without getting competitive -Copper tooling: select the design, still level of direction from the leader -Relaxation techniques: guided imagery: person with paranoia writes down what people say on the board -Pasta salad: planning and making: have materials listed and patients prepare it.Keep roles, routines and habits the same. – Roles: participant, helper, director – Routines: standard, no surprises, know well in advance about changes, need structure – Habits: for a group, make sure set-up is consistent and people put away materials in the same spots |
A short film portrays a young man with paranoid personality disorder. | 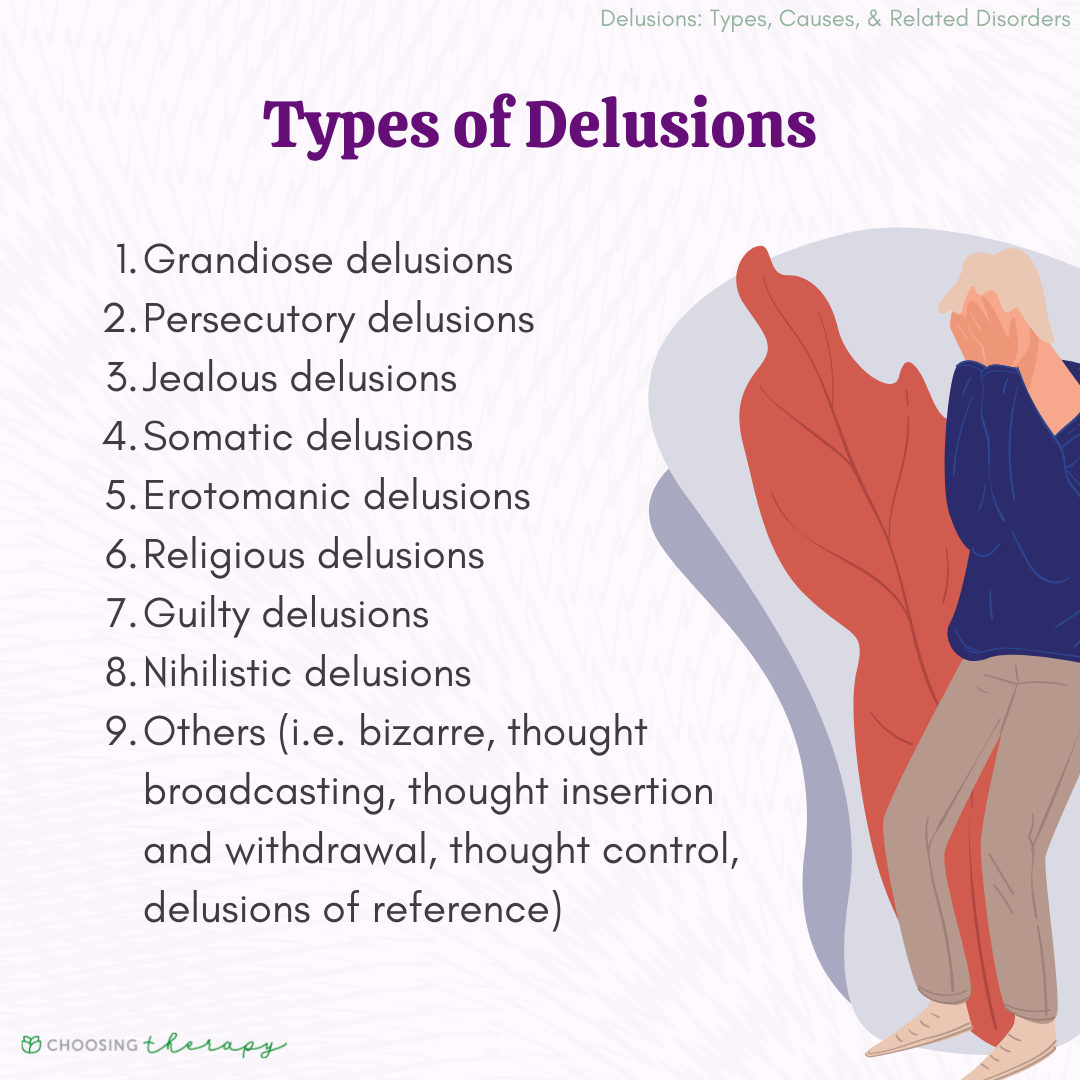 |
| Deep need for praise or honor, very high view of self, poor social skills, little or no concern for others or their feelings, aggression, entitlement, pride, and inability to build and maintain relationships.
This is a large and varied group of disorders, and they each have their own symptoms and characteristics. However, there are some traits that are common to all the disorders. |
Personality disorders or PD are grouped into three clusters. –Cluster A is Paranoid PD, Schizoid PD, and Schizotypal PD. –Cluster B is Antisocial PD, Borderline PD, Histrionic PD, and Narcissistic PC. –Cluster C is Avoidant PD, Dependent PD, and Obsessive- Compulsive PD. |
Talk therapies are common treatments for personality disorders. These may include a combination of support groups, counseling and family sessions. Patients with these disorders need to be monitored for changes and increases in symptoms. | An OT should work with the patient to keep their mind on reality and to help them develop social and interpersonal skills while managing other symptoms. | -Reality based therapeutic activities and groups -Social skills groups -IADL training |
An entertaining lecture about personality disorders. | 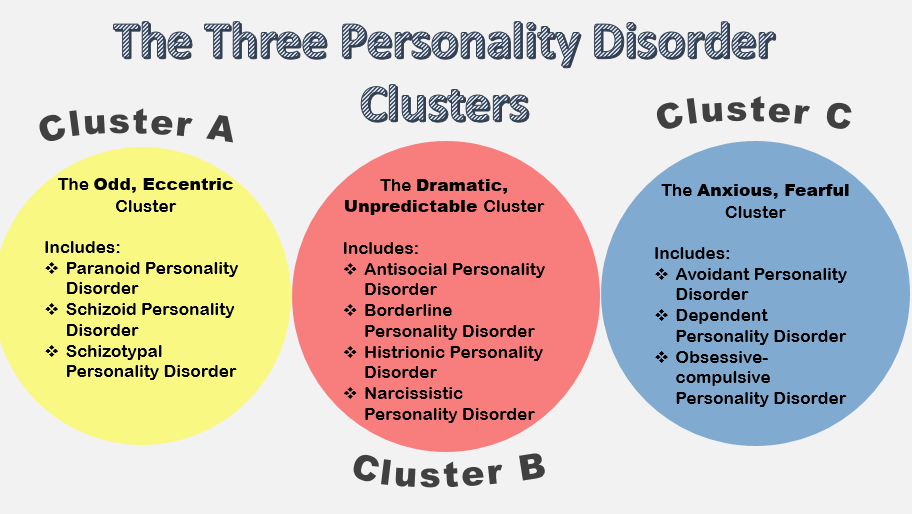 |
| Anxiety, loneliness, inability to sleep, inability to feel joy, anger, aggression, nightmares (night terrors), feeling guilty, risky behaviors, self-harm, suicidal thoughts.
Often the symptoms of PTSD are triggered when a situation or event reminds the person of the trauma they experienced. These triggers can be hard to predict. Sometimes even the littlest thing can trigger a major and explosive reaction. |
-Anxiety -Depression |
Since PTSD is often accompanied by anxiety and depression, medication to treat those two conditions are often prescribed for those with PTSD. Therapy is essential for PTSD patients and should focus on helping the patient understand and overcome that initial trauma. Support groups can also be helpful. | The first goal of an OT should be to determine how much the PTSD has impacted the patient’s performance and work to discover the specific triggers for the patient. Triggers should be understood and addressed while providing training to the patient and their caregivers to avoid triggers and create healthy routines. | -Individual and group activities that address trauma triggers and warning signs -Education in coping strategies -Stress management and relaxation techniques -IADL training or retraining, including time management, money management, vocational rehabilitation and driver training or retraining |
A TED Talk about PTSD. | 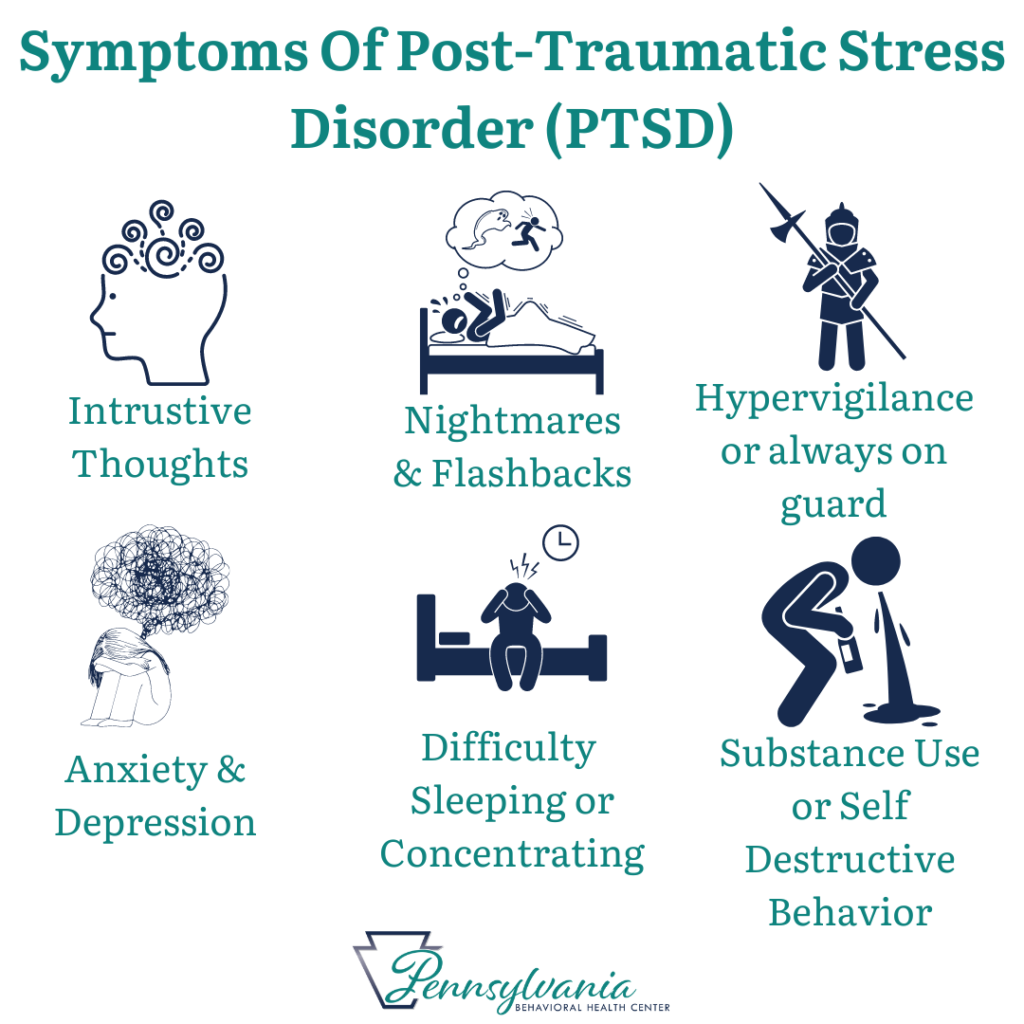 |
| Schizophrenia has a long list of symptoms but fall under the category of abnormal social behavior.
Some patients also hear or see things that are not real – delusions or hallucinations. Patients may also harm themselves or others have significant cognitive impairment. Research shows that Schizophrenia is strongly linked to genetics, but brain chemistry and environmental factors also play a role. These patients can be extremely volatile, unstable and sometimes dangerous. Additional research reveals the influence of cognitive deficits on daily function. The level of cognitive impairment varies between people diagnosed with Schizophrenia, but this impairment tends to stay stable throughout each person’s lifetime. The following cognitive skills tend to show varying levels of dysfunction in people diagnosed with Schizophrenia: -working memory (often referred to as short term memory) – usually significantly impaired |
-Hallucinations -Delusions -Anxiety disorders -Depression -Obsessive compulsive disorder (OCD) -Substance abuse |
The main treatment for Schizophrenia is medication and there are many different pills and injections available. This diagnosis often requires hospitalization. Group and individual therapy can also be helpful in rehabilitating the patient and increasing their social skills. | OTs should focus on quality of life. Some symptoms of this disorder may be reduced through psychoeducation and training in self-care and social interactions. -Keep the environment stable and structured. -Foreshadow change or other factors that could create stress -Emphasize caring and support -Minimize environmental distractions and sensory input if the patient displays symptoms of an acute episode. -Insure that the patient stays on his or her medication schedule. -Avoid using sharp objects during therapy sessions if patient is not yet stapilized. |
-Group activities to address social skills -Therapeutic activities and adaptations to address cognitive skills -ADL and IADL training -Mindfulness training -Family and caregiver education in the disease and how to provide support at home. |
A brief discussion about psychosocial treatment for schizophrenia. | 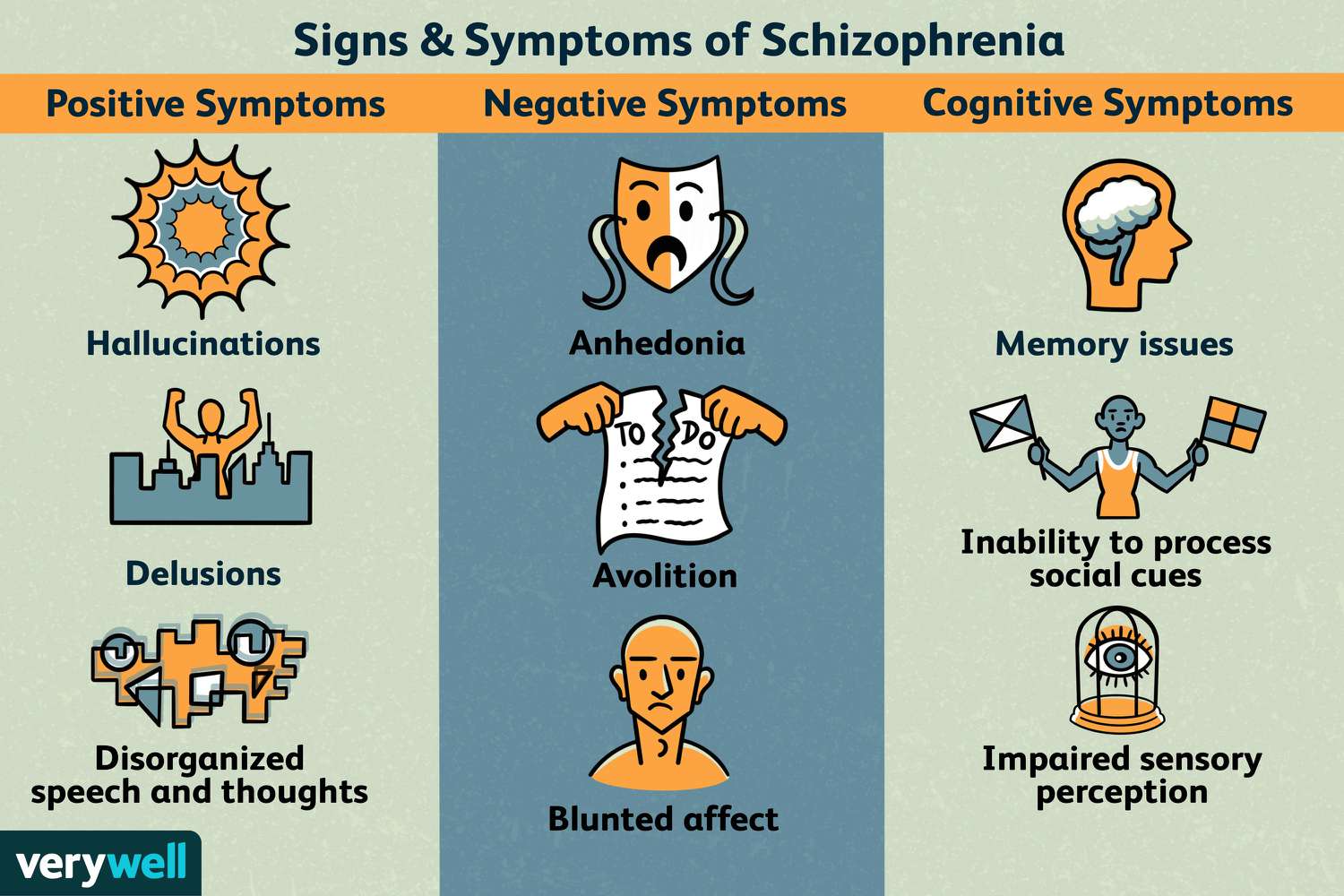 |
| Any behavior that would normally be seen as explicitly sexual or provoking a sexual response
-Might include removing clothing and/or masturbating in public |
Usually occur in pts. who are psychotic Associated with psychosexual disorder |
Approach in calm, non-judgmental way. -Explain the rules of therapy and strictly enforce them. Be clear about limits but maintain the therapeutic relationship. -The patient may confuse therapeutic relationship Last resort: ask another therapist to provide treatment to the patient. |
Non-crowded environment Remain non-judgmental Patient should have personal space Protect the patient from sudden touch, smell, warmth of others |
Sanding or other activities that involve physical exertion -No contact sports Gross motor activities Educate in safe sex practices |
A student film demonstrates a psychosexual disorder. | 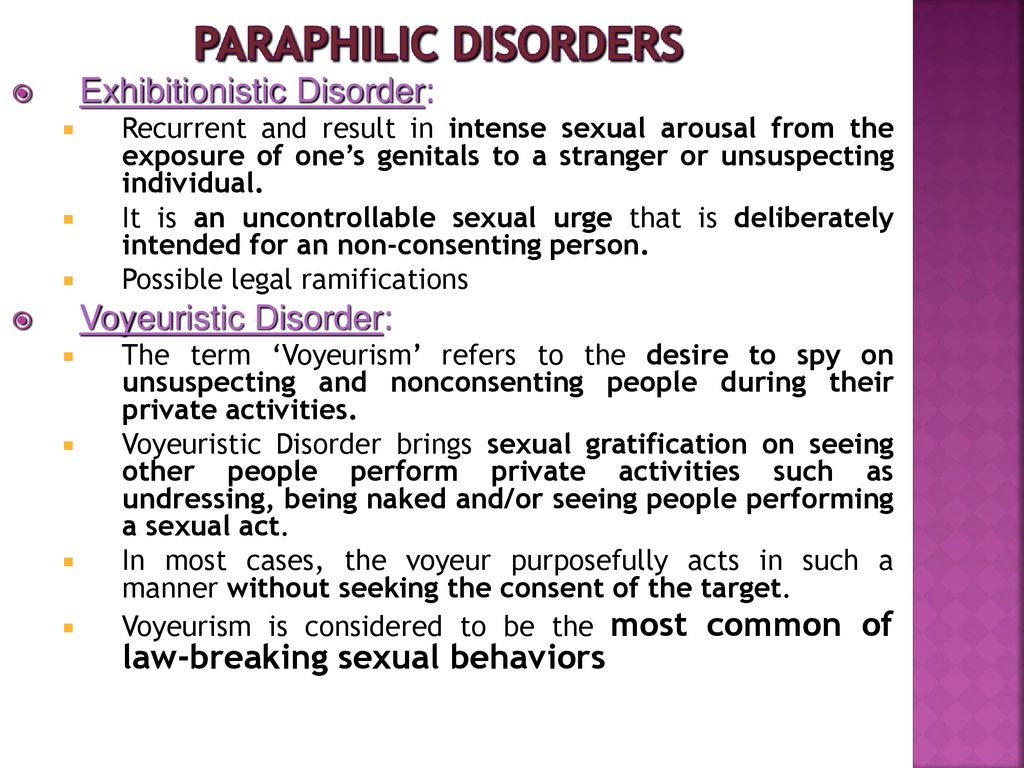 |
| A dependence on any substance, usually drugs or alcohol.
This is not occasional use, but persistent, compulsive need for the substance. Withdrawals when trying to quit. |
-Anxiety -Depression -PTSD -Schizophrenia -Mania -Anti-social personality disorder -Dementia |
Psychotherapy is the leading form of treatment for substance abuse. This treatment can take many different forms and take place in many settings. Some prescriptions are also available to help balance withdrawals or create an aversion to the substance. Alternative therapies are also becoming more popular for substance abuse. | Overcoming addiction is a tiring and overwhelming process for both the patient and their family. There is often a great deal of distrust from the family of an addict. They’ve seen many things fail in the past. An OT will need to support and educate both the patient and the caregiver for a positive outcome to be maintained. | -Individual and group activities that focus on behaviors and lifestyle changes -Relaxation and stress management techniques -IADL training -Vocational rehabilitation -Exploration of leisure activities -Education in health and wellness |
A short lecture on substance use disorders (substance abuse). | 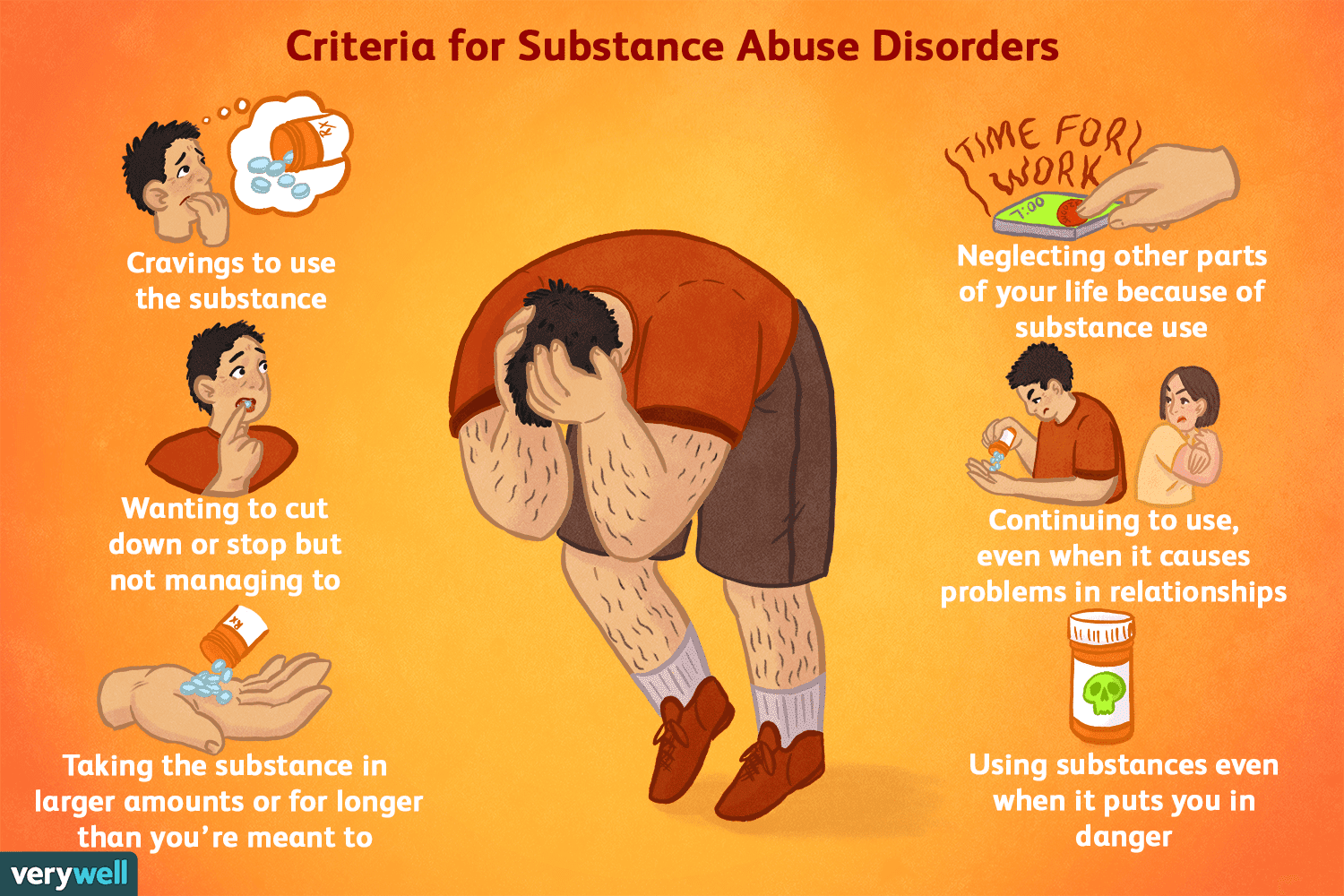 |