DYSPHAGIA- FOCUS ON CP
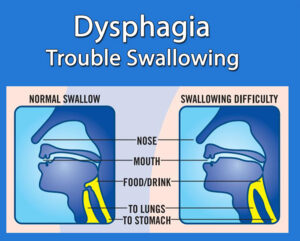
DYSPHAGIA
Dysphagia is a condition in which disruption of the swallowing process interferes with a patient’s ability to eat. It can result in aspiration pneumonia, malnutrition, dehydration, weight loss, and airway obstruction. The goals of dysphagia treatment are to maintain adequate nutritional intake for the patient while maximizing airway protection.
DEGLUTITION
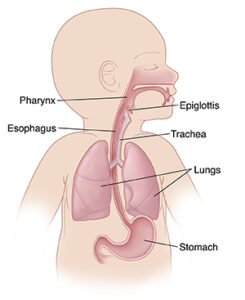
This is the act of swallowing, which allows a food or liquid bolus to be transported from the mouth to the pharynx and esophagus, through which it enters the stomach. Normal deglutition is a smooth, coordinated process that involves a complex series of voluntary and involuntary neuromuscular contractions and typically is divided into distinct phases: oral, pharyngeal, and esophageal. Each stage facilitates a specific function; if the stages are impaired, specific symptoms may result.
A. Oral phase
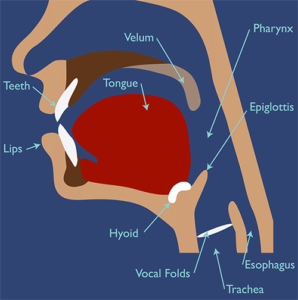
The oral phase of swallowing is divided into the following 2 parts:
I. Oral preparatory phase: The processing of the bolus to render it swallowable
II. Oral propulsive (or transit) phase: The propelling of food from the oral cavity into the oropharynx
B. Pharyngeal phase
The pharyngeal phase is of particular importance, because without intact laryngeal protective mechanisms, aspiration (the passage of food or liquid through the vocal folds) is most likely to occur during this phase. The pharyngeal phase of swallowing is involuntary and totally reflexive, so no pharyngeal activity occurs until the swallowing reflex is triggered.
C. Esophageal phase
In the esophageal phase, the bolus is propelled downward by a peristaltic movement. The lower esophageal sphincter relaxes at initiation of the swallow, and this relaxation persists until the food bolus has been propelled into the stomach. The sphincter closes after the bolus enters the stomach, thereby preventing gastroesophageal reflux.
SIGNS AND SYMPTOMS OF DYSPHAGIA
Signs and symptoms of oral or pharyngeal dysphagia include the following:
• Coughing or choking with swallowing
• Difficulty initiating swallowing
• Food sticking in the throat
• Sialorrhea- This is the unintentional loss of saliva from the mouth. This can be due to excessive production of saliva, lack of control of the lips and lack of lip closure (inadequate oral motor control).
• Unexplained weight loss
• Change in dietary habits
• Recurrent pneumonia
• Change in voice or speech (wet voice)- When food penetration or aspiration occurs, the mucous membrane covering the vocal cords is modified; this produces a change in the voice and is referred to as a “wet voice”. If the child is unable to speak, this wet voice is evident in their cry.
• Nasal regurgitation
Signs and symptoms of esophageal dysphagia include the following:
• Sensation of food sticking in the chest or throat
• Change in dietary habits
• Recurrent pneumonia
• Symptoms of gastroesophageal reflux disease (GERD)- including heartburn, belching, sour regurgitation
Other associated factors/symptoms of dysphagia include the following:
• General weakness
• Mental status changes
 Symptoms of aspiration
Symptoms of aspiration
• Coughing or wheezing during or right after eating
• Too much saliva
• Shortness of breath or tiredness while eating
• A wet-sounding voice during or after eating or drinking
• Fever 30 to 60 minutes after eating
** Stay upright for at least 30 minutes after eating, this can help reduce the risk for aspiration.
DIAGNOSIS OF DYSPHAGIA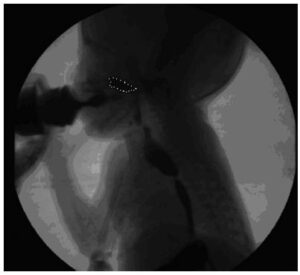
Since history and physical examination alone may not be adequate to make a diagnosis in cases of silent aspiration, additional diagnostic tests, such as video fluoroscopy may be indicated.
MANAGEMENT OF PEDIATRIC DYSPHAGIA
Cognitive, developmental, and behavioral issues can affect the treatment options. Treatment does not necessarily imply feeding therapy. Tone abnormalities, postural control, adverse behavior, and primitive reflexes may need to be managed. Hypoxemia can occur while a child with dysphagia eats, so pulse oximetry during mealtime can be useful.
..
FEEDING A CHILD WITH CP 
Considerations:
1. Type of food (liquid, porridge, whole) that the child ingests and the feeding method (mouth, nasogastric probe or mixed route).
2. Food utensil to be used, usually a small metallic spoon (tea), which is not larger than the child’s tongue. If there is a strong bite, use a plastic spoon that is strong or a metal spoon that is coated. An adapted spoon can also be used if the child has the physical skills to use it.
3. Posture before and during the feeding process.
4. The way of approaching the spoonful of food, which must always enter from the bottom up and in front of the child. This favors anticipation of the food process.
** A common precaution is to fill the spoon with food only halfway.
Intervention:
Treatment selection will depend on the child’s age, cognitive and physical abilities, and specific swallowing and feeding problems.
Goal: Protect the airway and offer safer transit of food and liquid
1. Postural and Positioning Techniques 
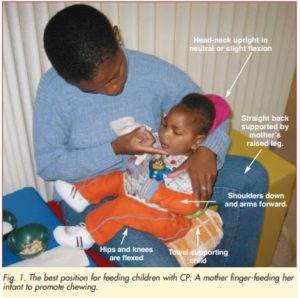
Postural and positioning techniques involve adjusting the child’s posture or position before and if necessary, during feeding. The general goal is to establish central alignment and stability for safe feeding.
• Use of preparation techniques to normalize abnormal tone and to develop more normal pattern of movements
• Use of adequate seating equipment and/or handling techniques to maintain head/trunk alignment and in an upright positon
• Slight chin tuck and elongation of the back of the neck, positioned in midline
• Provide adequate symmetric postural stability – stable base of support for bottom and trunk, hip symmetrically flexed at around 90°, tray to support arms and headrest to support neck
• Arms forward and resting comfortably on the tray or table
• Feet resting on a firm surface
• Cheek and jaw support as needed
2. Diet Modifications
Diet modifications consist of altering the viscosity, texture, temperature, portion size, or taste of a food or liquid to facilitate safety and ease of swallowing.
Typical modifications may include:
• Thickening thin liquids
• Pureeing solid foods
• Temperature of a food may be altered to provide additional sensory input for swallowing
3. Equipment and Utensils 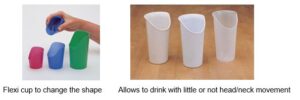

Adaptive equipment and utensils may be used with children who have feeding problems to foster independence with eating and increase swallow safety by controlling bolus size or achieving the optimal flow rate of liquids.
Examples of adaptive equipment include:
• Modified nipples
• Cut out cups (Nosey Cup)
• Coated spoon if tonic bite not inhibited
• Weighted forks and spoons
• Angled forks and spoons
• Sectioned plates
• Non-tip bowls
• Dycem® to prevent plates and cups from sliding
** The choice of adapted cutlery depends on the type of CP.
4. Strategies for Tonic Bite and Tongue Thrust
•Tonic Bite
A tonic bite reflex is an automatic, sustained jaw closure, accompanied by increased abnormal tone in the jaw muscles. For those who have a tonic bite reflex, mealtimes can be extremely challenging. It is difficult to release, and its force can damage the teeth, or the object that has been placed in the mouth. It can be caused by hypersensitivity of the mouth, the oral cavity, or surrounding area of the face. Additionally, seeing a spoonful of food approaching their mouth can trigger a tonic bite reflex for some children. Because the spoon is clamped in the child’s mouth and they are unable to let go of it, the person feeding them may attempt to remove it before the involuntary jaw closure is released. They may attempt this by either pulling it straight out of the mouth, or by wiggling it from side to side to get it out of the mouth and, in both cases, this may be painful or damage tissue in or around the mouth. The caregiver must learn to be patient with individuals who have a tonic bite reflex. The tonic bite increases if the item is pulled on.
Guidelines
• It is extremely important that the environment is quiet and calm and does not over stimulate the child
• Use a coated flat spoon. Avoid plain metal or light plastic spoons
• Present the cup or spoon on the child’s lower lip
• NEVER try to pull the cup or spoon out of the child’s mouth while their reflex is still active
• When the child is biting down, apply light pressure on the bottom of their chin. Wait to feel their jaw drop and then remove the spoon or cup from their mouth. If this does not help, gently guide the child’s chin to chest as this is a way to naturally open the mouth and release the utensil or cup.
•Tongue Thrust
During eating, a tongue thrust will work against the intake of food. Instead of being part of the process of bringing food into the mouth, the tongue extends during the intake of food, pushing the food out of the mouth.
Guidelines
• Place a level spoon on the center of the tongue and apply firm downward pressure while offering firm pressure under the chin using your finger
• Place a cup on the lower lip below the tongue while offering firm pressure under the chin (to the tongue)
• Thicken liquids
Feeding Strategies:
Pacing
Feeding strategies for children may include alternating bites of food with sips of liquid or swallowing. For infants, pacing can be accomplished by limiting the number of consecutive sucks. Strategies that slow the feeding rate may allow for more time between swallows to clear the bolus and may support more timely breaths.
Compensatory techniques
Maintaining oral feeding often requires compensatory techniques to reduce aspiration or improve pharyngeal clearance.
These include the following:
• Use of the chin-tuck position
• Rotation of the head to the affected side
• Tilting of the head to the strong side
• Lying on one’s side or back during swallowing
• Supraglottic swallow- vocal folds are usually closed by voluntarily holding breath before and during swallow in order to protect the airway.
• Bolus-clearing maneuvers
• Enteral feeding
• Nasogastric tube (NGT) feeding
• Oroesophageal tube feeding
• Percutaneous endoscopic gastrostomy (PEG)
..
THE DYSPHAGIA DIET
The National Dysphagia Diet (NDD),aims to have standard terminology and practice applications of dietary texture modification in dysphagia management.
The dysphagia diet framework consists of eight levels (0-7) and includes both foods and liquids on a single continuum. Drinks/liquids are measured from Levels 0-4, while foods are measured from Levels 3-7.
Drinks – Levels 0 to 4
Level 0 (thin). These are watery liquids such as juice, tea, milk, soda, beer, and broth. You can drink them through a nipple, cup, or straw.
Level 1 (slightly thick)
These are thicker than water. They require more effort to drink than thinner liquids but still flow through a straw or nipple.
Level 2 (mildly thick)
These liquids flow off a spoon but more slowly than thinner drinks. They can be sipped or sucked from a straw with some effort.
Level 3 (liquidized, moderately thick)
You can drink these from a cup or sucked from a straw with some effort. These are liquids that may be thick enough to be eaten with a spoon An example is a thick milkshake. Their texture is smooth without lumps.
Level 4 (pureed, extremely thick)
These are usually eaten with a spoon. You can’t drink them from a cup. An example is pudding.
Food – Levels 3 to 7
Level 3 (moderately thick)
These are foods that:
Don’t require chewing
Have a smooth texture but are not lumpy
Can be eaten with a spoon, but not with a fork
Are not thick enough to stand stiff on a plate. For example, not stiff like molded gelatin.
Level 4 (pureed, extremely thick)
These foods:
– Can often be eaten with a spoon, but sometimes a fork
– Can’t be drunk from a cup
– Don’t need to be chewed
– Can be molded, such as gelatin
– Are not sticky or lumpy
– Fall off a spoon all together when tilted and still hold shape on a plate. For example, pudding.
– Can’t be poured but move very slowly if the plate is tilted
Level 5 (minced, moist)
These foods:
– Can be eaten with a fork or spoon, or a chopstick if you have good hand control
– Can be scooped and shaped on a plate. For example, mashed potatoes.
– Are soft and moist but don’t separate into liquid
– May have small lumps that can be mashed with the tongue
Level 6 (soft)
These foods:
– Are tender, moist, and bite-sized
– Can be eaten with a fork, spoon, or chopsticks but don’t need a knife to cut
– Must be chewed
Level 7 (regular)
These are:
– Normal, everyday foods of varying textures, including soft, stringy, and hard and crunchy
– Foods that can be eaten by any method. For example, from a cup or using utensils.
– Foods that need to be chewed, with all types of textures and may have pieces that can’t be swallowed, such as gristle.
Take note:
** Level 3 includes moderately thick liquids and liquidized foods, which share similar characteristics and descriptions.
** Level 4 includes extremely thick liquids and pureed foods, which share similar characteristics and descriptions.
** Level 5 contains minced particle sizes of 4mm, which happens to be the size of food particles after chewing and are “swallow-ready” so this diet requires minimal chewing.
*For pediatrics, they suggest 2 mm particle size.
** Level 6 contains bite sizes that are 1.5cm or 15mm, so that if a chunk falls into the airway, the person will not choke/asphyxiate. The size of 15mm is about the size of an adult thumbnail, and is smaller than the typical adult airway.
* For pediatrics, the chunk size should be no larger than 8mm or the size of the child’s fingernail on their little finger.
Summary of Dysphagia Diet
Dysphagia diet 1: Thin liquids (eg, fruit juice, coffee, tea)
Dysphagia diet 2: Nectar-thick liquids (eg, cream soup, tomato juice)
Dysphagia diet 3: Honey-thick liquids (ie, liquids that are thickened to a honey consistency)
Dysphagia diet 4: Pudding-thick liquids/foods (eg, mashed bananas, cooked cereals, purees)
Dysphagia diet 5: Mechanical soft foods (eg, meat loaf, baked beans, casseroles)
Dysphagia diet 6: Chewy foods (eg, pizza, cheese, bagels)
Dysphagia diet 7: Foods that fall apart (eg, bread, rice, muffins)
Dysphagia diet 8: Mixed textures
Resources:
https://emedicine.medscape.com/article/2212409-overview
https://www.asha.org/PRPSpecificTopic.aspx?folderid=8589934965§ion=Treatment
http://www.appstate.edu/~clarkhm/pediatric/pedout5.htm
https://www.fairview.org/patient-education/90424
https://dietitiansondemand.com/a-clinical-dietitians-guide-to-iddsi/
https://www.physio-pedia.com/Feeding_the_Child_with_Cerebral_Palsy