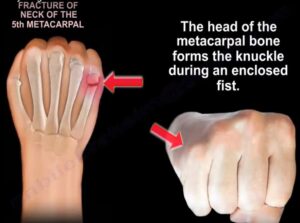
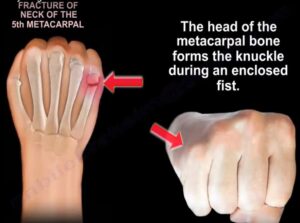
Boxer’s Fracture
(Proximal Fracture) |
A boxer’s fracture is the result of a clenched fist hitting an object with enough force to break the MCP neck, most commonly seen in the fourth and fifth digits. |
|
Ulnar gutter splint |
|
 |
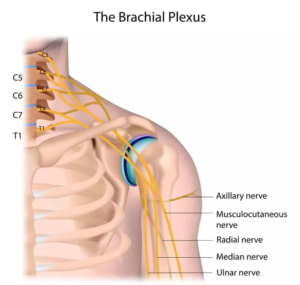
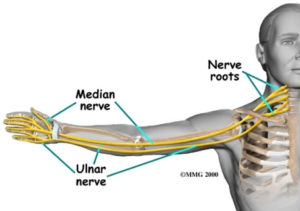
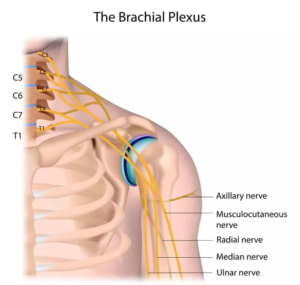
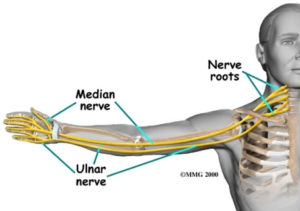
| Brachial Plexus Injury |
A network of nerves that
conducts signals from the spinal
cord, which is housed in the
spinal canal of the vertebral
column (or spine), to the
shoulder, arm and hand.
These nerves originate in the fifth, sixth, seventh and eighth
cervical (C5-C8), and first
thoracic (T1) spinal nerves, and innervate the muscles and skin of the chest, shoulder, arm and hand. Brachial plexus injuries or lesions are caused by damage to those nerves. They can occur as a result of shoulder trauma, tumors, or inflammation. |
Treatment includes
orthosis/splinting, surgery, or it may heal without treatment. The ability to bend the elbow (biceps function) is considered an indicator of probable recovery. Additional upward movement of the wrist and straightening of thumb and fingers an even stronger indicator of excellent spontaneous improvement. Gentle range of motion exercises. |
Flail arm splint
provides the needed
stability at both the
shoulder and elbow for functional positioning of the hand. |
Any motion beyond 90° abduction may induce added stress to the brachial plexus and its roots. |
 |
| C5 SCI |
Movements possible: Shoulder,
flexion, abduction, extension.
Elbow flexion, supination.
Scapular adduction, abduction. |
|
Wrist splint in a
functional position with a slot to hold a typing stick |
|
 |
| C6-C7 SCI |
Movements possible:
C6:
Scapular protraction (partial
horizontal adduction). Forearm
supination. Radial wrist
extension.
C7: Elbow extension
Ulnar/wrist extension. Finger
extensions. Thumb flexion,
extension & abduction |
Practice to allow the
proximal interphalangeal
(PIP) joints to develop a
contracture to facilitate
functional grasp.
Ranging the hand (wrist extension combined with finger flexion and wrist flexion combined with finger
extension) of a patient with
a spinal cord injury preserves a functional tenodesis grasp while encouraging PIP flexion
contractures |
Tenodesis splint. C6
(wrist driven flexor
hinge splint during a
prehension activity). |
|
 |
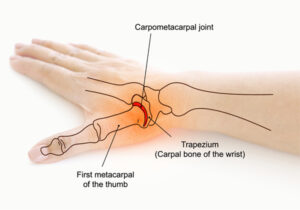
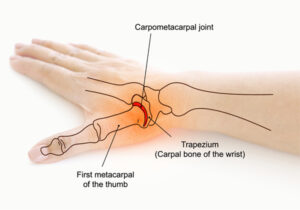
| CMC arthritis |
Most commonly involved
arthritic joint in the hand.
More common in women, may exist in a localized form or may exists as a systemic form of arthritis, primary form is most common in postmenopausal women, systemic form may be due to RA or gout |
|
A hand-based thumb
splint |
|
 |
| Carpal Fracture |
Fracture to the individual carpal
bone. Most common injury to
the wrist is the scaphoid. Lunate fractures are associated with Kienbock’s disease. |
|
|
|
 |
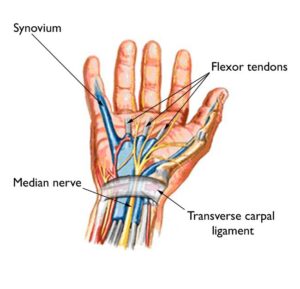
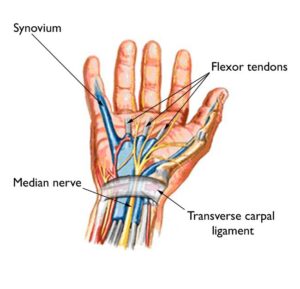
| Carpal tunnel |
Median nerve injury. Symptoms
include palmar numbness and
numbness of first digit to half of
the fourth digit, with generalized weakness and pain. |
Conservative management: wrist splint in neutral, median nerve gliding exercises, activity mod, ergonomics.
Post-surgical management: edema control, AROM, nerve/tendon glides, sensory re-ed., strengthening, activity mod. – Pillar pain is pain on
either side of the carpal
tunnel release surgery site. The source of the pain is unknown and may be ligamentous or muscular in origin. |
Wrist volar splint with wrist in neutral |
|
 |
| CMC osteoarthritis |
Degenerative joint disease
affecting the first carpometacarpal joint (CMC1).
This joint is formed by the trapezium bone of the wrist and the first metacarpal bone of the thumb. Occurs when the cushioning cartilage of the joint surfaces wear away, resulting in damage of the joint. |
Splinting and activity
modification |
A thermoplastic splint osteoarthritis to
support the CMC joint or a CMC neoprene wrap support to provide more movement but less support. |
|
 |
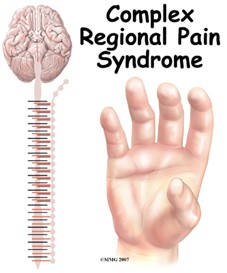
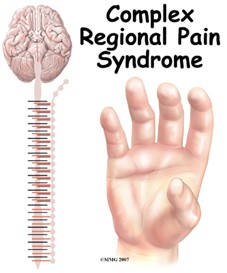
Complex Regional
Pain Syndrome
(AKA: reflex
sympathetic dystrophy |
Distal radius fracture is the
primary reason. Pain dispropriate to an injury that is either sympathetically maintained or independent of the sympathetic nervous system. Symptoms often include pain, swelling, stiffness, sudomotor and trophic changes. |
Gentle, pain-free AROM
for short periods, stress
loading (i.e.scrubbing the floor, carrying a weighted bag). Pain control techniques TENS, splinting, continuous passive motion. Edema control techniques (i.e., elevation, massage
AROM, contrast baths,
compression). Desensitization techniques, Fluidotherapy, blocked exercises, tendon gliding, joint protection, energy conservation.
Provide instruction in a
stress loading program
and incorporation of use
of the upper extremity in
functional activities. |
Static then dynamic as tolerated. Volar in
extension, as tolerated
Circumferential wrist
might be used to avoid edema |
PROM or painful
treatment. Wearing
an arm sling will
increase stiffness
and edema
because it places
the extremity in a
dependent and
static position for
long periods of
time. |
 |
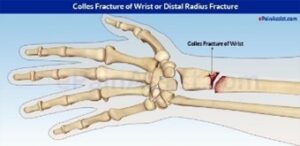
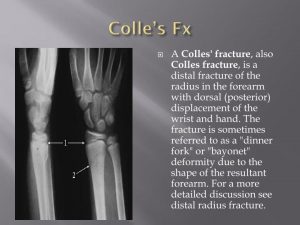
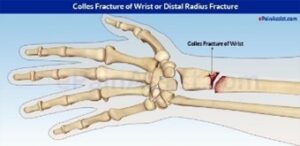
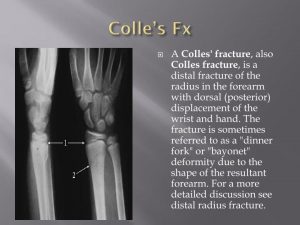
| Colles Fracture |
Complete fracture of the distal
radius with dorsal displacement.
Most common type of wrist
fracture. |
Orthotics are used for
immobilization as needed.
ROM is begun early, within 1 week if medically cleared. A sling is used
for type 1 fractures or comfort if the patient has
pain and is nervous in
public places. |
|
|
  |
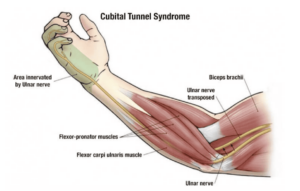
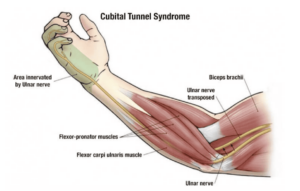
| Cubital tunnel syndrome |
Ulnar nerve compression at
elbow; numbness/tingling along
ulnar aspect of forearm/ hand,
pain at elbow with extreme ,
weak power grip; elbow splint to prevent ; + Tinel sign at elbow (pain or sensation) |
Conservative management: elbow pad to decrease
compression of nerve,
activity mod. Post-surgical management: edema control, AROM, nerve glides,
strengthening, MCP splint if clawing is noted |
(non-surgical) elbow
splint to prevent |
|
 |
Cumulative
trauma disorder
(CTD) |
Trauma to soft tissue caused by repeated force. Patient has muscle fatigue, pain, chronic inflammation, sensory impairment, decreased ability to work.
Ex. playing piano 10
hours a day |
Acute phase: reduction of
inflammation and pain
through static splinting, ice, contrast baths, ultrasound, interferential stimulation. Subacute phase: slow stretching, myofascial release, progressive resistive exercises as tolerated, proper body mechanics, education on identifying triggers and returning to acute phase treatment. Return to work, functional capacity evaluation, work hardening. Activity modification and proper
body mechanics are essential for long-term control of an inflammatory cumulative trauma disorder. |
Static splint during
activities that cause
pain. |
|
 |
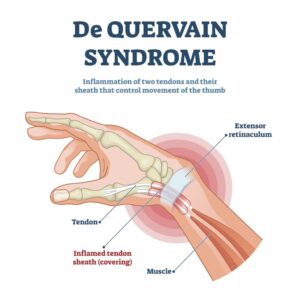
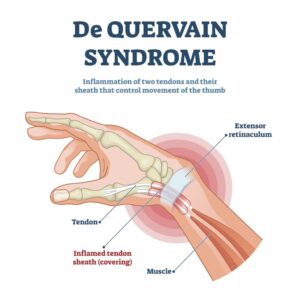
| De Quervain’s Disease |
Caused by cumulative microtrauma resulting in tenosynovitis of the thumb, muscle tendon unit, abductor
pollicis longus and extensor pollicis brevis, and the tendons in the first dorsal compartment of the wrist. Get it through repetition. |
Conservative management:
computer ergonomics workstation education and strengthening exercises. Post-surgical management: gentle ROM, tendon gliding exercises, grip and pinch
strengthening after 2 weeks, scar management and desensitization techniques are used.
Use isometric exercises first. |
Thumb Spica Splint
including wrist.
Forearm based thumb spica splint with wrist in neutral and thumb radially abducted for 3 weeks. After 3 weeks, the patient can progress to a soft splint and isometric exercises. post-surgery put in, up to 20 degrees extension. |
Nonoperative
treatment: activity
modification and
avoidance of pinch
are recommended. |
 |
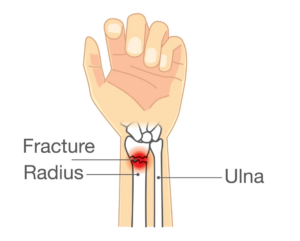
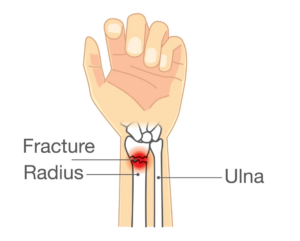
| Distal Radius fracture |
Look at Colles fracture and
Smith’s fracture. With edema
use edema message, finger
dexterity and strengthening |
Initiation of controlled
AROM can begin between 3 and 6 weeks post injury if the fixation of the fracture is adequate. |
Wrist extension splint. |
|
 |
| Double Crush Syndrome |
Occurs when a peripheral nerve is entrapped in more than one location. Symptoms: Intermittent diffuse arm pain and paresthesias with specific postures. |
Conservative management:
treat according to each
nerve injury or syndrome.
Nerve gliding exercises,
and exercises for scapular stability, posture, and core trunk strengthening. |
|
Avoid movements
or postures that
aggravate symptoms. |
 |
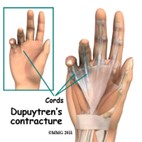
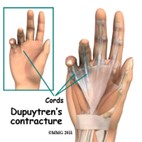
| Dupuytren’s Disease |
Disease of the fascia of the palm and digits. Results in flexion deformities of the involved digits (i.e., mostly ring finger) |
Wound Care: dressing
changes. Whirlpool if
infection is suspected.
Edema Control: elevation
above the heart. A/PROM and progress to strengthening when wounds are healed. Scar management, functional tasks that emphasize flexion (griping) and extension (release). |
Extension splint at all
times except to remove for ROM and
bathing |
|
 |
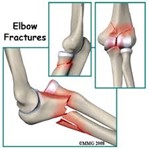
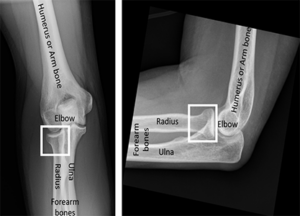
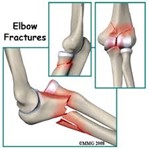
| Elbow fracture |
Involvement of radial head may
result in limited rotation of
forearm. Usually caused by a forceful load through an outstretched arm. |
ROM begins early, within 1 week if medically cleared. |
Orthotics are used for
immobilization as
needed. A sling is
used for Type 1 fracture (nondisplaced) or
comfort if the patient
has pain and is
nervous in public
places. |
|
 |
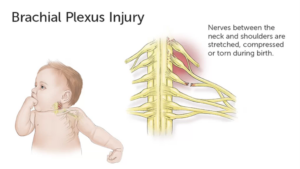
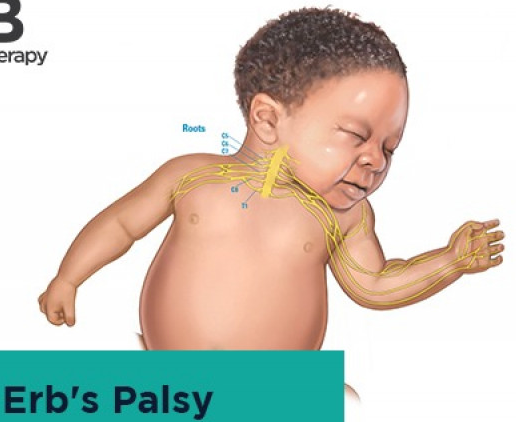
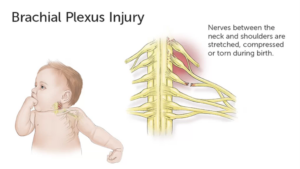
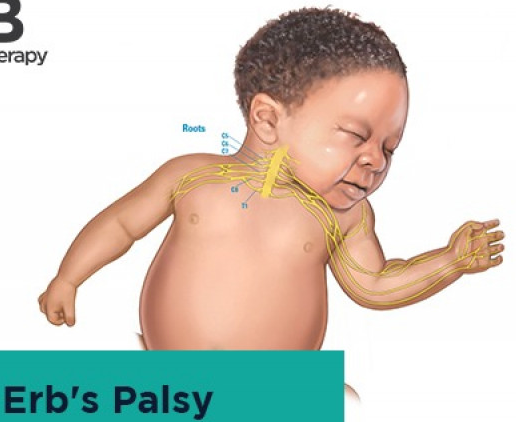
| Erb’s palsy |
Paralysis of the arm caused by
injury to the upper group of the
arm’s main nerves, specifically
the severing of the upper trunk
C5–C6 nerves. The arm hangs
limp with the shoulder rotated
inward due to atrophy and
paralysis in the biceps, deltoid,
brachialis, and brachioradialis
muscles. This significantly limits functional movement. |
The paralysis can either
resolve on its own over a
period of months, necessitate rehabilitative therapy, or require surgery |
Elbow lock splint
stabilizes the elbow to enable the individual to position the hand closer to or away from his/her body for functional use. |
|
 |
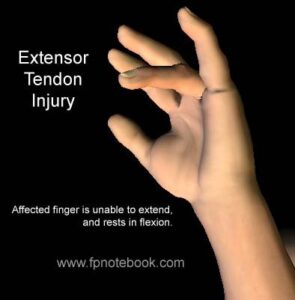
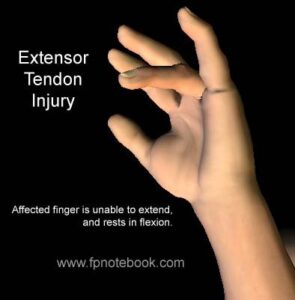
| Extensor Tendon Injury |
Injury to the extensor digitorum communis, extensor indicis proprius (EIP) |
Exercises promote
tendon excursions and
prevent adhesions.
Modalities include heat, to
gradually prepare the tissue for motion, and NMES to promote tendon excursion and activation. Use of modalities begins once cleared by the prescribing physician. A clearly identified and planned home program is important to ensure the patient’s safety and progress toward goals.
Tendon glides are used to
promote excursions and prevent adhesions. ROM.
Strengthening usually not
initiated until the late phase of repair, usually 8- 12 weeks after surgery. |
|
|
 |
| Flaccidity |
Lacking firmness, resilience, or muscle tone |
|
Resting hand splint |
|
 |
| Flaccid wrist |
Lacking firmness, resilience, or muscle tone in the wrist |
Support the user’s wrist in
10 to 20 degrees of extension to prevent contracture, but allows digits to function |
Cock up splint |
|
 |
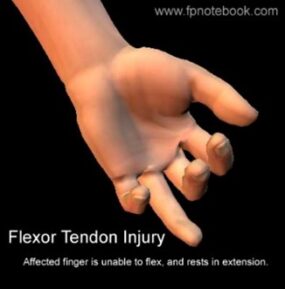
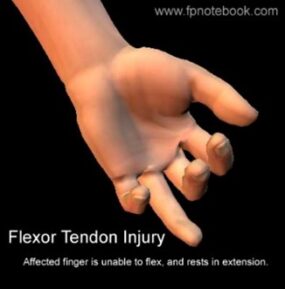
| Flexor tendon injury |
A deep cut on the palm side of
your fingers, hand, wrist, or
forearm can damage your flexor
tendons, which are the tissues
that help control movement in
your hand. A flexor tendon injury
can make it impossible to bend
your fingers or thumb. |
Flexor tendon protocol
using controlled passive
motion. Passive extension of the distal interphalangeal joint if the metacarpal and proximal phalangeal joints are flexed. The distal interphalangeal joint and proximal interphalangeal joint can be passively extended if the other joints of the digit are flexed to initiate tendon glide and prevent scarring of the tendon. Zone II of the flexor tendon system has been called no man’s land because excessive scarring makes it difficult to get good results from a repair. Zone IV consists of the transverse carpal ligament, and the median nerve runs under this ligament; Zone V is distal to this ligament and thus contains the median nerve branch. |
Kleinert or Duran
dorsal protection
splint. The dorsal
blocking splint protects the surgery and guards against flexor tendon rupture. |
A tendon repair is
typically, at its
weakest 10–12
days post-surgery
during the
fibroplasia phase, in
which collagen is
just beginning to be
laid down to
strengthen the repair.
|
 |
| Fracture of Medial Epicondyle |
Paralyzed interossei (no abduction/adduction of the fingers) and no flexion in little and ring finger reduced causing Ulnar Claw Hand |
Gentle active range-of- motion exercises may begin within 1 week after injury. |
Initially, the arm
should be splinted in
90° of elbow flexion.
Protective splinting
may be continued for
3 weeks if necessary. |
|
 |
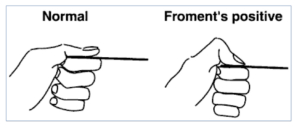
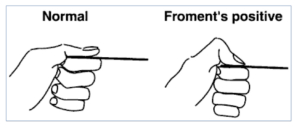
| Froment’s sign |
Froment’s sign is a test of the
wrist. It tests for palsy of the
ulnar nerve, specifically, the
action of adductor pollicis.
Occurs when the flexor pollicis
longus compensates for a weak or paralyzed adductor pollicis and flexor pollicis brevis. When a patient attempts to pinch, the interphalangeal joint of the thumb flexes more than usual. |
To perform the test, a patient is asked to hold an object, usually a flat object such as a piece of paper, between their thumb and index finger (pinch grip). The OT then attempts to pull the object out of the subject’s hands. A normal individual will be able to maintain a hold on the object without difficulty. However, with ulnar nerve palsy, the patient will experience difficulty maintaining a hold and will compensate by flexing the FPL (flexor pollicis longus) of the thumb to maintain grip pressure causing a pinching effect. The compensation of the affected hand results in a weak pinch grip with the tips of the thumb and index finger, therefore, with the thumb in obvious flexion. |
|
|
 |
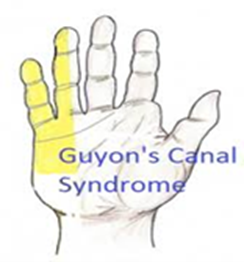
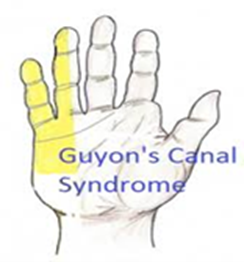
| Guyon’s canal |
– An ulnar nerve compression at the wrist; numbness/tingling in ulnar nerve distribution of hand; motor weakness of ulnar nerve innervated musculature; neutral wrist splint; + Tinel’s sign at Guyon’s canal. |
Conservative management: work activity mod. Post-surgical management: edema control, AROM, nerve glides, sensory reed.,strengthening |
Non-surgical- wrist splint in neutral, |
|
 |
| Humeral fracture |
Most common fracture of the
upper arm and may involve the
articular surface, greater or
lesser tuberosity, or surgical
neck |
With a nondisplaced
fracture of the humeral
neck, support from a sling
and supervised exercise
lead to the most desirable
outcome. Displaced fractures require open reduction internal fixation surgery. Post-surgical management includes physical agent modalities for pain control, AROM, strengthening when cleared by physician. |
Humeral fracture brace for nonsurgical intervention. |
|
 |
| Index finger injury |
Injury to the index finger, (also
referred to as forefinger, pointer finger, trigger finger, digitus secundus, digitus II, and many other terms), is the first finger and the second digit of a human hand. |
|
Strap incorporating the index and middle
fingers provides
passive rom to the
index finger |
|
 |
| Intrinsic Plus Splint |
Known as the safe position for
hand splinting. The hand can be immobilized in this position for long periods of time without
developing as much stiffness as would occur if the digits were
positioned differently. |
Flexion of MPs to 90 degrees and extension at PIP and DIP. Interossei and lumbricals at their shortest. Common in
patients with RA. |
|
|
 |
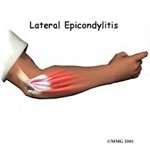
| Lateral epicondylitis |
CTD from degeneration of the
tendon origin as a result of
repetitive microtrauma; overuse of the wrist extensors, especially the ECRB; AKA tennis elbow |
Ice/deep friction massage, stretching, activity mod,
strengthening |
Elbow wrap/wrist
splint. The splint rests
the muscle and tendon and protects against pain with activity. |
|
 |
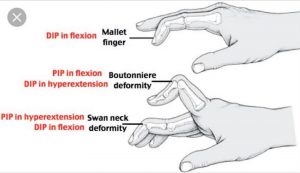
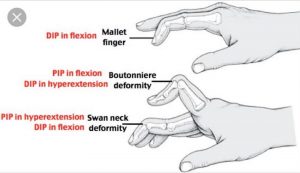
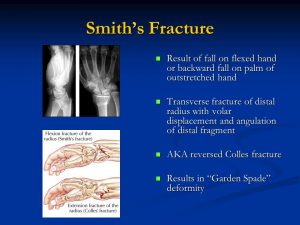
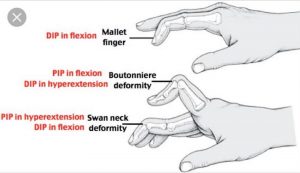
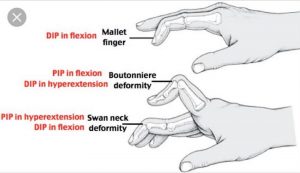
| Mallet Finger |
Avulsion of the terminal tendon |
First splint the patient’s DIP
joint in full extension
continuously for 6 weeks.
The DIP terminal tendon
is delicate and requires
continuous splinting to
prevent extensor lag of
the tendon. |
Splinted for 6 weeks. |
|
 |
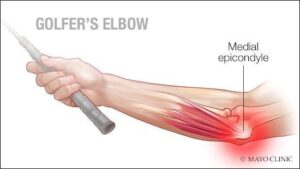
| Medial epicondylitis |
same as lateral epicondylitis,
but is overuse of wrist flexors;
AKA golfer’s elbow |
|
Elbow wrap/wrist splint |
|
 |
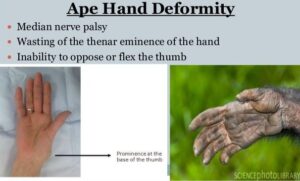
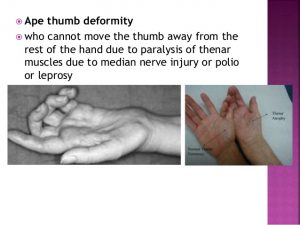
| Median Nerve Injury. |
Causes ape hand deformity.
Symptoms: ape hand deformity, sensory loss in index, middle, and radial side of ringer finger loss of pinch, thumb opposition,index finger MCP and PIP flexion; and decreased pronation. |
Post-surgical management:
AROM and PROM in
splint for digits and
thumb, tendon gliding
exercises, scar massage,
discontinue splint at 6
weeks and begin
strengthening exercises. |
Non-operative
treatment: Static
thenar web spacer
splint. Operative
treatment: dorsal wrist
blocking splint worn
for 4-6 weeks. |
|
 |
| Median nerve laceration |
– loss of thumb opposition, weak pinch; clawing of index/mid fingers for low level lesion Ape hand- flattening of thenar eminence of Hand of benediction- loss of thumb, index, and middle fingers; high level lesion |
A/PROM, scar management,
strengthening, sensory re-ed |
Dorsal protection
splint (30° wrist if low
lesion, 90° elbow at
elbow if high), C-Bar
splint to prevent thumb adduction contracture |
|
 |
| Median and Ulnar nerve injury |
Injury to both the median and
ulnar nerves result in an
impairment of function.
Can be caused by car accidents and glass injuries. |
|
Figure of eight splint to prevent MP
hyperextension or
dynamic MCP flexion
splint |
|
 |
| Metacarpal fracture |
|
|
Ulnar gutter splint |
|
 |
| MCP flexion limitation |
Difficulty flexing the MCP’s. The
metacarpophalangeal joints
(MCP) are of the condyloid kind,
formed by the reception of the
rounded heads of the
metacarpal bones into shallow
cavities on the proximal ends of
the first phalanges, with the
exception of that of the thumb,
which is a hinge joint. |
|
The correct angle of
pull for a finger loop is 90°. This angle of pull distributes the
pressure most evenly
to the proximal phalanx. |
|
 |
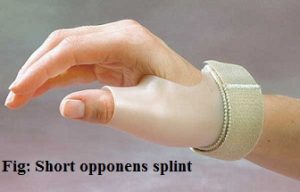
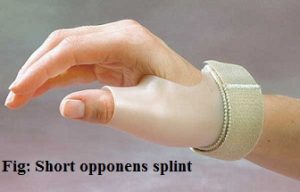
| Opponens splint |
For fist contracture |
|
|
|
 |
| Pronator teres syndrome |
A median nerve compression
between two heads of pronator
teres; symptoms same as CTS,
with also aching pain in proximal volar forearm |
|
Elbow splint at 90° (forearm in neutral), |
Avoid repetitive
forearm pronation/supination |
 |
| Proximal Fracture |
Metacarpal fracture, such as a
boxer’s (4th and 5th finger)
fracture |
|
|
|
 |
Proximal
interphalangeal
(PIP) flexion
contracture |
|
|
A prefabricated
dynamic PIP
extension assist splint will improve PIP extension and takes less therapy time to fit than to custom make this splint. |
|
 |
| Radial head fracture |
33% of elbow fractures.
Usually caused by a forceful load through an outstretched arm .
. |
Type 2 (displaced)
treated conservatively
with immobilization for 2-3
weeks and early motion
with medical clearance.
Type 3 (committed)
treated surgically, with
immobilization and early
motion within the first
post-surgical week as
medically prescribed. |
Type 1 (nondisplaced)
can be treated with a
long arm sling. A Type III fracture of the radial head requires removal
of the fragmented
bone and a cast for
3–4 weeks to ensure
proper healing and
support. |
|
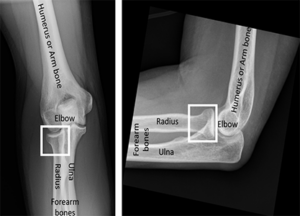 |
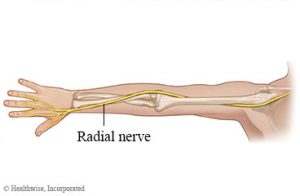
| Radial Nerve laceration |
Inability to ⁄ digits to release
objects; difficulty manipulating
objects |
ROM, sensory re-ed, home program, activity mod |
Dynamic ⁄ splint |
|
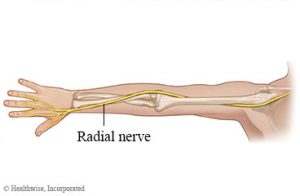 |
| Radial nerve palsy |
Radial nerve compression;
weakness/paralysis of extensors to wrist, MCPs, thumb; wrist drop; AKA Saturday night palsy.
Slow nerve regeneration. |
ROM, nerve gliding, strengthening |
Thumb Extension
Splint, Duran dorsal
protection splint, volar splint with wrist in neutral, dynamic ⁄
splint |
|
 |
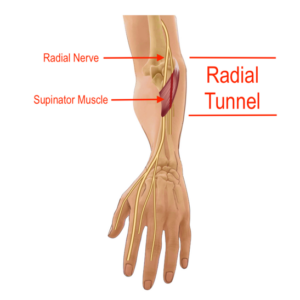
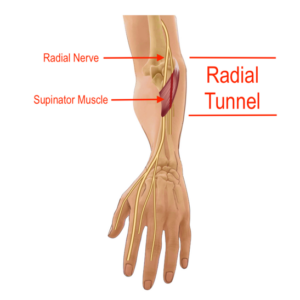
| Radial tunnel syndrome |
Compression of the radial nerve in the proximal forearm resulting in a dull ache and burning sensation along the lateral forearm. |
Post-surgical management: Long arm splint with the wrist in extension, elbow in flexion, and forearm in neutral rotation for 2 weeks, then wrist cock up for 2 more weeks, passive and active pronation and supination, hand strengthening exercise at 3 weeks, resistive exercise at 6 weeks. |
Non-operative: Long arm orthosis with the wrist in extension, elbow in flexion, and forearm in neutral rotation, massage or
TENS for pain
management, pain free ROM, nerve
gliding, activity
modification |
Avoid forceful wrist
extension and
supination
. |
 |
| Retts syndrome |
Under the broad category of
pervasive developmental
disorders, together with the
autism spectrum disorders.
Repetitive stereotyped hand
movements, such as wringing
and/or repeatedly putting hands into the mouth. |
Maintain the integrity of the skin such as dynamic elbow splints that inhibit a hand to mouth pattern by limiting full elbow flexion. |
|
|
 |
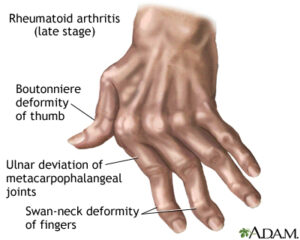
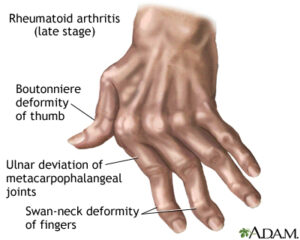
| Rheumatoid arthritis |
An autoimmune disease that results in a chronic, systemic inflammatory disorder that may affect many tissues and organs, but principally attacks flexible (synovial) joints. |
|
Volar in extension, up
to 30 degrees, based
on the person’s comfort level
-Ulnar drift close
to neutral |
|
 |
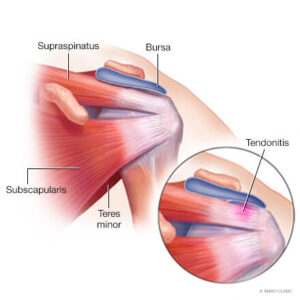
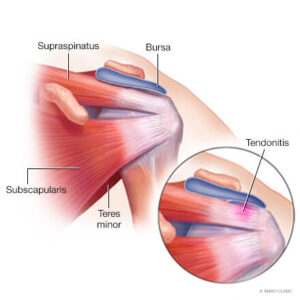
| Rotator cuff tendonitis |
Inflammation (irritation and swelling) of the tendons of the shoulder |
Activity mod, educate in sleeping posture (avoid arm overhead), pain management, strengthening |
Codman exercises/pendulum
exercises |
|
 |
| Serpentine Hand Splint |
It is used when the thumb is in palmar abduction and it allows
the thumb to move within abduction needed for opposition. Helps with muscle weakness for children with CP and it is important to use it
during functional activities |
|
|
|
 |
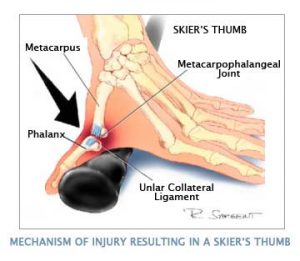
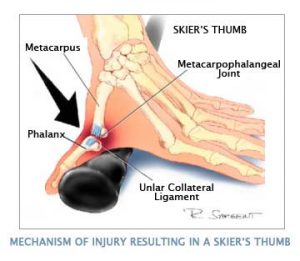
| Skier’s Thumb (Gamekeepers Thumb) |
Rupture of the ulnar collateral
ligament of the MCP joint of the thumb. (i.e., skiing with the
thumb held in a ski pole) |
AROM and pinch strength
at 6 weeks. ADL’s that
require opposition and pinch strength. PROM at 8 weeks and strengthening at 10 weeks. Wear all day and night. |
Thumb splint for 4-6 weeks |
Contraindicated: twisting a tight cap |
  |
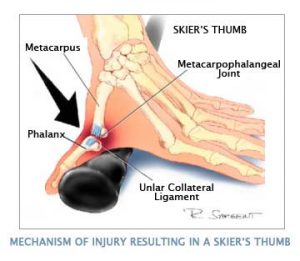
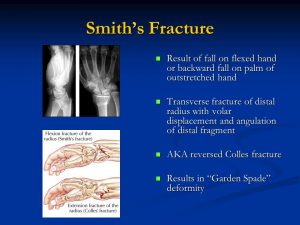
| Smith’s fracture |
Complete fracture of the distal
radius with volar displacement. |
Orthotics are used for
immobilization as needed.
ROM is begun early, within 1 week if medically cleared. A sling is used for type 1 fractures or comfort, if the patient has pain and is nervous in public places. |
Thumb splint |
|
|
| Spasticity |
Altered skeletal muscle
performance in muscle tone
involving hypertonia; it is also
referred to as an unusual
“tightness”, stiffness, or “pull” of muscles. |
|
Spasticity splint or cone splint |
|
 |
| Swan neck deformity |
Injury to the MCP, PIP, or DIP joints characterized by PIP hyperextension and DIP flexion.
Adaptive equipment |
|
Silver rings/tripoint
splint. PIP is splinted
in slight flexion, or
buttonhole splint |
|
  |
Tendinitis
/Tenosynovitis |
Inflammation of a tendon |
Treatment is largely
conservative with rest, and gradual return to exercise is a common therapy. Ice, compression and elevation. Initial recovery is typically within 2 to 3 days and full
recovery is within 4 to 6 weeks. Treatment of
tendinitis helps reduce some of the risks of developing tendonosis, which takes longer to heal. |
Duran dorsal protection splint, volar splint with wrist in neutral |
|
 |
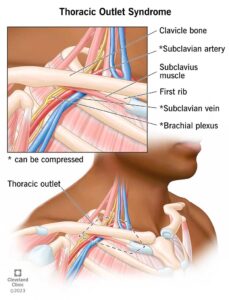
| Thoracic outlet syndrome |
Excess pressure placed on a
neurovascular bundle passing
between the anterior scalene
and middle scalene muscles |
|
|
|
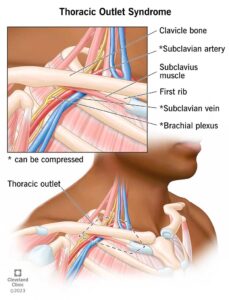 |
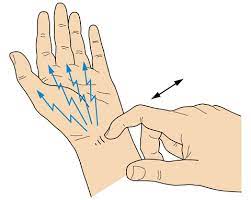
| Tinel’s Sign |
Tinel’s sign is a way to detect
irritated nerves. It is performed by lightly tapping (percussing) over the nerve to elicit a sensation of tingling or “pins and needles” in the distribution of the nerve. The Tinel sign is typically elicited by lightly percussing along the course of the affected nerve from distal to proximal. For example, in carpal tunnel syndrome where the median nerve is compressed at the wrist, Tinel’s sign is often “positive” causing tingling in the thumb, index, middle finger and the radial half of the fourth digit. Tinel’s sign is a generalized term, and can also be positive in ulnar nerve impingement at the wrist (Guyon’s canal syndrome), where it affects the other (ulnar) half of the fourth digit and the fifth digit. |
|
|
|
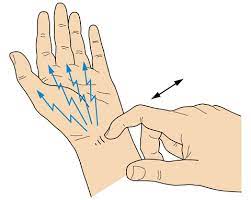 |
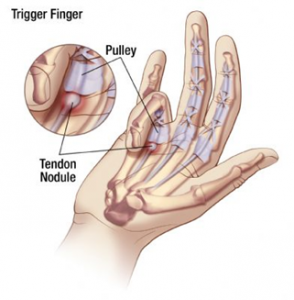
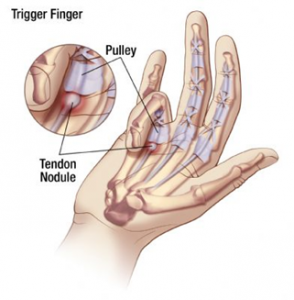
| Trigger finger |
CTD; tenosynovitis of the finger flexors; most common is A1 pulley. Trigger finger is a condition in which edema in the tendon and synovium of the digit results in lack of smooth flexion or extension of the finger. |
To rest the tendon and
prevent snapping as the tendon pulls through the
finger pulleys, the MCP
joint is blocked by splinting, then gentle pull through with bending and straightening of the distal and proximal
interphalangeal joints is
recommended 20 times every 2 hours while the patient is awake. Edema control, tendon gliding, activity/work mod
. |
Hand-based TF splint
(MCP ⁄DIP and PIP is
free), a splint to support the
metacarpophalangeal
joint in extension |
|
 |
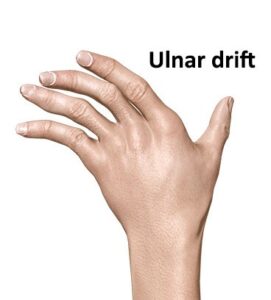
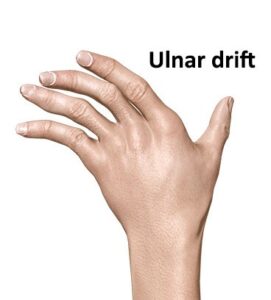
| Ulnar Drift |
Hand deformity in which the
swelling of the metacarpophalangeal joints (the big knuckles at the base of the fingers) causes the fingers to become displaced, tending towards the little finger. The hand, including the fingers, move towards the ulna. Ulnar deviation is a disorder in which flexion by ulnar nerve innervated muscles is intact while flexion on the median nerve side is not. |
|
|
|
 |
| Ulnar Nerve Injury |
Results in ulnar claw deformity and numbness of the ulnar side of the hand and the fifth and half of the fourth digits. See generalized weakness of the ulnar side of the hand and pain. Trouble cutting with small knife. Trouble with power grip and lateral pinch. |
Orthotics are used for
immobilization as needed.
ROM is begun early, within 1 week if medically cleared. A sling is used for type 1 fractures or comfort if the patient has pain and is nervous in public places. |
Ulnar nerve injury
splint, dynamic/static
splint to position MP’s
in flexion. MCP block
splint. If it is a low level ulnar nerve injury, use a splint that prevents
hyperextension of the
MCP joints and allows MCP flexion. |
|
 |
| Upper extremity weakness |
|
|
A deltoid sling . |
|
 |
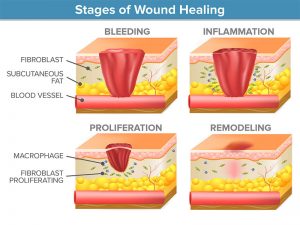
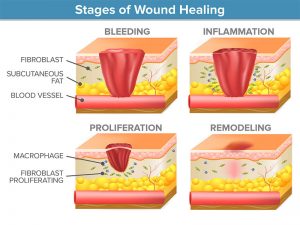
| Wound healing |
Occurs in phases that generally follow the process of
inflammation, proliferation, and
remodeling |
|
|
|
 |
| Wrist fracture |
Injury to the wrist. The wrist is
variously defined as the carpus
or carpal bones, the complex of
eight bones forming the proximal skeletal segment of the hand, the wrist joint or radiocarpal joint, the joint between the radius and the
carpus.
The wrist includes the distal parts of the bones of the forearm and the proximal parts of the five metacarpal bones. The series of joints between these bones are referred to as wrist joints. This region also includes the carpal tunnel, the anatomical snuff box, the flexor retinaculum, and the extensor retinaculum. |
Maximum passive extension up to 30 degrees. |
Duran dorsal protection splint, volar splint with wrist in neutral |
|
 |
| Wrist tendonitis |
Inflammation of the wrist |
Dexamethasone is the
most widely used medication by therapists using iontophoresis because of its anti-inflammatory properties. |
|
|
 |