SPLINTING MATERIALS

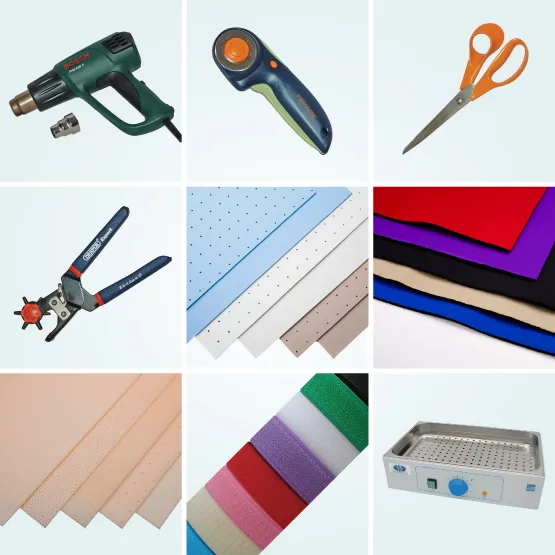
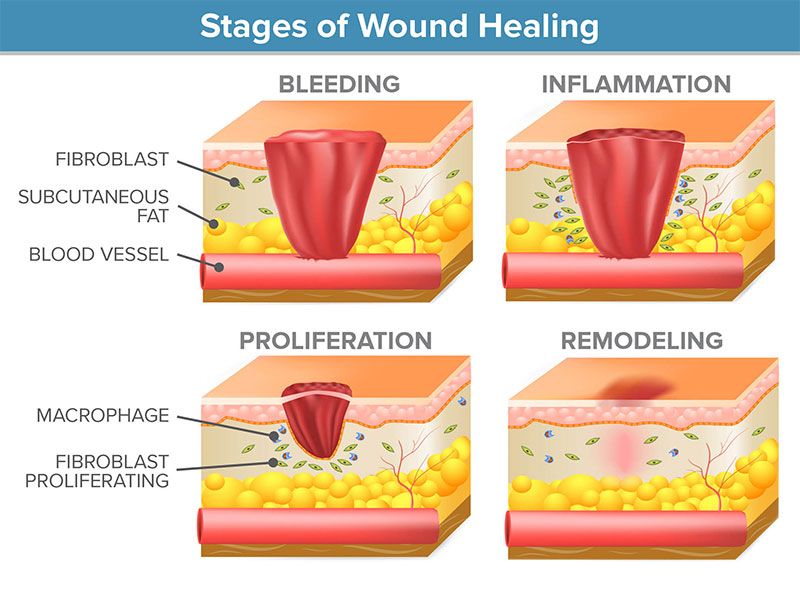
THE IMPORTANCE OF UNDERSTANDING TISSUE HEALING
Orthotic intervention directly correlates with the phases of tissue healing- consider the time frames for both soft-tissue and bone healing.
1. Acute Inflammatory Phase
During the acute inflammatory phase, tissues should be positioned for support and rest using orthoses that immobilize.
2. Proliferative Phase
During the proliferative phase, active motion may be initiated in this phase and the focus of orthotic intervention is continued protection of soft-tissue structures and their associated repairs while allowing for intervals of active exercises. During this phase, orthoses might be used to restrict joint motion in specific directions while allowing motion in other directions. And, periodically, the orthosis might be modified for improved positioning during this phase.
3. Maturation Phase
During the maturation phase, you will begin to encourage your patients to move more, increase their participation in functional activities, and add movement against resistance. Orthotic interventions during this phase might address limitations in joint motion. Orthoses for mobilization are typically introduced during the maturation phase of healing to encourage and promote movement, tissue remodeling, and collagen realignment. These types of orthoses are particularly helpful when joints are stiff or soft tissues are shortened from lack of motion.
Remember to monitor the patient’s extremity. You may elect to revise or maintain the orthotic intervention based on what you observe during the healing process. Do not make changes based solely on the calendar, but on your assessment of the patient’s needs.
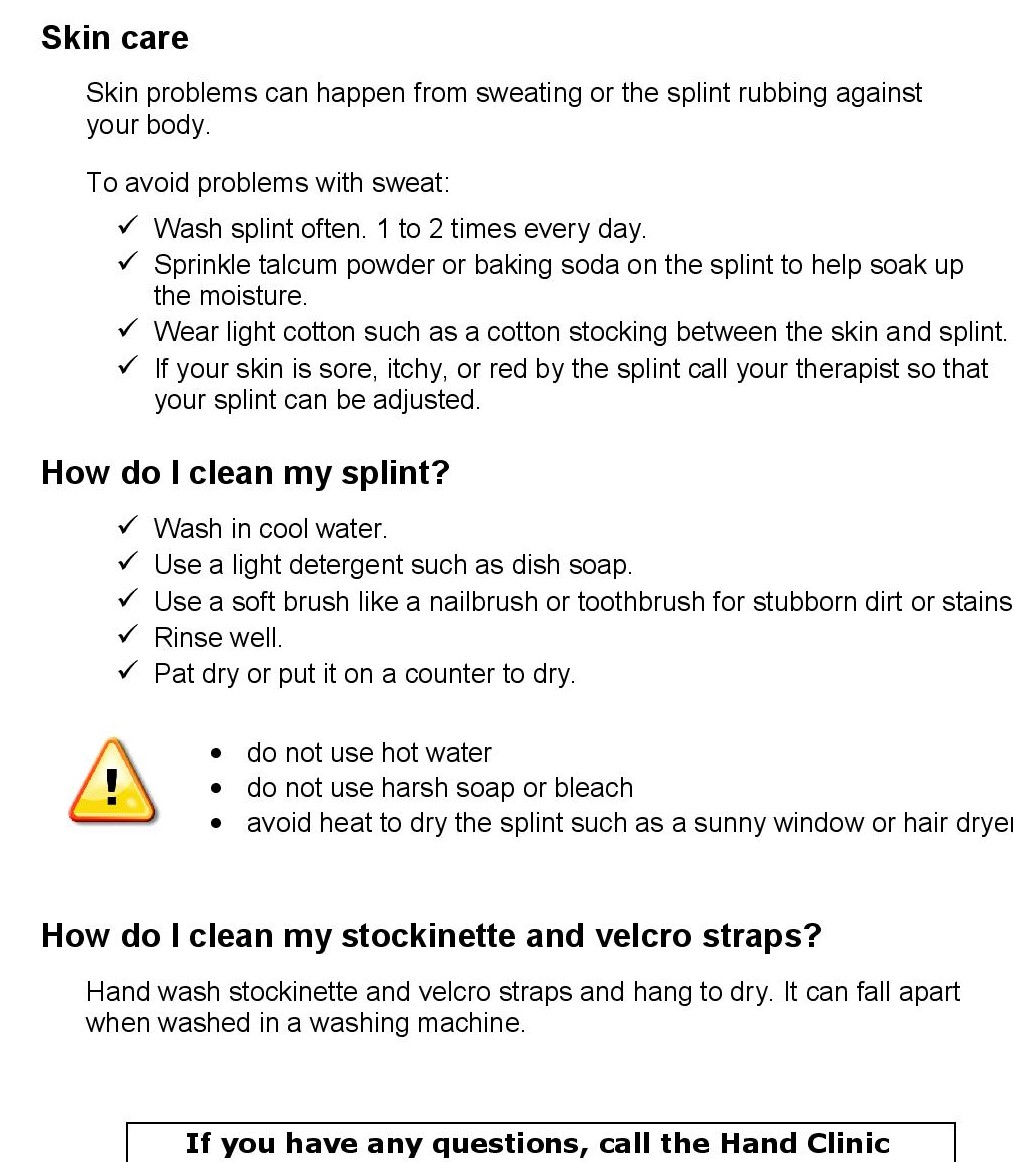
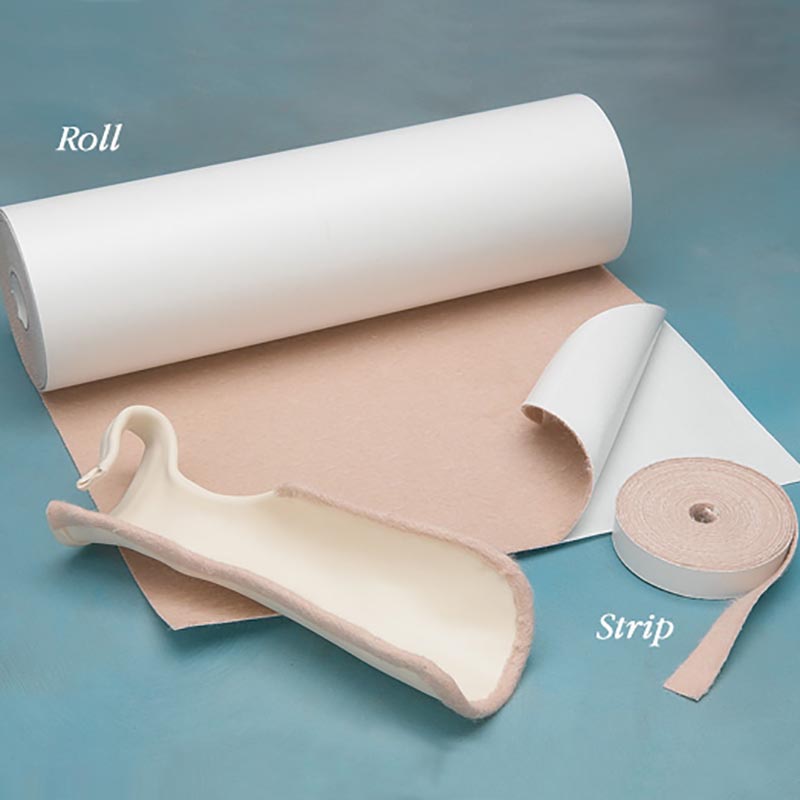
SPLINTING MATERIALS 
Low-temperature thermoplastic (LTT) materials are the most commonly used to fabricate splints. The materials are considered “low temperature” because they soften in water heated between 135° and 180°F and the OT practitioner can usually safely place them directly against a person’s skin while the plastic is still moldable. When LTT is heated, it becomes pliable, and then hardens to its original rigidity after cooling. Successful molding requires OT practitioners to refrain from pushing the material during shaping. Instead, the material should be lightly stroked into place. Light touch and constant movement of the OT practitioners’ hands will result in splints that are cosmetically appealing.
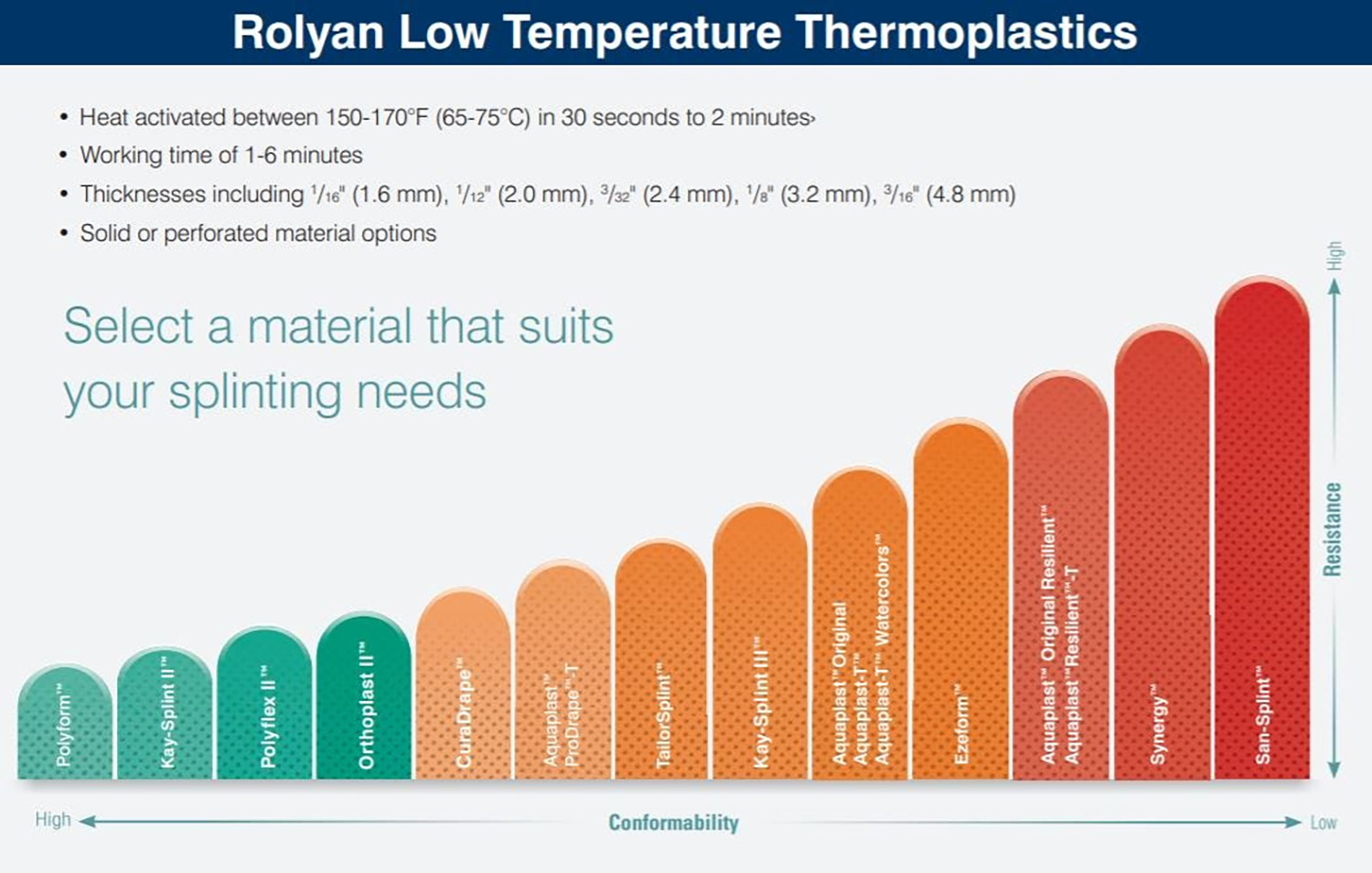
Thermoplastic Options
• Thickness
• Solid vs. Perforations
• Bonding – Uncoated vs. Coated
• Conformability vs. Resistance
Characteristics of Splinting Material
| Property/Characteristic | What it Means | Intended Use |
| Rigidity
|
The strength of the material. Materials that have a high degree of rigidity are strong and resistant to repeated stress.
|
High rigidity is necessary for large splints, specific diagnoses such as spasticity, and splints projecting large forces Rigidity is especially important when OT practitioners make medium to large splints (such as splints for elbows or forearms). Large splints require rigid material to support the weight at larger joints. In smaller splints, rigidity is important if the plastic must stabilize a joint. |
| Memory
|
Ability of the material to return to its original size and shape after being stretched. Materials with 100% memory will return to their original size and thickness when reheated. Most materials with memory turn translucent (clear) during heating. Using the translucent quality as an indicator, the OT practitioner can easily determine that the material is adequately heated and can prevent over or underheating. The ability to see through the material also assists the OT practitioner to properly position and contour the material on the patient.
|
Memory allows OT practitioners to reheat and reshape splints several times without the material stretching excessively. This is an important concept when frequent remolding of the splint will be necessary, as in serial splinting to increase extension or flexion over time. Memory makes the material more cost efficient.
|
| Conformability/Drapability | Drapability is the degree of ease with which a material conforms to the underlying shape without manual assistance- The way the material conforms to the shape of the hand.
|
Materials with high drapability work best with gentle handling as they conform easily to the arches or bony prominences. Materials with low drapability require firm handling and are recommended for larger splints where this moldability is less important. Successful molding requires OT practitioners to refrain from pushing the material during shaping. Instead, the material should be lightly stroked into place. Light touch and constant movement of OT practitioners’ hands will result in splints that are cosmetically appealing. Materials with low drapability require firm pressure during the molding process. Therefore, persons with painful joints or soft-tissue damage will better tolerate materials with high drapability. |
| Resistance to stretch
|
The amount of resistance the material gives to being stretched when heated | High resistance means you must work slowly and steadily to stretch the material. Low resistance to stretch means you need to work more quickly and carefully control the material as it stretches. Materials with a high resistance to stretch can be worked more aggressively than materials that stretch easily. As a result, resistance to stretch is a helpful property when one is working with uncooperative persons, those with high tone, or when one splint includes multiple areas |
| Coating
|
Materials that are coated always require surface preparation with a bonding agent or solvent i.e. Thermoplastic materials have a coating that must be removed for bonding to occur. Self-bonding (uncoated) materials may not require surface preparation. | Coated materials do not bond easily to attachments without having the coating removed. Non-coated materials have very good bonding to themselves and other attachments.
Uncoated |
| Perforations | Various perforation patterns are available (e.g., mini-, maxi-, and micro-perforated). Perforations in the material allow for air exchange to the underlying skin. | Perforated materials are designed to reduce the weight of splints.
Perforated material should not be stretched because stretching will enlarge the holes in the plastic and thereby decrease its strength and pressure distribution. When cutting a pattern out of perforated material, OT practitioners should attempt to cut between the perforations to prevent uneven or sharp edges. If this cannot be avoided, the edges of the splint should be smoothed. |
Other Considerations
1. Heating time
The time required to heat thermoplastic materials to a working temperature should be monitored closely because material left too long in hot water may become excessively soft and stretchy. Thinner materials and those that are perforated heat and cool more quickly.
2. Color of the material:
– Darker-colored splints tend to show less soiling and appear cleaner than white splints.
– Colored splints are easily seen compared to white splints and, therefore, useful in preventing loss in institutional settings.
3. Thickness of the material:
– Thinner thermoplastic materials are commonly used for small splints and for arthritis and pediatric splints
– A high degree of flexibility can take stresses repeatedly. Flexibility is an important characteristic for circumferential splints because these splints must be pulled open for application and removal.


 SAFETY FIRST
SAFETY FIRST
Orthotic fabrication involves working with heat and sharp tools. Both require extreme caution and supervision around patients. This is especially important when children or cognitively impaired people are nearby.
– Tools such as utility knives and scissors should not be left unattended on the table or countertop. Heat guns should be pointed away from people and objects when on, and should never be left running unattended. Make sure to close splint pan lids when you walk away.
– Always check the temperature of heated material prior to placing it on your patient to prevent a burn or discomfort. Remember that the splinting material holds heat.
– Splinting materials shrink slightly as they cool. During the molding and cooling time, precautions should be taken to avoid a shrinkage-induced problem such as difficulty removing a digit from a circumferential component of a splint.
– Remember to preheat thicker materials prior to cutting to avoid injuring your hands from the force and strain that will be required to cut the material.
– Remember to use the principles of good body mechanics and ergonomics. When fabricating an orthosis on a patient, avoid leaning excessively over the table or awkwardly over the patient. These positions put a lot of strain on your back and neck.
* Always try to obtain easy access to the patient’s extremity.
* Use gravity to assist you in orthotic fabrication by letting the material rest on top of the extremity as opposed to holding it up and in place.
– Remember to round all corners of the orthosis and all corners of the straps. Besides giving the orthosis a finished look, it is important to prevent sharp and pointed edges from scratching your patient.
– Foam and adhesive-backed padding materials are available for placement inside the orthosis and are often applied for comfort over bony prominences. Make sure to stretch the thermoplastic surface to create space for padding. Adding padding without creating space for it will increase pressure on a bony prominence, which is exactly what you want to avoid.
COMPLIANCE
A well-made orthosis is the key to successful outcomes and improved compliance. The goals of the orthosis will only be met if the orthosis is worn according to plan.
1. It is essential to explain the purpose of the orthosis to your patients. Make sure your patients understand the benefits of wearing their orthosis as well as the risks of non-adherence.
2. Explain what activities are (not) allowed while wearing the orthosis.
3. Follow up with patients regularly to encourage their adherence to the prescribed treatment plan. Continue to check for a comfortable and well-fitting orthosis.
4. Allow the patient some say in the design and/or color of the orthosis.
5. Make sure they are aware of the wearing schedule and know the expected time frame for achieving results.
6. Document the patient’s agreement with the treatment plan and keep a record of the schedule in writing.
7. Have the patient keep a record of their wearing schedule at home.
Example of a splint wearing schedule