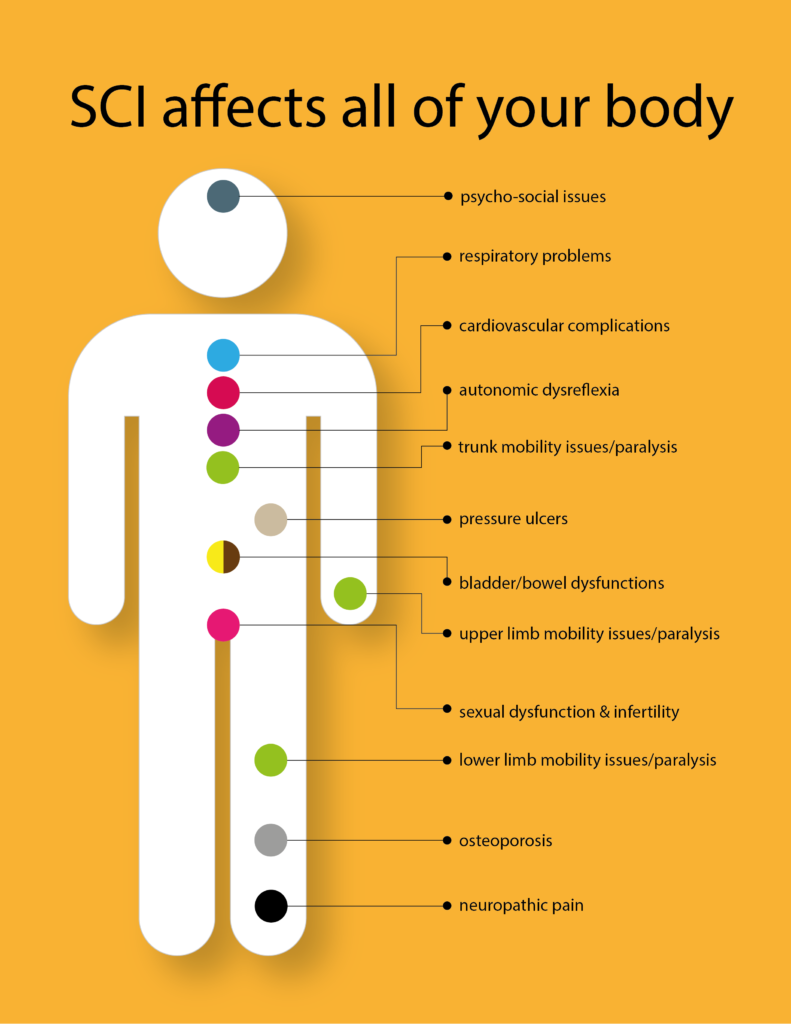
Complications of Spinal Cord Injury
………………… …….
| Complication | Description | Cause | Symptoms | Intervention |
| Orthostatic Hypotension (OH)
Also known as Postural Hypotension
|
Usually seen in both acute and chronic stages following SCI. Characterized as a drop in blood pressure that occurs when a person stands up from sitting or lying down. Defined as a decrease in systolic blood pressure of 20 mmHg or more, or a reduction in diastolic blood pressure of 10 mmHg or more, when the body position changes from supine to upright, regardless of whether symptoms occur. | The autonomic nervous system responds to changes in position by constricting veins and arteries and increasing heart rate and cardiac contractility. | The symptoms associated with orthostatic hypotension include: • Dizziness • Light Headedness • Nausea • Headache • Pallor • Yawning • Sweating • Muscle weakness • Fatigue • Occasionally syncope (temporary loss of consciousness) |
The goal of treatment for orthostatic hypotension is to restore normal blood pressure. That usually involves increasing blood volume, reducing the pooling of blood in the lower legs and helping blood vessels to push blood throughout your body.
Management of OH includes application of pressure stockings and abdominal binders, adequate hydration, gradual progressive daily head-up tilt, and administration of pharmacological agents. For an acute episode: The patient must be reclined quickly and, if sitting in a wheelchair, should be tipped back with legs elevated until symptoms subside. With time, this problem can diminish as sitting tolerance and level of activity increases |
| Autonomic Dysreflexia (AD) | AD is a well-known medical emergency. AD may appear any time after a SCI but is a characteristic of the chronic stage. It generally occurs in patients with a SCI at levels of T6 and above. It is more common in patients with cervical and complete lesions. | AD is caused by spinal reflex mechanisms initiated by a noxious stimulus entering the spinal cord below the level of injury. The excessive parasympathetic activity (and lack of sympathetic tone) leads to vasodilation above the level of the lesion resulting in acute, uncontrolled hypertension. Bladder distension is the most common triggering factor for AD. The distension can result from urinary retention or catheter blockage. The second most common triggering for AD is bowel distension due to fecal impaction. Other potential factors include hemorrhoids and anal fissures, gastrointestinal precipitants (appendicitis, cholecystitis, etc.), pressure ulcers, ingrown toenails, heterotopic ossification, fractures, menstruation, pregnancy or labor, deep vein thrombosis, pulmonary embolism and sexual activity. | Signs of AD include: • High blood pressure • Pounding headache • Flushed face • Sweating above the level of injury • “Goose bumps” below the level of injury • Nasal stuffiness • Nausea • Slow pulse (slower than 60 beats per minute).An individual with a SCI above T6 often has a normal systolic blood pressure in the 90-110 mm Hg range- comparatively low resting blood pressure. A blood pressure reading of 20mm to 40mm Hg above their baseline may be a sign of autonomic dysreflexia. |
The management goals are normalization of heart rate and blood pressure and improving the symptoms of AD. An important part of the successful management of AD is prevention. Education of the patient, caregivers and family members regarding autonomic dysreflexia is vital to prevent AD and to recognize its occurrence without delay.
If AD occurs: 2. Next, loosen any tight clothing and/or constrictive devices / splints / braces-especially around the torso and quickly check the catheter for blockages. 3. Closely monitor BP. 4. Search for and eliminate the precipitating stimulus. This involves careful inspection to identify the source of painful stimuli. Remember: “The Five B’s” The occupational therapist must be aware of symptoms and treatment because autonomic dysreflexia can occur at any time after the injury. Individuals who are susceptible to this condition are encouraged to carry an emergency card describing the condition and treatment because many emergency rooms and medical personnel may be unfamiliar with it. |
| Pain Syndromes | Chronic pain is one of the frequent secondary complications for individuals with SCI. Chronic pain may lead to functional disability and emotional discomfort and may impact negatively on community participation and quality of life. The International Association for the Study of Pain has proposed 2 types of pain related to SCI: nociceptive (musculoskeletal or visceral) and neuropathic (either above level, at level or below level of injury). |
Nociceptive pain After SCI, chronic musculoskeletal pain may occur with: – Abnormal posture, gait and overuse of structures such as the arm and shoulder. For example, using a manually operated wheelchair increases the risk of developing shoulder pain. . -Carpal tunnel syndrome and ulnar nerve entrapment at the cubital tunnel and Guyon canal are also seen. . -Muscle spasm pain is another type of musculoskeletal pain that is often seen in patients with incomplete SCI. . Neuropathic pain Neuropathic pain can occur above the level, at the level or below the level of injury. Above the level neuropathic pain may arise from complex regional pain syndromes and compressive mononeuropathies. |
Neuropathic pain often presents diffusely caudal to the level of SCI. It is generally characterized as a burning, aching, tingling or stabbing sensation. | The use of simple analgesics, non-steroidal anti-inflammatory drugs and opioids are frequently used to treat patients with musculoskeletal pain after SCI.
Neuropathic pain relief in patients with SCI can be complex and requires a multifaceted approach. Medications, surgical interventions, the use of modalities and psycho-therapy are included in this approach. |
| Pressure Ulcers | Pressure ulcers are an important and potentially life-threatening secondary complication of SCI. They can lead to further functional disability and fatal infections and surgical interventions can be required. Pressure ulcers have been defined as a localized injury to the skin and/or underlying tissue, usually over a bony prominence, as a result of pressure or pressure in combination with shear. | Sensory loss increases the risk of skin breakdown. Individuals with sensory loss cannot feel the pressure and shearing of prolonged sitting or lying in one position or the presence of pain or heat against the body. Pressure causes the loss of blood supply to the area, which can ultimately result in necrosis.
Risk factors for pressure ulcers are immobility, reduced activity, lack of sensation, moisture due to urinary and fecal incontinence, muscle atrophy, prolonged time since injury, depression, smoking and poor nutrition. |
Most common locations for pressure ulcers after SCI are the ischium, trochanters, sacrum, heel, malleolus and feet. | Prevention of pressure ulcers begins at the time of injury and is a lifelong commitment for those living with SCI or their caregivers. • Pressure ulcer management includes daily inspection of skin, keeping skin clean and dry, avoidance of excessive pressure or shearing, proper pressure relief techniques, individually prescribed equipment (e.g., wheelchair cushions), well-balanced nutrition, early recognition and treatment. • Management of tissue loads- bed positioning, using pressure-reducing bed and wheelchair support surfaces, addressing postural alignment. • Electrical stimulation, ultrasound/ultraviolet light C and non-thermal pulsed electromagnetic energy treatment can be used as adjunctive therapies to standard wound management. |
| Urinary Complications | SCI may lead to disturbances of the urinary system. It causes bladder dysfunction, often referred to as the neurogenic bladder. As with other complications, urological dysfunctions after SCI also increase the risk of long-term complications and decreased psychological and social well-being of the patient. | Regular monitoring and suitable management for bladder dysfunction are important to prevent long-term complications (e.g., infections, vesicoureteral reflux, renal failure, bladder cancer) and provide a better quality of life in patients with SCI. | ||
| Bowel Complications | Neurogenic bowel is a major problem in terms of physical and psychological aspects for people with SCI. A neurogenic bowel occurs when there is a dysfunction of the colon due to lack of nervous control. | There are various interventions used for management of bowel dysfunction in patients with SCI. The non-surgical treatment methods include high dietary fiber intake, abdominal massage, digital rectal stimulation, manual evacuation, oral laxatives, rectal suppository and other pharmacological agents (stool softeners, colonic stimulants, contact irritants, bulk formers) and functional electrical and magnetic stimulation of skeletal muscles. | ||
| Spasticity | Spasticity is a common secondary impairment after SCI characterized by hypertonus, increased intermittent or sustained involuntary somatic reflexes (hyperreflexia), clonus and painful muscle spasms. Spasticity is an involuntary muscle contraction below the level of injury that results from lack of inhibition from the brain. Patterns of spasticity change over the first year, gradually increasing in the first 6 months and reaching a plateau about 1 year after the injury. Spasticity affects 70% of patients with SCI and causes considerable disability for many. | The pathogenesis of spasticity in patients with SCI remains uncertain. A possible cause may be an alteration in the excitability of various supraspinal inhibitory nerve. | Although spasticity has often been viewed as a factor that can negatively affect functional level after SCI, light to moderate spasticity may have a positive impact on functional activities, including standing, transfers and ambulation. Additionally, it contributes to better peripheral circulation, thereby avoiding edema and reducing the risk of deep vein thrombosis.
• A moderate amount of spasticity can be helpful in the overall rehabilitation of the patient with an SCI. It helps to maintain muscle mass, assists in the prevention of pressure sores by facilitating blood circulation, and can be used to assist in range of motion (ROM) and bed mobility. • A sudden increase in spasticity can alert the individual to other medical problems, such as bladder infections, skin breakdown, and fever. • Severe spasticity may contribute to increased functional impairment, contractures, ulcers, posture disorders and pain. |
Management options of spasticity involve the elimination of exacerbating factors (such as urinary tract infection, constipation, ingrown nails, pulmonary infection, pressure ulcers, etc.) and the use of physical agents (heat, cold) and physical techniques, electrical stimulation and surgical interventions. Surgical approaches include many orthopedic procedures (e.g., tendon extension, tendon plasty or osteotomy) and the ablation of motor nerves and/or rhizotomy of sensory spinal roots. Surgical treatment of spasticity leads to irreversible changes and can often be avoided if other methods are used at an early stage. Commonly used antispastic medications are baclofen, tizanidine, botulinum toxin, benzodiazepine, dantrolene sodium, gabapentin and pregabalin |
| Osteoporosis and Bone Fractures | Osteoporosis, a condition characterized by low bone mass and deterioration of the skeletal microarchitecture, is a well-known complication of SC. It occurs rapidly in the first 12-18 months post injury but continues for several years | Bone loss after SCI leads to increased risk of low impact fractures (those occurring spontaneously or from a transfer from bed to chair). A number of factors appear to have an influence on bone mass in patients with SCI. The level of the lesion, the extent of functional impairment, muscular loading of the bones, the duration of injury and aging are included in these factors. | The most common fracture sites are around the knee, such as the distal femur or proximal tibia. | There is generally no standardized treatment guidelines for management of osteoporosis in patients with SCI.
Non-pharmacological treatment methods such as standing-up, orthotically aided walking, weight – bearing physical exercises, functional electrical stimulation and pulsed electromagnetic fields have been trialed. |
| Decreased Vital Capacity | Reduced vital capacity affects the overall endurance level for activity. Prevalent with cervical and high thoracic lesions. | These individuals have markedly limited chest expansion and a decreased ability to cough because of weakness or paralysis of the diaphragm and the intercostal and latissimus dorsi muscles. This can result in recurrent respiratory tract infections. | Endurance can be improved by assisted breathing and by vigorous respiratory and physical therapy. Strengthening of the sternocleidomastoids and the diaphragm, manually assisted cough, and deep breathing exercises are essential to maintain optimal vital capacity. |
Resources:
Chronic complications of spinal cord injury. World J Orthop. 2015 Jan 18; 6(1): 24–33. (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4303787/)
Pedretti’s Occupational Therapy – E-Book (Occupational Therapy Skills for Physical Dysfunction)